By Enchun M. Liu, MD, Bradley T. Smith, MD, and J. William Harbour, MD
Edited by Steven J. Gedde, MD
Download PDF
Five years since we last saw him, Jason Shepherd* was back in our office with a new problem. We had previously seen Jason when he was 9 years old and had been referred to our office for a chronically red right eye. It had previously been attributed to allergies, and, apart from its appearance, it did not bother him. We diagnosed him with Sturge-Weber syndrome, based on his constellation of physical exam and fundus findings. At the time, he had no ocular or systemic complications, so we recommended routine follow-up with his general ophthalmologist with monitoring of his intraocular pressure (IOP).
Now 14 years old, Jason was having difficulty seeing out of his right eye. In addition to having blurry vision, he reported feeling like a shade was covering the superior aspect of his visual field, and it had been gradually worsening over the past month.
 |
|
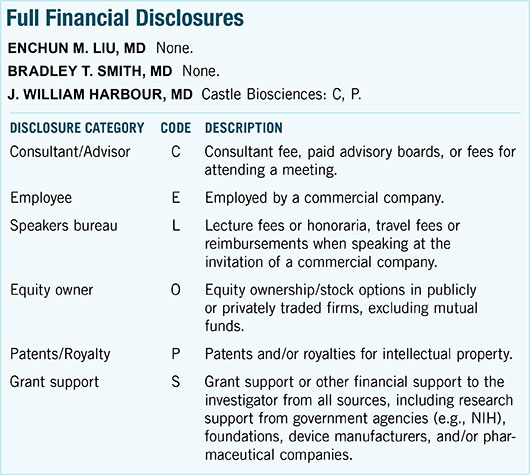
RIGHT EYE. (1) We noted a diffusely dark red choroid from 1 o’clock to 10 o’clock, a reddish orange lesion in the macula, and an inferior retinal detachment. (2) B-scan ultrasound showing a diffusely thickened choroid with focal circumscribed elevation in the macula. (3) A-scan ultrasound over the lesion showing medium to high internal reflectivity.
|
The Exam
Jason’s visual acuity (VA) was 20/80 in the right eye and 20/15 in the left eye. There was no afferent pupillary defect. His IOP by applanation was 15 mm Hg in the right eye and 19 mm Hg in the left eye. His anterior segment examination showed conjunctival hyperemia in the inferior aspect of his right eye. Gonioscopy of the right eye revealed prominent iris vessels in the inferior angle, without any iris or angle neovascularization.
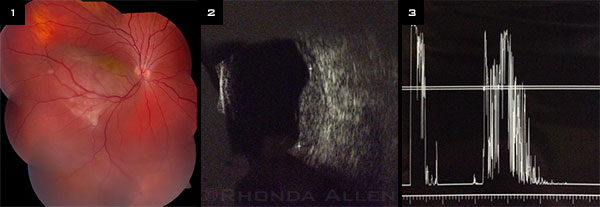
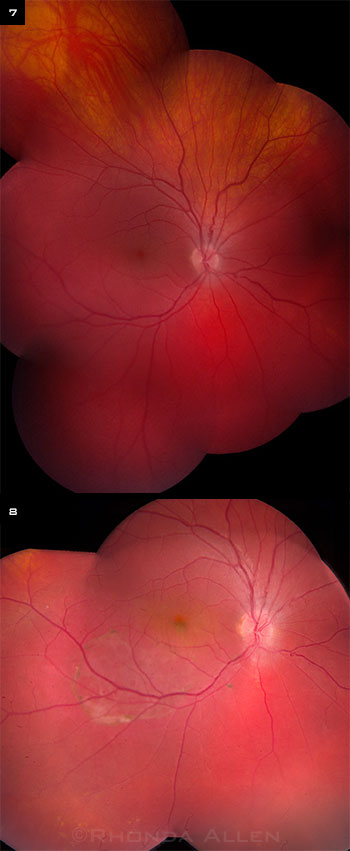
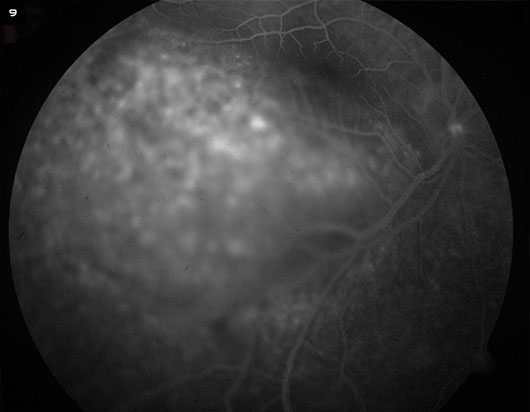
On dilated fundus examination, Jason’s right eye was noted to have a well-circumscribed orange-red lesion within the macula and an inferior retinal detachment from 3 o’clock to 9 o’clock (Fig. 1). The choroid had a diffuse dark red appearance from 1 o’clock to 10 o’clock. B-scan ultrasonography of the right eye revealed a diffusely thickened choroid with a focal area of round choroidal elevation in the macula (Fig. 2). The corresponding A-scan showed medium to high internal reflectivity. Fluorescein angiography revealed early stippled hyperfluorescence within the macular lesion with staining in the late phase (Fig. 9). Spectral domain optical coherence tomography (SD-OCT) over the macula showed choroidal elevation with overlying subretinal fluid (Fig. 4). Interestingly, there appeared to be areas of fluid loculation underneath the retina in a few of the scans (Fig. 5).
On physical examination, the patient had a small nevus flammeus on the right side of his upper lip (Fig. 6), in addition to large patches of pigmented café-au-lait–like lesions on the right side of his chest and back.
 |
|
FURTHER EVIDENCE. SD-OCT showing (4) choroidal elevation with overlying subretinal fluid and (5) focal areas of loculated subretinal fluid. (6) Small nevus flammeus on the patient’s right side, above his upper lip.
|
Diagnosis and Treatment
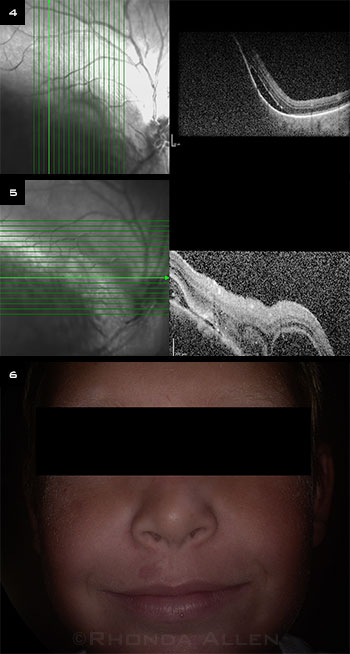
When we first saw Jason as a 9-year-old, his vision was 20/40 in the right eye, and he had an incomplete diffuse choroidal hemangioma from 1 o’clock to 10 o’clock (Fig. 7). He had normal IOP, and there was no exudative retinal detachment at that time. We had recommended a screening MRI/MRA to rule out ipsilateral intracranial vascular malformations, but his parents declined further workup.
Now, 5 years after his initial diagnosis, we believed that Jason had developed a new focal circumscribed choroidal hemangioma within the macula that caused an inferior exudative retinal detachment. After discussing the treatment options with the patient and his parents, they elected external beam radiation therapy.
Jason underwent low-dose lens sparing external beam radiation (≤20 Gy) to his right eye 1 month after being diagnosed with his exudative retinal detachment. Three months after treatment, his vision had improved to 20/60 in the right eye. The circumscribed hemangioma in the macula was considerably decreased in size, but we noted that there was still a small amount of subretinal fluid remaining inferiorly, outside the inferior arcade (Fig. 8).
 |
|
ADDITIONAL FUNDUS IMAGES. (7) Five years previously, when Jason was 9 years old, we diagnosed him with Sturge-Weber syndrome. At that time, we had noted an incomplete diffuse choroidal hemangioma from 1 o’clock to 10 o’clock. (8) At age 14, he underwent low-dose external radiation for a new macular circumscribed choroidal hemangioma with inferior exudative retinal detachment. Resolution of the macular subretinal fluid is noted in this fundus montage taken 3 months posttreatment.
|
Discussion
Sturge-Weber syndrome (SWS), also known as encephalotrigeminal angiomatosis, is a congenital neurocutaneous disorder that frequently involves the eye. Unlike other phakomatoses, such as neurofibromatosis or tuberous sclerosis, SWS is a sporadic condition with no known inheritance. The incidence of SWS is estimated to be 1 in 20,000 to 50,000 live births.1
Possible cause. A recent study found that whole-genome DNA sequencing of visibly affected tissue from patients with SWS revealed a somatic activating mutation in GNAQ1.2 It is hypothesized that this leads to increased activation signaling, which results in the blood vessels becoming malformed, dysregulated, and progressively dilated.
Signs and symptoms. Systemic findings of this syndrome include a cutaneous capillary malformation along the trigeminal nerve (port-wine stain, or nevus flammeus) and ipsilateral leptomeningeal vascular malformations. Central nervous system involvement can lead to focal neurological deficits such as seizures, hemiplegia, and mental deficiency. Many patients with SWS, however, have normal intelligence.
In the eye, SWS classically manifests with a diffuse choroidal hemangioma ipsilateral to the facial port-wine stain. The diffuse dark red appearance of the choroid on ophthalmoscopy gives it the commonly used name of “tomato ketchup” fundus. Although the classic ocular finding in SWS is diffuse choroidal hemangioma ipsilateral to the facial port-wine stain, the most common ocular finding is glaucoma. This can be due to angle development anomalies (usually when patients are younger than 2 years old), or from elevated episcleral venous pressure. In a review of 51 patients with SWS, Sullivan and colleagues found that 71% of patients had glaucoma, 69% had congested conjunctival or episcleral vessels, and 55% had diffuse choroidal hemangioma.3
Vision loss in SWS occurs secondary to a hyperopic shift, amblyopia, macular edema, glaucoma, or exudative retinal detachment. Although present at birth, diffuse choroidal hemangiomas often do not cause an exudative retinal detachment until later in life, with an average age of onset at 8 years.4 Indeed, patients often don’t present with an exudative retinal detachment until adolescence, because the lesion grows with the patient. This was the case in our patient, who had an incomplete diffuse choroidal hemangioma but did not develop an exudative retinal detachment until adolescence.
Goal of treatment. The goal of treatment for diffuse choroidal hemangioma with a concomitant exudative retinal detachment is to cause involution of the lesion and subsequent resolution of subretinal fluid without damaging the overlying retina. Patients without exudative retinal detachment or glaucoma are usually monitored for the development of these complications.
Types of treatment. Different treatment modalities for these hemangiomas have been reported with varying success, including laser photocoagulation, plaque brachytherapy, photodynamic therapy, and external beam radiation (the latter 2 are the most widely used).4 Successful involution of diffuse choroidal hemangiomas with oral propranolol or anti-VEGF treatment has also been reported in single case studies,5-8 but long-term follow-up and larger studies are needed.
|
Web Extra: Morning Rounds
|
 |
|
FLUORESCEIN ANGIOGRAM. We noted early stippled hyperfluorescence with late staining.
|
Conclusion
SWS is a rare, spontaneous, congenital neurocutaneous disorder. It commonly presents with vision loss at a young age due to exudative retinal detachment from a diffuse choroidal hemangioma. Prompt recognition and early referral for treatment can help prevent late complications from unrecognized glaucoma or exudative retinal detachment.
We believe Jason presented with a forme fruste, or partial expression, of the syndrome, with an incomplete diffuse choroidal hemangioma, absence of glaucoma, and no mental deficiency. He developed a new circumscribed lesion at adolescence, causing an exudative retinal detachment. The condition responded well to external beam radiation, with lesion regression, resolution of subretinal fluid in the macula, and return of vision to near baseline at 3 months posttreatment. Now at 1 year after radiation treatment, there are no signs of recurrence, and Jason’s visual acuity is 20/30 in the right eye, and his lens remains clear.
___________________________
* Patient name is fictitious.
___________________________
1 Comi AM. Lymphat Res Biol. 2007;5(4):257-264.
2 Shirley MD et al. N Engl J Med. 2013;368(21):1971-1979.
3 Sullivan TJ et al. J Pediatr Ophthalmol Strabismus. 1992;29(6):349-356.
4 Tsipursky MS et al. Surv Ophthalmol. 2011;56(1):68-85.
5 Paulus YM et al. Ocul Immunol Inflamm. 2009;17(4):292.
6 Shoeibi N et al. Ocul Immunol Inflamm. 2011;19(5):358-360.
7 Arevalo JF et al. Arch Ophthalmol. 2011;129(10):1373-1375.
8 Thapa R, Shields CL. Eur J Ophthalmol. 2013;23(6):922-924.
___________________________
Dr. Liu is a former vitreoretinal fellow at The Retina Institute in St. Louis and is now at Retina Associates of South Texas in San Antonio. Dr. Smith is a vitreoretinal and ocular tumor specialist at The Retina Institute in St. Louis. Dr. Harbour is director of the ocular oncology service at Bascom Palmer Eye Institute in Miami. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.