Download PDF
The differential diagnosis for a swollen disc can be extensive. Here are 4 illustrative examples.
With causes ranging from the infectious to the vascular to the malignant, the swollen optic nerve is a crucial, but often mystifying, sign. And the patient’s vision—or life—may depend on a timely diagnosis. What steps should you take to pin down the diagnosis? Four neuro-ophthalmologists contributed instructive cases from their own practices. They also provided general guidelines on how to conduct the examination, tips for distinguishing between pseudopapilledema and true optic disc swelling (see “Is It Real?”), and a brief overview of unilateral and bilateral disc edema (see “Quick Guide to the Differential Diagnosis”).
Performing a Good Examination
As you begin taking a full neurological and ophthalmic history, ask specifically about any headaches, the experts said. Other tips are as follows:
- Don’t dilate the patient’s pupils until you have determined whether a relative afferent pupillary defect (RAPD) is present.
- Pay attention to the perimeter of the disc, looking for retinal nerve fiber layer opacification with obscuration of the retinal vessels overlying the disc margin.
- Note the color of the disc and any abnormal vasculature.
- If you have a clear view, look for a spontaneous venous pulsation.
- Examine the fellow eye for comparison.
- To assess optic nerve function, check visual acuity, color vision, and contrast sensitivity.
- Do an automated visual field (VF) test to look for an enlarged blind spot.
- Assess the patient’s neurological system and cranial nerves.
Case 1
Acute Unilateral Vision Loss With Pain
Courtesy of M. Tariq Bhatti, MD
History and Exam
A 34-year-old woman presented with 3 days of decreased vision in her left eye associated with ocular pain, which worsened when she moved the eye. She had no significant history of previous medical, ocular, or neurological problems, and she was not taking any medications. A complete review of systems was negative; in particular, she did not have any recent illness and was not in contact with domestic or feral cats.
The examination revealed that her visual acuity (VA) was 20/20 in her right eye and counting fingers in her left. She had a left RAPD and was not able to identify any of the color plates with her left eye. The slit-lamp examination and her intraocular pressures (IOPs), ocular motility, and cranial nerve function were all normal. The dilated fundus exam was normal in the right eye, but the optic nerve was swollen in the left.
Clinical Course and Outcome
Given the patient’s age and symptoms, we suspected acute inflammatory demyelinating optic neuritis (ON). Acute ON is characterized by acute to subacute, most often unilateral, painful loss of vision; dyschromatopsia; an RAPD; and a VF defect.1 Notably nearly two-thirds of patients with ON have a normal-appearing optic nerve (i.e., retrobulbar ON).
Diagnostic testing included routine blood tests and orbital and cranial magnetic resonance imaging (MRI) with contrast to determine whether there was any abnormality of the optic nerve itself or in structures in proximity to the nerve. The orbital MRI demonstrated enhancement of the optic nerve; in addition, there were multiple white matter lesions on the cranial MRI.
The patient was prescribed high-dose IV methylprednisolone (1 g per day) for 3 days; this was followed by oral prednisone (1 mg/kg per day) for 11 days and then by a 4-day taper. Intravenous methylprednisolone accelerates visual recovery from ON but has no impact on long-term visual outcome. The visual prognosis is excellent in most cases, regardless of whether the patient is treated with corticosteroids.2 In this case, the patient’s vision was restored within 6 weeks.
The presence of white matter lesions on an MRI scan is the strongest predictor for developing multiple sclerosis (MS).2 If a patient’s brain MRI is abnormal (1 or more lesions), the risk of developing MS at 15 years is approximately 70%. In contrast, if the brain MRI is normal (0 lesions), the 15-year risk of developing MS drops to 25%.3
A first episode of neurological symptoms that lasts at least 24 hours and is caused by inflammation and demyelination in 1 or more sites in the central nervous system is referred to as a clinically isolated syndrome (CIS), and CIS patients with an abnormal MRI are encouraged to begin treatment with a disease-modifying drug to delay the onset of MS.2 I discussed the implications of the patient’s MRI results with her. She was started on β-interferon and has had no further neurological episodes to date.
Final Diagnosis
Inflammatory demyelinating optic neuritis with a high risk of MS as indicated by cranial MRI
Key Points
- Acute loss of vision from an optic neuropathy in a young person is most often due to ON.
- Visual prognosis is excellent with ON.
- The assessment of MS risk is based on the brain MRI.
- Consider treatment of high-risk patients (abnormal MRI) with a disease-modifying drug.
Case 2
Bilateral Vision Loss With Headache
Courtesy of Leah Levi, MD
History and Examination
A 16-year-old girl with no health problems aside from a body mass index (BMI) of 30 presented with a headache. She told us that her vision had become fuzzy over a period of several weeks, but she denied having any visual blackouts or pulsatile bruits.
On initial examination, her uncorrected VA was 20/25+ in her right eye and 20/25 in her left, not improving with pinhole. Her color vision (Hardy-Rand-Rittler) was 5/6 in her right eye and 4.5/6 in her left. VF testing showed a markedly enlarged blind spot in each eye. There was no RAPD. The patient was orthophoric in all positions of gaze, with full ductions. The slit-lamp exam and her IOPs were normal. There was marked disc edema in each eye.
Clinical Course and Outcome
The patient was sent for an urgent MRI scan, which showed no abnormalities of the brain such as tumor or hydrocephalus. There was increased cerebrospinal fluid (CSF) around both optic nerves, with flattening of the posterior aspect of the globes. Magnetic resonance venography (MRV) showed no venous sinus thrombosis. Lumbar puncture showed an opening pressure of 43 cm H2O and normal CSF composition.
The patient was diagnosed with idiopathic intracranial hypertension (IIH) and was started on acetazolamide 500 mg twice daily; in addition, she was advised to lose weight. As she was followed, her symptoms resolved, and her clinical findings improved. The acetazolamide was tapered and finally discontinued 6 months after the patient’s initial presentation. A follow-up exam approximately 2 months later showed 20/20 acuity, color vision of 6/6, and normal VF testing in each eye, with no papilledema.
Although the clinical presentation in a young overweight female was consistent with IIH, this diagnosis should not be made before ruling out other causes of bilateral optic disc swelling, including mass lesions of the brain; venous sinus thrombosis; and inflammatory, infiltrative, and infectious causes. The patient must have neuroimaging, including MRI and MRV, as well as a lumbar puncture. The CSF must be normal aside from the increased opening pressure. If the demographic is not the typical overweight female, the history should be directed at uncovering known causes of increased intracranial pressure, such as certain medications or underlying medical conditions.4
Final Diagnosis
Idiopathic intracranial hypertension
Key Points
- The diagnosis of IIH cannot be made without neuroimaging, including MRI and MRV, and a lumbar puncture that shows increased opening pressure as the only abnormality.
- In most cases, treatment with the highest-tolerated dose of acetazolamide will lead to resolution.5
- IIH is more severe and the risk of visual loss is higher in patients who have a BMI greater than 40.6
Case 3
Acute Unilateral Vision Loss Without Pain
Courtesy of Anthony C. Arnold, MD
History and Examination
A 64-year-old man awoke with impaired vision in the inferior visual field of his left eye 3 days before he consulted us. He had no headache, pain with eye movements, or other systemic symptoms, and his vision had remained stable over that 3-day period. He had a history of hyperlipidemia and systemic hypertension.
The examination revealed that his VA was 20/20 in his right eye and 20/40 in his left. A left RAPD was present. The anterior segment, ocular motility, and cranial nerve examinations were normal. Dilated funduscopy demonstrated clear media, a normal right optic disc with structurally full configuration and no cup, and a similarly structured left optic disc, with segmental disc edema and a parapapillary retinal flame hemorrhage. Quantitative perimetry demonstrated an inferior altitudinal VF defect in the left eye; the right eye was normal.
Clinical Course and Outcome
Based on the relatively acute onset of painless inferior VF loss with evidence of optic nerve edema and dysfunction in a patient with known vasculopathic risk factors, we made a tentative diagnosis of nonarteritic anterior ischemic optic neuropathy (NAION).7 Although there were no symptoms suggestive of giant cell arteritis, we ordered screening tests for vasculitis, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). All were normal, with the latter 2 measuring 26 mm/hr and 0.4 mg/L, respectively. We do not routinely perform MRI of the brain in typical cases of NAION.
The patient was referred to his internist to assess for control of his known risk factors and to screen for others, such as diabetes and obstructive sleep apnea.8 We cautioned that he should avoid excessive nighttime doses of antihypertensive medications, which might exacerbate nocturnal hypotension and possibly potentiate further optic disc ischemia. We recommended the initiation of low-dose aspirin therapy at 80 mg/day, in hope of reducing the risk of fellow eye involvement. At 6 months’ follow-up, the patient’s VA had improved to 20/25, and the VF defect showed mild improvement.
There is no proven effective therapy for NAION.7 The majority of patients maintain a stable VA and VF after the initial episode of visual loss, although a minority (25% to 40%) demonstrate some degree of deterioration during the first 4 to 6 weeks after onset. Recurrence in the same eye is relatively rare, occurring in 5% or less in most studies. During follow-up, some 40% of patients spontaneously improve by at least 3 lines of Snellen acuity.9 This feature must be taken into account when assessing the effectiveness of multiple recently proposed therapies, including corticosteroids and other intravitreal compounds, such as VEGF inhibitors and potential neuroprotective agents.
Fellow-eye involvement is estimated at roughly 15% of patients within 5 years. There is limited evidence that low-dose aspirin may reduce this rate,10 with the added potential benefit of reducing risk of other cardiovascular events.
Final Diagnosis
Nonarteritic anterior ischemic optic neuropathy
Key Points
- NAION is the most common acute optic neuropathy in patients older than age 50.
- Clinical features include an RAPD, optic disc edema with flame hemorrhage, and inferior altitudinal VF loss.
- Giant cell arteritis must be ruled out.
- There is no proven effective therapy, but patients typically remain stable, with a 40% spontaneous improvement rate.
- Low-dose aspirin may be beneficial in reducing the risk of fellow-eye involvement.
Is It Real?
Differentiating between true optic disc swelling and pseudo–optic disc swelling is important for avoiding unnecessary testing, Dr. Bhatti said. While papilledema is disc edema secondary to increased intracranial pressure, pseudopapilledema is a benign condition that is often due to optic disc drusen.
Critical finding. Swelling of the nerve fiber layer, which blurs the disc margins and the peripapillary vessels, is a hallmark of papilledema.1 Buried drusen also produce elevation of the disc and blurring of its margin but can be differentiated by lack of hyperemia, lack of disc surface microvascular abnormalities, and clearly visible retinal vessels at the disc margin.2 Ancillary testing such as ultrasound, autofluorescence, red-free photography, fluorescein angiography, or computed tomography may be necessary to differentiate pseudopapilledema from true papilledema, Dr. Bhatti said.
Most patients with pseudopapilledema have no visual symptoms, but this may be the case for some patients with true papilledema, too. Pseudopapilledema may be unilateral or bilateral, but many cases of papilledema are bilateral.1,2
Dr. Bhatti provided a quick reference for the features of papilledema and pseudopapilledema:
Papilledema. Findings include retinal nerve fiber opacification with obscuration of retinal blood vessels, disc hyperemia, loss of spontaneous venous pulsations (opening pressure >250 mm H2O in adults and >280 mm H2O in children), venous distension, hemorrhages, exudates, cotton-wool spots, circumferential retinal folds, and obliteration of the central cup.
Pseudopapilledema. Findings include anomalous branching pattern of blood vessels off the optic nerve, evidence of spontaneous venous pulsations, no obscuration of retinal blood vessels, no exudates, no cotton-wool spots, and, rarely, hemorrhages.
___________________________
1 http://eyewiki.aao.org/Papilledema. Accessed July 30, 2015.
2 http://eyewiki.aao.org/Optic_nerve_head_drusen. Accessed July 30, 2015.
|
Case 4
Acute Unilateral Vision Loss Without Pain
Courtesy of Valerie A. Purvin, MD
History and Examination
A 16-year-old boy presented with a weeklong history of painless loss of vision in his left eye. He was generally healthy; however, 3 weeks before his visual loss, he had developed muscle aches and a fever. This had resolved without treatment over the course of a week.
On examination, the VA in his left eye was 20/400. He also had markedly reduced color vision and a trace RAPD. VF testing in his left eye showed a large central scotoma, and the left optic disc was markedly swollen.
All findings in the patient’s right eye were normal, including the appearance of the optic disc, but there was a single chorioretinal white spot below the macula.
Further questioning revealed that the patient had recently acquired a kitten and that he had received several scratches while playing with it.
Clinical Course and Outcome
Two weeks later, the patient’s left optic disc edema had improved, but there were now hard exudates centered on the macula that formed a star figure. Review of his laboratory testing revealed elevated Bartonella henselae titers (IgG 1:1,024 and IgM 1:20).
Based on the patient’s clinical features and results of ancillary testing, we diagnosed cat-scratch neuroretinitis (NR). While his initial presentation was suggestive of “garden-variety” ON, there were a few clinical features that pointed to the correct diagnosis. First, the absence of eye pain would be unusual for ON, which is accompanied by pain in about 90% of cases. Second, ON is relatively uncommon in teenaged males, as it typically affects women between the ages of 20 and 35. Finally, the magnitude of his visual loss (large) was out of proportion to the RAPD (trace). This latter finding indicated that a large part of his visual loss was due to maculopathy rather than to optic nerve dysfunction, despite the prominent optic disc swelling. This combination of findings is quite typical for NR.
The patient received a course of ciprofloxacin (500 mg twice daily) for 10 days. Six months after onset, his VA had returned to 20/25, and his color vision and VF were normal. The macula showed some pigment irregularity; the appearance of the optic disc was normal.
Final Diagnosis
Cat-scratch neuroretinitis
Key Points
- NR is characterized by acute unilateral visual loss with central visual loss and marked optic disc edema. The characteristic macular star figure is distinctive but takes 9 to 12 days to develop.11-13
- Although NR may be caused by a number of infectious agents, in the United States, the most common cause is cat-scratch disease.
- Most cases of cat-scratch NR involve children or young adults and are preceded by systemic symptoms, including fever, sore throat, headache, and myalgias.
- The visual prognosis is generally excellent regardless of treatment. Even so, a course of antibiotics is often prescribed.
Quick Guide to the Differential Diagnosis
BILATERAL DISC EDEMA
Dr. Bhatti offered 6 M’s to remember:
- Malignant hypertension
- Mass (intracranial)
- Mucked-up drainage (venous sinus thrombosis, hydrocephalus)
- Medications (tetracycline, steroid withdrawal)
- Meningitis (cryptococcal)
- Morbid obesity (IIH)
UNILATERAL DISC EDEMA
- Neoplastic (optic nerve glioma, optic nerve sheath meningioma)
- Inflammatory (demyelination, sarcoidosis, systemic lupus erythematosus)
- Infectious (cat-scratch disease, syphilis)
- Metabolic/toxic
- Hereditary (Leber hereditary optic neuropathy)
- Ocular (uveitis, hypotony)
- Vascular (NAION, arteritic anterior ischemic optic neuropathy, perioperative anterior ischemic optic neuropathy)
|
1 Voss E et al. Ther Adv Neurol Disord. 2011;4(2):123-134.
2 Abou Zeid N, Bhatti MT. Neurologist. 2008;14(4):207-223.
3 Optic Neuritis Study Group. Arch Neurol. 2008;65(6):727-732.
4 Friedman DI et al. Neurology. 2013;81(13):1159-1165.
5 NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. JAMA. 2014;311(16):1641-1651.
6 Szewka AJ et al. J Neuroophthalmol. 2013;33(1):4-8.
7 Miller NR, Arnold AC. Eye. 2015;29(1):65-79.
8 Bilgin G et al. J Neuroophthalmol. 2013;33(3):232-234.
9 Newman NJ et al. Am J Ophthalmol. 2002;134(3):317-328.
10 Kupersmith MJ et al. J Neuroophthalmol. 1997;17(4):250-253.
11 Purvin V et al. J Neuroophthalmol. 2011;31(1):58-68.
12 Ghauri RR, Lee AG. Surv Ophthalmol. 1998;43(3):270-274.
13 Golnick KC et al. Am J Ophthalmol. 1994;118(2):145-151.
___________________________
MORE AT THE MEETING: “Case Studies on the Use of OCT for Diagnosis of Unknown Causes of Visual Loss” will cover using OCT to diagnose papilledema and pseudopapilledema. Presented Monday, Nov. 16, 9:00-11:15 a.m., in Sands Expo/Venetian, Murano 3205. Check www.aao.org/programsearch for full details.
Meet the Experts
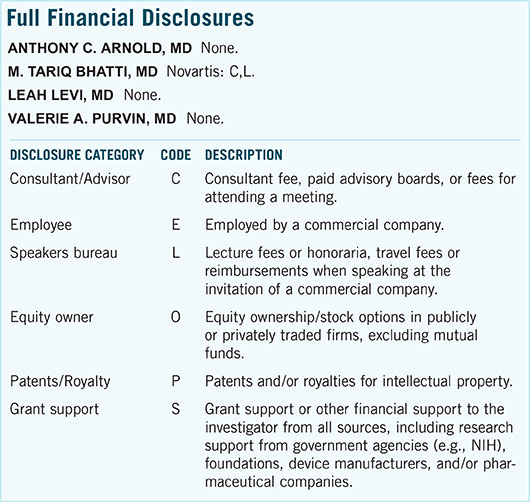
Anthony C. Arnold, MD Professor of ophthalmology and chief of the Neuro-ophthalmology Division at the Stein Eye Institute in Los Angeles. Relevant financial disclosures: None.
M. Tariq Bhatti, MD Professor of ophthalmology, professor of neurology, and chief of neuro-ophthalmology at Duke University in Durham, N.C. Relevant financial disclosures: Novartis: C,L.
Leah Levi, MD Director of neuro-ophthalmology at Scripps Clinic in La Jolla, Calif. Relevant financial disclosures: None.
Valerie A. Purvin, MD Clinical professor of ophthalmology and neurology at Indiana University Medical Center and chief of the Neuro-ophthalmology Section at the Midwest Eye Institute in Indianapolis. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
|