NOTE: Since print publication of this article, the CDC has updated its contact information. This version of the article has been updated to reflect that change.
Download PDF
Although the scourge of syphilis has been largely brought under control by modern medicine’s treatment and prevention measures, earlier this year the U.S. Centers for Disease Control and Prevention (CDC) sounded a warning when syphilis caused serious sequelae, including blindness, in several patients. The CDC called on ophthalmologists, among other health professionals, to be on the lookout for ocular symptoms of syphilis and to expand screening protocols to include any patients who are potentially at risk for sexually transmitted diseases (STDs).1
With 3 physicians who have expertise in detecting and treating STDs, EyeNet explored what the CDC warning means for ophthalmologists.
What You Need to Know
“The eye can be impacted by syphilis at any stage of the disease,” said Gary N. Holland, MD, at UCLA Stein Eye Institute. “Because typical manifestations like posterior uveitis or panuveitis can also be caused by a range of other diseases, an ophthalmic examination alone cannot confirm whether a patient has syphilis. That’s why it’s crucial that ophthalmologists remember to order appropriate syphilis screening tests and collaborate with infectious disease specialists in interpreting test results whenever syphilis is a possibility.”
Tests. When confronted with patients who have unexplained inflammatory eye disease, ophthalmologists should order both treponemal and nontreponemal tests to screen for syphilis, Dr. Holland noted, but he cautioned that false negatives or positives can occur. Robyn N. Fanfair, MD, MPH, of the CDC, explained that because ocular syphilis is a manifestation of neurosyphilis, the CDC advises ordering a cerebrospinal fluid (CSF) test when ocular syphilis is suspected, although a normal CSF result does not rule out ocular syphilis.
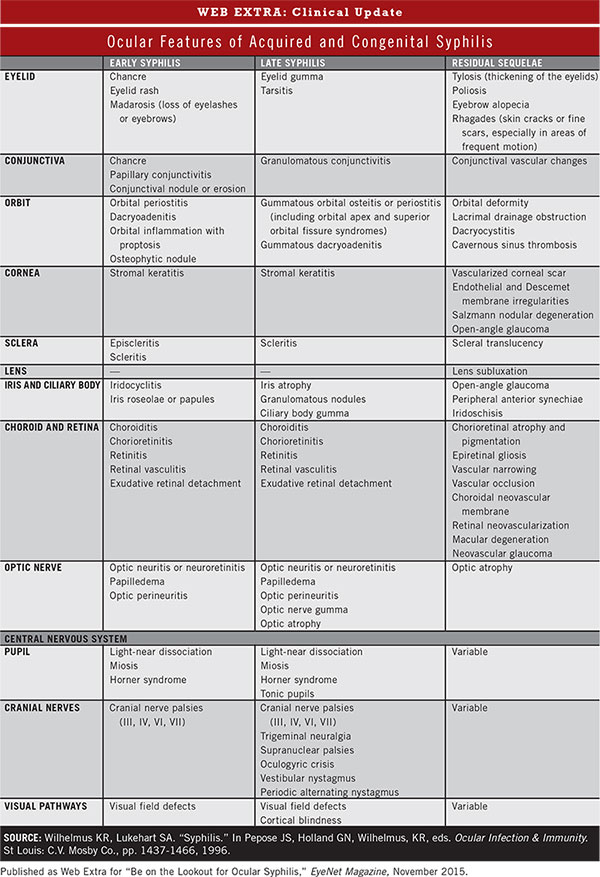
Signs. Most U.S. physicians rarely encounter syphilis, and proper diagnosis is made more challenging by the vague and intermittent nature of the disease’s signs and symptoms, especially early in its course. Also, in the early stage, patients may be unaware of these manifestations or consider them too minor to report to their health care providers. Ophthalmologists need to be aware that ocular syphilis can occur even in the absence of other, nonocular, manifestations of syphilis. Although uveitis is the most common presentation, Dr. Holland reminds ophthalmologists that syphilis can affect nearly all of the eye’s structures and cause neuro-ophthalmic disorders as well. (See “Ocular Features of Acquired and Congenital Syphilis” below.)
Usual suspects. “Although ophthalmologists need to consider syphilis in all patients with ocular inflammatory disease, in large urban areas like Los Angeles syphilis is most commonly seen in HIV-infected individuals,” said Dr. Holland. He added, “Ocular involvement is often seen in more severely HIV-infected patients.” A study by Karumudi and Augenbraun also found increased rates of early neurologic and ocular syphilitic involvement among HIV-infected patients with syphilis.2
(click to expand)
Rising Rates
Paradoxically, medicine’s success in treating HIV infection may be contributing to the increase in syphilis cases noted by the CDC since 2012. Infectious disease specialist Robert L. Murphy, MD, at Northwestern University, said that he is seeing a “near-epidemic of syphilis” among HIV-infected men who have sex with men, or “MSM.” Successfully treated HIV-infected patients usually perceive themselves as being essentially noncontagious, he said, so a false sense of safety may be fueling the apparent upsurge in unsafe sex among MSM. Of course, in reality, these patients and their partners are protected only against HIV, not other STDs. Increased access to anonymous partners due to the rise of online and sex club services may be another factor in the uptick in syphilis, Dr. Murphy added.
Not the usual suspects. “We’ll need to take precautions with patients other than MSM in order to stop this resurgence of syphilis,” said Dr. Murphy, adding that the disease is also being seen in people not traditionally considered vulnerable to syphilis. “We need to test all patients who have or may be at risk for HIV, other STDs, or intravenous drug misuse. This includes people in heterosexual relationships, who may not fully disclose their sexual activities to their partners. And let’s not overlook older people who may still be sexually active.”
Case study. The case of an older man, who was initially referred to Dr. Murphy for suspected toxoplasmosis, highlights why ophthalmologists need to keep syphilis in mind when unusual or unexplained symptoms are present. The man’s symptoms prompted Dr. Murphy to order HIV and syphilis blood tests. Both indicated infection. Dr. Murphy then ordered these STD tests for the man’s wife. (The couple was long married and, as far as the wife knew, monogamous.) Tests showed that she had syphilis but not HIV. The husband then acknowledged that he’d had anonymous sex with a man but hadn’t considered this brief encounter a health risk—and so hadn’t told his wife or physicians. The husband and wife were treated successfully.
Treatment
Dr. Holland recommends the following guidelines to ophthalmologists for managing ocular involvement in patients with syphilis. Such patients should also receive systemic treatment for syphilis, managed by a physician with STD expertise.
- As a sequestered site, the eye requires aggressive antimicrobial therapy.
- Treat aggressively with regimens used for tertiary syphilis, even if the ocular involvement occurs in earlier stages of syphilis.
- Remember that a local Jarisch-Herxheimer reaction can involve the eye and that the associated inflammation can be destructive; patients may need increased anti-inflammatory therapy (including pretreatment before administration of penicillin) and close follow-up immediately after treatment.
- Patients with unknown or previously negative HIV status should receive an HIV test.
Report Ocular Syphilis to the CDC
Dr. Fanfair confirmed that since December 2014, 24 cases of ocular syphilis were reported in California, Washington, and other states. Some of these cases resulted in blindness or other serious sequelae.1 Although the number of overall syphilis cases increased between 2012 and 2013 (the most recent national data available), the STD Prevention division of the CDC is not characterizing the current rates of syphilis as an epidemic or using any similar terminology, she said.
In addition to reporting cases of ocular syphilis to the state or local health department within 24 hours of diagnosis, ophthalmologists are requested to report any cases of ocular syphilis diagnosed since Dec. 1, 2014, to Dr. Oliver at 404-639-1204 or yxo4@cdc.gov, the CDC’s Division of STD Prevention. Dr. Oliver can also provide advice about clinical management of ocular syphilis or assistance with shipment of clinical samples for molecular typing. If possible, pre-antibiotic clinical samples (whole blood, primary lesions and moist secondary lesions, CSF, or ocular fluid) should be saved and stored at –80 degrees C for molecular typing.1
General information about syphilis can be found at www.cdc.gov/std/syphilis. Clinical advisory updates will be posted on the Syphilis: Treatment and Care section of the website.
___________________________
1 www.cdc.gov/std/syphilis/clinicaladvisory os2015.htm Accessed Aug. 25, 2015.
2 Karumudi UR, Augenbraun M. Expert Rev Anti Infect Ther. 2005;3(5):825-831.
___________________________
Dr. Fanfair is Medical Epidemiologist with the CDC’s Division of STD Prevention, Atlanta. Relevant financial disclosures: None.
Dr. Holland is Jack H. Skirball Professor of Ocular Inflammatory Diseases, Department of Ophthalmology, Uveitis Service, UCLA Stein Eye Institute, University of California, Los Angeles. Relevant financial disclosures: None.
Dr. Murphy is Director, Center for Global Health–Institute for Public Health and Medicine, and John Philip Phair Professor of Infectious Diseases, Northwestern University Fein-berg School of Medicine, Chicago. Relevant financial disclosures: None.
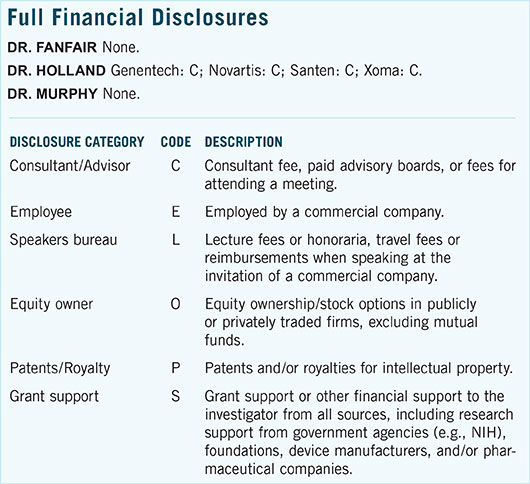
For full disclosures and the disclosure key, see below.