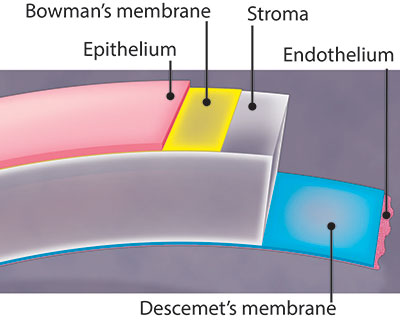
The cornea is the clear, front window of the eye. It helps focus light into the eye so that you can see. The cornea is made of layers of cells. These layers work together to protect your eye and provide clear vision.
Your cornea must be clear, smooth and healthy for good vision. If it is scarred, swollen, or damaged, light is not focused properly into the eye. As a result, your vision is blurry or you see glare.
If your cornea cannot be healed or repaired, your ophthalmologist may recommend a corneal transplant. This is when the diseased cornea is replaced with a clear, healthy cornea from a human donor.
A human donor is someone who chooses to donate (give) their corneas after their death to people who need them. All donated corneas are carefully tested to make sure they are healthy and safe to use.
There are different types of corneal transplants. In some cases, only the front and middle layers of the cornea are replaced. In others, only the inner layer is removed. Sometimes, the entire cornea needs to be replaced.
What Causes Corneal Problems?
Eye disease and injuries can damage the cornea. Here are some common eye problems that can lead to a damaged cornea:
- Keratoconus, where the cornea is cone-shaped rather than dome-shaped
- Fuchs’ dystrophy, where cells in the inner layer of the cornea are not working effectively
- Eye infections or injuries that scar the cornea
- Previous corneal surgery or other eye surgery that damaged the cornea
Corneal Transplant Surgery Options
Full thickness corneal transplant
Your entire cornea may need to be replaced if both the front and inner corneal layers are damaged. This is called penetrating keratoplasty (PK), or full thickness corneal transplant. Your diseased or damaged cornea is removed. Then the clear donor cornea is sewn into place.
PK has a longer recovery period than other types of corneal transplants. Getting complete vision back after PK may take up to one year or longer.
With a PK, there is a slightly higher risk than with other types of corneal transplants that the cornea will be rejected. This is when the body’s immune system attacks the new cornea tissue.
Partial thickness corneal transplant
Sometimes the front and middle layers of the cornea are damaged. In this case, only those layers are removed. The endothelial layer, or the thin back layer, is kept in place. This transplant is called deep anterior lamellar keratoplasty (DALK) or partial thickness corneal transplant. DALK is commonly used to treat keratoconus or bulging of the cornea.
Healing time after DALK is shorter than after a full corneal transplant. There is also less risk of having the new cornea rejected.
Endothelial keratoplasty
In some eye conditions, the innermost layer of the cornea called the “endothelium” is damaged. This causes the cornea to swell, affecting your vision. Endothelial keratoplasty is a surgery to replace this layer of the cornea with healthy donor tissue. It is known as a partial transplant since only this inner layer of tissue is replaced.
There are a few types of endothelial keratoplasty. They are known as:
- DSEK (or DSAEK) — Descemet's Stripping (Automated) Endothelial Keratoplasty
- DMEK — Descemet's Membrane Endothelial Keratoplasty
Each type removes damaged cells from an inner layer of the cornea called Descemet’s membrane. The damaged corneal layer is removed through a small incision. Then the new tissue is put in place. Just a few stitches—if any—are needed to close the incision. Much of the cornea is left untouched. This lowers the risk of having the new cornea cells being rejected after surgery.
Some things to know:
- With DSEK/DSAEK surgery, the donor tissue may be easier to transplant and position because it is thicker than the donor tissue in DMEK surgery.
- In DMEK surgery, the donor tissue is thin and can be more difficult to transplant. But, the recovery is quicker because the transplant tissue is thinner.
- Your eye surgeon will choose the type of surgery based on your cornea’s condition.
What to Expect When You Have a Corneal Transplant
Days or weeks before your transplant
Your ophthalmologist will talk with you about corneal transplant surgery. You will discuss why you need this surgery, how it can help you see better, and what you can expect during and after surgery.
Once you decide to have a corneal transplant, a date will be chosen for surgery. That date may change if a good donor cornea is not ready for you at that time.
Tell your ophthalmologist about all the medicines you take. They will tell you if you can keep taking them before surgery.
You may need to stop using blood thinners before surgery. You may need to visit your primary care doctor for a physical exam and perhaps other tests. This is to make sure you are healthy enough to have the transplant surgery.
You will not be able to drive after the transplant surgery. You should make arrangements for someone to drive you home after surgery.
The day of your transplant
A corneal transplant is done as an outpatient procedure.
Here is what will happen just before and during corneal transplant surgery.
- Eye drops will be put in your eyes. You may be given other medicine to help you relax.
- Your eye surgeon will use either local or general anesthesia so you do not feel pain. They will then put a device on your eye to keep it open. Even though your eye is open, you will see very little or nothing at all because of the anesthesia.
- Your eye surgeon will have chosen how to transplant the healthy donor cornea based on your specific need.
- In some cases, they may remove a circular part of your cornea and replace it with a matching portion of the donor cornea, stitching it into place.
- Sometimes they will remove only a very thin layer of cells from the front of the cornea, replacing them with donor tissue and stitching it into place.
- In other cases, only the damaged inner layer of the cornea is removed and a thin disc of healthy donor tissue is placed on the back surface of the cornea. An air bubble is then put in the eye to push this new cell layer into place so the cornea can heal properly.
- Sometimes your ophthalmologist may repair other eye problems during the same surgery, such as cataracts.
- After surgery, your ophthalmologist usually tapes a shield over your eye to keep it safely covered. You will be monitored after surgery to make sure you recover from the anesthesia and can go home safely.
- Your ophthalmologist will explain what to do to care for yourself at home after surgery.
After your transplant
The day after your corneal transplant surgery, you will need to go back to your ophthalmologist’s office to have your eyes checked.
The stitches from surgery may or may not need to be removed. This depends on how quickly you heal, the health of your eye, and the type of stitches used.
As you recover from surgery, these are things you need to do to care for your eye:
- Use the eye drops exactly as the ophthalmologist prescribed.
- Do not press on or rub your eye.
- If needed, take over-the-counter pain medicine. Ask your doctor which ones you can take.
- Wear eyeglasses or an eye shield to protect your eyes.
- Talk with your ophthalmologist about when you can get back to doing your normal daily routine.
- Depending on your transplant, you may have to lie on your back for a while after surgery. This helps the new donor tissue stay in place.
Call your ophthalmologist if you have concerns or questions about how to care for yourself at home.
Depending on the type of transplant you had and how your eye heals, it can take a year or more to fully recover from this surgery.
Possible problems with corneal transplant
Organ rejection is when the body’s immune system sees transplanted tissue as something that shouldn’t be there and tries to get rid of it. Rejection is a problem for up to 3 out of 10 people who have a full thickness transplant (PK). But prompt treatment with steroids can sometimes reverse the rejection and save the transplant. The risk is lower with partial thickness surgeries.
Warning signs of your body trying to reject your cornea transplant include:
Tell your ophthalmologist right away if you have any of these signs. They might be able to stop the rejection with medicine.
Sometimes corneal transplant can cause other eye problems such as:
Even when corneal transplants work as they should, other eye problems could limit the quality of your vision. For instance, the new cornea might not be curved regularly (called astigmatism). Or you could have an eye disease such as macular degeneration, glaucoma, or diabetic retinopathy.
Some people may need more than one corneal transplant. The first transplant could be rejected, or other problems might occur. However, a repeat transplant has a higher rate of rejection than the first one.
An opportunity for clear vision
If you have a damaged cornea, you and your ophthalmologist will discuss your options for improving your vision. For people with a deeply scarred or swollen cornea, transplant surgery can restore clear vision.