By Katherine A. Tsamis, MD, Eric W. Hein, MD, and Vishak J. John, MD
Edited by Steven J. Gedde, MD
Download PDF
When we first met 10-year-old Diego Alvarez* and his mother in clinic, they were clearly distressed about his progressive loss of vision, which began when he was 5. At first, he had difficulty with color, and he soon began losing his central vision. He denied having photophobia. Apart from the visual loss, he appeared to be healthy. In Peru, he had been diagnosed with retinitis pigmentosa (RP), and his mother brought him to the United States for a second opinion.
We Get a Look
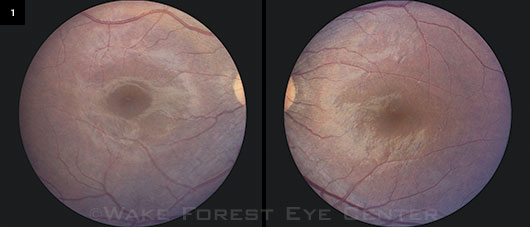
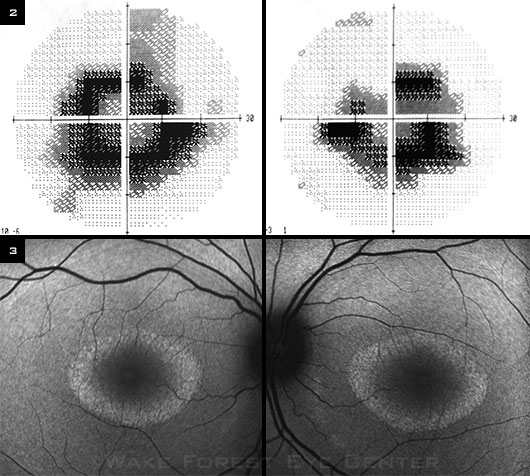
When we examined Diego, BCVA was 20/100 in both eyes, with normal pupils and full motility. No nystagmus was noted. Diego could not identify any of the Ishihara color plates except for the control. The slit-lamp examination was normal. The fundus exam revealed a 0.1 cup-to-disc ratio with normal vessels, a healthy-appearing macula, and mild pigmentary changes in the midperiphery bilaterally (Fig. 1). Humphrey visual fields demonstrated a central scotoma in both eyes (Fig. 2). Fluorescein angiography done in Peru was essentially normal. Optical coherence tomography (OCT) did not reveal any obvious retinal abnormalities in either eye.
In Peru, Diego had undergone pattern electroretinogram (ERG) testing, which demonstrated diminished retinal ganglion cell function. Full-field ERG changes expected in RP include a reduction in the a- and b-wave amplitudes and prolonged implicit times.
The initial ophthalmologist had diagnosed RP in this child with retinal pigmentary changes, central visual field loss, and ERG abnormalities. However, we were not convinced of this diagnosis because RP rarely presents with predominantly macular involvement or decreased visual acuity so early in the disease.
 |
|
WE GET A LOOK.The macula appeared normal in both eyes. Mild RPE changes were noted in the midperiphery of each eye.
|
The Next Step
Because of the relatively normal fundus exam, we utilized a newer imaging modality in clinic to aid in diagnosis. Fundus autofluorescence (FAF) imaging revealed a perifoveal hyperfluorescent ring, or bull’s-eye changes (Fig. 3).
This expanded our differential diagnosis to include cone dystrophies, toxic maculopathies, and Stargardt disease. Our patient had no history that suggested retinal toxicities, and we did not see the characteristic dark choroid of Stargardt on fluorescein angiography.
 |
|
HVF AND FAF. (2) Humphrey visual field testing demonstrated a central scotoma in both eyes. (3) Fundus autofluorescence imaging of our patient demonstrated the typical appearance of bull’s-eye maculopathy.
|
Discussion
Bull’s-eye changes on FAF combined with loss of color vision on exam make cone dystrophy the most likely diagnosis.
Categories and subtypes. Cone dystrophies can be categorized into stationary or progressive. Stationary cone dystrophy usually presents during childhood with diminished central vision that remains stable over time. In progressive cone dystrophy, central vision gradually deteriorates over time.
There are many subtypes of cone dystrophies, including achromatopsia, incomplete achromatopsia, and blue-cone monochromatism. The clinical symptoms and genetics vary considerably. Autosomal dominant, autosomal recessive, and X-linked recessive cases have all been reported.
Some symptoms to watch for. While patients with cone dystrophy present with decreased visual acuity, peripheral visual fields are usually spared, and the fundus may appear normal in the early stages of the disease.1 Other symptoms may include reduced color vision, photophobia, and nystagmus.
The value of fundus autofluorescence imaging. The bull’s-eye appearance of the macula is a classic sign for cone dystrophy due to retinal pigment epithelium (RPE) atrophy around the fovea. The loss of RPE integrity may not be apparent on ophthalmoscopic exam at early stages of the disease, which is why FAF is valuable for diagnosing, as well as monitoring, retinal diseases. FAF records fluorescence that occurs in the eye naturally with aging or as a result of a disease process. Autofluorescence is distinguished from fluorescence that is induced by administration of fluorescein or indocyanine green. Hyperfluorescence on FAF indicates localized accumulation of lipofuscin, which is a by-product of photoreceptor outer segment dysgenesis and RPE metabolism.
The value of electroretinogram testing. Since hyperautofluorescence in the foveola is a nonspecific manifestation of photoreceptor–RPE dysfunction, complete photopic and scotopic ERG testing is recommended.2 Pattern ERG, which our patient completed, is more useful for localized retinal dysfunction and is not as informative as full-field ERG for conditions involving the entire retina, such as cone dystrophy.
Potential therapies. There are currently no cures for cone dystrophy, but research is leading to a better understanding of genetic mutations involved in retinal function.3 Clinical trials are exploring the use of dietary supplementation—such as vitamin A, saffron, and DHA—as well as gene and cell therapies to slow the progression of photoreceptor degeneration.
Our Recommendations
In the absence of proven therapies for cone dystrophy, management is directed toward symptomatic control. For example, avoiding bright environments and using tinted glasses can provide the patient with ultraviolet protection of the retina. For our patient, we recommended magnifiers and other low vision aids. We also recommended that Diego undergo genetic testing, and that he complete a full-field ERG to get a more accurate global picture of retinal function.
___________________________
1 Hamel CP. Orphanet J Rare Dis. 2007;2:7.
2 Wang NK et al. Doc Ophthalmol. 2009;119(2):141-144.
3 Simunovic MP et al. Eye (Lond). 1998;12(3b):553-565.
___________________________
*Patient name is fictitious.
___________________________
Dr. Tsamis will be an ophthalmology resident, Dr. Hein is an assistant professor of ophthalmology, and Dr. John is an assistant professor of ophthalmology; all are at Wake Forest University School of Medicine in Winston-Salem, N.C. Relevant financial disclosures: None.
Be Published in EyeNet
Morning Rounds. If you had a mysterious or challenging case, share it with your colleagues.
Ophthalmic Pearls. Review a medical condition or surgical procedure.
Blink. Got an image that is perplexing or intriguing? Let us showcase it.
Letters. EyeNet welcomes your correspondence on all ophthalmic issues.
How to get started. Visit “Write for Us.”
|