Download PDF
Stacy Smith* recently got a new pair of glasses to correct her myopia. At first, the 47-year-old was quite happy with her new vision, but this satisfaction did not last. She came back 4 months later complaining of blurry vision with her new spectacles—they just were not helpful any longer.
Medical History
Ms. Smith has a history of relapsing-remitting multiple sclerosis (MS) and had recently started taking dimethyl fumarate. However, immediately after beginning the medication, she developed flushing and “vision changes,” so the medication was stopped. She was subsequently switched to glatiramer. She also recently started topiramate for headaches.
Her other medical problems included hypertension and hyperlipidemia, for which she was taking amlodipine-valsartan-hydrochlorothiazide and atorvastatin, respectively.
We Get a Look
On examination, her visual acuity with her current spectacles was 20/400 in both eyes. There was no afferent pupillary defect. Her intraocular pressure by applanation was 16 mm Hg in the right eye and 17 mm Hg in the left. Her ocular movements were full, and visual fields were full to confrontation in both eyes.
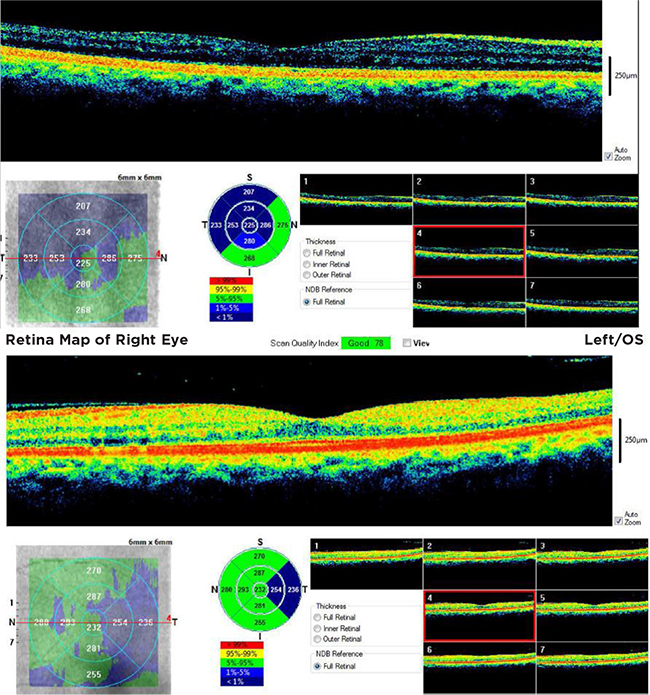
Slit-lamp examination revealed +1 nuclear sclerosis in both eyes, with an otherwise normal anterior segment exam. Her fundus examination was within normal limits as well. To complete the evaluation, we obtained optical coherence tomography (OCT) of the macula, which was found to be normal. (To review those OCT images, see below.)
 |
|
OCT. The authors noticed nothing unusual when they reviewed the OCT imaging.
|
Refraction
As mentioned earlier, her recently purchased spectacles had initially improved her visual acuity but were now no longer helpful. Four months ago, her refraction was –2.50 +0.50 × 180 in her right eye and –2.25 +0.50 × 035 in her left eye, with a best-corrected visual acuity (BCVA) of 20/20.
However, at her follow-up clinic visit, her new refraction was found to be +1.75 +0.75 × 180 in her right eye and +2.25 +0.50 × 025 in her left eye with a BCVA of 20/30 in her right eye and 20/25 in her left eye. This refraction was significant for a binocular hyperopic shift of approximately 4 D since her prior visit (see Table 1, below).
Table 1: What Caused the Change in Refraction?
| |
Sphere |
Cylinder |
Axis |
Distance VA |
Add |
Near VA |
| At time of new glasses |
| Right |
–2.50 |
+0.50 |
180 |
20/20- |
+1.50 |
J1+ |
| Left |
–2.25 |
+0.50 |
035 |
20/20- |
+1.50 |
J1+ |
| 4 months later |
| Right |
+1.75 |
+0.75 |
180 |
20/30- |
+1.50 |
J1 |
| Left |
+2.25 |
+0.50 |
025 |
20/25 |
+1.50 |
J1+ |
Differential Diagnosis
Given this new finding and an overall insignificant exam, we generated our differential diagnosis by reviewing the possible causes of a bilateral hyperopic shift, starting from the front of the eye and working posteriorly.
A reduction in corneal curvature can induce hyperopia, but she was not found to have corneal pathology on exam. Adie’s topic pupil can be associated with a hyperopic shift, but her pupils were equal, round, and briskly reactive. Cataracts commonly cause a myopic shift, but they occasionally produce hyperopia. She did have a mild cataract, but it was not significant on exam. Posterior dislocation of the lens can induce hyperopia, but her lens was in a normal anatomical position. Lenticular osmotic shifts can cause a refractive change, with diabetes mellitus in the state of hyperglycemia being the most common culprit, typically causing a myopic shift. However, her hemoglobin A1c was checked 8 months previously and was found to be normal.
We then discussed other etiologies that could push the retinal pigment epithelium/retina anteriorly and cause a hyperopic shift, but this was unlikely, based on her normal OCT. Orbital masses can shorten the axial length and induce hyperopia. However, she had a recent MRI because of her history of MS, and it did not reveal any orbital masses.
We considered the possible effects of recent medications. Glatiramer has been associated with dry eyes and diplopia. Topiramate is classically associated with a myopic shift due to anterior displacement of the lens-iris diaphragm. Dimethyl fumarate has not been reported to be associated with ocular symptoms. However, none of these medications have been associated with hyperopic shifts.
Making the Diagnosis
Despite knowing that hyperglycemia typically causes a myopic refractive change, we decided to check our patient’s hemoglobin A1c anyway, as hyperopic changes have been mentioned in the literature (though they are rare). This decision was made after we had excluded many causes of bilateral hyperopic shifts to ensure that no common conditions had been missed. Her hemoglobin A1c returned with a clinically significant value of 13.5%. We immediately called Ms. Smith to inform her of the results and asked her to speak to her primary care physician as soon as possible to start medical therapy.
We Review the Literature
Diabetes mellitus is the leading cause of new blindness in people under the age of 65. Given the rarity of hyperopic shifts associated with hyperglycemia and diabetes, we did a literature search to determine the pathophysiology of this occurrence.
Refractive errors in diabetic patients were first described in 1798 by John Rollo, who found an association between diabetes and cataracts.1 Sustained and transient refractive changes have been described in the literature.2 Sustained refractive changes are thought to occur in the setting of increased thickness and increased surface curvature of the crystalline lens, which typically causes a myopic shift. However, transient refractive changes are thought to result from changes in the refractive index of the lens, which can cause a myopic or hyperopic shift.
In the literature on hyperglycemia, the majority of sources present various theories to explain the myopic shift associated with diabetes and hyperglycemia1-4; however, as seen in our review of that literature, there are a few theories that explain how transient hyperopia can occur in the setting of hyperglycemia.5
- Overhydration of the crystalline lens and sorbitol production can lead to a decrease in the lens’ index of refraction and subsequent hyperopia.
- A small increase in the refractive indices of the aqueous and vitreous humor can occur in the hyperglycemic state, decreasing the power of the lens and leading to hyperopia.
- Choroidal thickening may affect the axial length of the eye, producing a hyperopic shift.
- Paresis of accommodation due to excessive glycogen deposits in the pigment epithelium of the ciliary body has also been noted in 21% of diabetic patients.1
Therefore, although the association of hyperglycemia and myopia has been the conventional thought process, hyperopia can and does occur in the setting of hyperglycemia.
Treatment
Ms. Smith was visually symptomatic, with 4 D of hyperopic shift and inability to use the spectacles that she had been prescribed just 4 months previously. However, not all diabetic individuals who have a refractive change are symptomatic.3 Given her new diagnosis of diabetes with visually significant symptoms, she was referred back to her primary care physician for evaluation and management of her diabetes. She was subsequently started on glyburide to control her blood sugar levels.
Follow-up
Ms. Smith’s hemoglobin A1c level is now 6.8%. At her most recent evaluation, her refraction was –0.25 +0.75 × 050 in her right eye and plano +1.25 × 165 in her left eye. Her BCVA was 20/50 in her right eye and 20/40 in her left eye because she had developed posterior subcapsular diabetic cataracts in both eyes, worse in the left than the right eye. Ms. Smith will be undergoing surgical removal of her cataracts with intraocular lens implantation in the near future.
She was very thankful to our team for diagnosing her diabetes and getting her the care she needed to achieve a better state of health.
___________________________
* Patient name is fictitious.
___________________________
1 Waite JH et al. N Engl J Med. 1935;212(9):367-379.
2 Bron AJ et al. Eye. 1993;7(Pt 2):260-275.
3 Duke-Elder WS. Br J Ophthalmol. 1925;9(4):167-187.
4 Furushima M et al. Jpn J Ophthalmol. 1999;43(5):398.
5 Mehdizadeh M et al. Ophthalmologica. 2010;224(1):63
___________________________
Dr. Patel is an ophthalmology resident, Dr. Domeracki is associate professor of clinical ophthalmology and director of the ophthalmology residency program, and Dr. Krakauer is an assistant professor of clinical ophthalmology; all 3 of them are at Temple University Hospital in Philadelphia. Relevant financial disclosures: None.