Download PDF
Antibiotic resistance to common ocular pathogens continues to be a challenge, according to the most recent data from the ongoing Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance Study, presented at the 2016 Association for Research in Vision and Ophthalmology (ARVO) annual meeting.1
New data, continuing trends. The updated data are based on 441 isolates collected from 19 sites in 2015. The current findings follow a trend that has been observed since 2009, when the nationwide multicenter survey began looking at resistance of common ocular pathogens to several commonly used antibiotics. The data show high levels of antibiotic resistance among staphylococcal isolates, especially among methicillin-resistant (MR) strains, with many isolates demonstrating multidrug resistance.
“This trend is here to stay; and even if it does not increase, the level is so high that not dealing with antibiotic resistance is not an option,” said Penny A. Asbell, MD, MBA, professor, Department of Ophthalmology, Icahn School of Medicine at Mount Sinai, New York.
Key findings. The report analyzed organisms frequently implicated in bacterial eye infections; common ocular isolates submitted by labs nationwide include Staphylococcus aureus (SA), coagulase-negative staphylococci (CoNS), Streptococcus pneumoniae, Haemophilus influenzae, and Pseudomonas aeruginosa. The isolates were tested for susceptibility to as many as 15 antibiotics. Following are some of the key findings:
- Resistance among staphylococci was most notable for azithromycin (54%-59%), oxacillin/methicillin (24%-45%), and ciprofloxacin (22%-28%).
- CoNS isolates exhibited substantial levels of resistance to trimethoprim (26%) and tobramycin (19%).
- 39% of CoNS isolates and 20% of SA isolates were resistant to 3 or more drug classes.
- Multidrug resistance remained prevalent among MRSA (67%) and MRCoNS isolates (74%).
- Resistance among P. aeruginosa isolates continues to be low, and H. influenzae isolates were generally susceptible to all antibiotics tested.
Advice for clinicians. “Choosing the best antibiotic to use is not trivial,” said Dr. Asbell. It requires determining the possible organism and its sensitivities and the antibiotic’s ability to penetrate the target tissue, as well as its biocompatibility or safety profile, she said.
Dr. Asbell advised clinicians to keep handy the tables from the 5-year ARMOR surveillance study, including more than 3,200 isolates, published last year in JAMA Ophthalmology.2 “The ARMOR data can be useful for selecting your first antibiotic to use, especially if fortified compounded antibiotics are not available,” she said. “These data should be used hand-in-hand with local antibiograms from hospitals to aid therapy selection and improve antibiotic stewardship.”
Dr. Asbell offered further recommendations for prescribing antibiotics:
- Don’t prolong treatment.
- Don’t use antibiotics to treat allergies and/or viral infections.
- Consider antibiotic cycling/rotation based on resistance trend data.
- Emphasize the importance of treatment adherence to your patients.
ARMOR is continuing to collect ocular isolates from centers nationwide. In the meantime, Dr. Asbell urged clinicians to “choose the antibiotic wisely” for the initial treatment, since not all antibiotics will work on all isolates. Then check culture results to adjust as the clinical course demands. “Clinical assessment still counts,” she said. “Each case needs to be considered individually.”
—Miriam Karmel
___________________________
1 Sanfilippo CM et al. Antibiotic Resistance Profiles of Ocular Pathogens—An Update from the 2015 ARMOR Surveillance Study. Poster presented at: ARVO Annual Meeting; May 4, 2016; Seattle.
2 Asbell PA et al. JAMA Ophthalmol. 2015;133(12):1445-1454.
___________________________
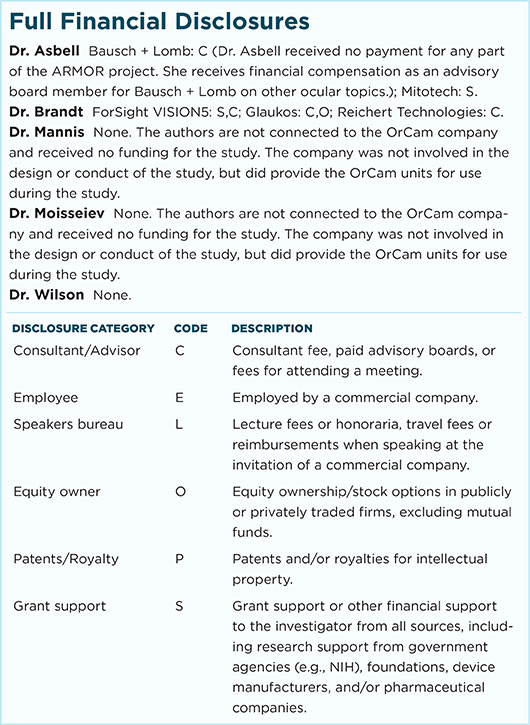
Relevant financial disclosures—Dr. Asbell: Bausch + Lomb: C (unrelated to this article).
For full disclosures and disclosure key, see below.
More from this month’s News in Review