Download PDF
When it comes to the prevalence of age-related macular degeneration (AMD) and diabetic retinopathy (DR), all people are not created equal.
More evidence for this truism of ophthalmic epidemiology emerged recently when investigators in the Chinese American Eye Study (CHES) reported the results of extensive clinical examinations and retinal photography in more than 4,000 participants aged 50 and older.1,2 The CHES is the largest-ever ophthalmic study in Americans of Chinese ancestry, the authors wrote.
Participants were drawn from Monterey Park, Calif., a Los Angeles–area community with a sizable and stable population of Chinese Americans. A large majority of them were first-generation immigrants, primarily from mainland China.
Following are some key findings from this population-based cross-sectional study, which was funded by the National Eye Institute.
AMD results. The study detected 320 cases of any type of AMD, for an overall age-adjusted prevalence of 8.1% (95% CI, 7.2%-9.0%). Estimates of the disease prevalence in Chinese individuals living in urban and rural China and urban Taiwan range from 3.0% to 9.2%, suggesting that environmental or behavioral factors could be influencing AMD risk in Chinese Americans, said Rohit Varma, MD, PhD, chief investigator for CHES.
Early disease. In 306 of the cases, the disease was classified as early AMD, for an age-adjusted prevalence of 7.8% (95% CI, 6.9%-8.7%).
Advanced AMD. There were 14 cases of advanced AMD, for an age-adjusted prevalence of 0.4% (95% CI, 0.2%-0.6%). This is similar to the levels found in people of African descent by the Barbados and Baltimore eye studies and lower than what has been reported among Latinos and non-Hispanic white people, the researchers noted. Of the 14 advanced cases in CHES, 86% had neovascular AMD and 14% had geographic atrophy.
The influence of age. In an analysis of the data by 10-year age groups, the investigators found a direct correlation between older age and greater AMD prevalence. In all age groups, however, men had a higher rate of AMD than women. AMD prevalence ranged from 5.8% in subjects 50 to 59 years old to 17.6% in those 80 years or older. For the same 2 age groups, respectively, the prevalence rates were 9.8% and 32.4% for large drusen, 27.6% and 58.6% for soft drusen, and 4.1% and 7.2% for retinal pigment abnormalities.
Diabetes and retinopathy. Blood testing revealed that 736 participants (16.1%) had type 2 diabetes; 35.8% of this subgroup had DR (95% CI, 32.1%-39.6%). This compares to a 46% rate of DR previously reported among Chinese with type 2 diabetes in rural China, and 48% in Latinos living in Los Angeles, the CHES investigators wrote.
Participants with diabetes were 3 times more likely (6.7% vs. 2.2%; p < .001) than those without diabetes to have significant visual impairment, defined as best-corrected visual acuity worse than 20/40 in the better-seeing eye. The causes of the impaired vision were cataracts and macular edema.
Takeaway messages. “This study sounds a clarion call for all eye care providers to be aware of the higher relative prevalence of wet AMD compared with dry AMD in those of Chinese ancestry and to provide the available treatments such as anti-VEGF injections and laser therapies,” said Dr. Varma, director of the University of Southern California Roski Eye Institute. “And while [diabetic eye disease is] not as prevalent as we see in the Latino community, we also need to be aware of addressing those Chinese Americans with diabetes to prevent diabetic retinopathy and the onset of significant visual impairment.”
—Linda Roach
___________________________
1 Varma R et al. JAMA Ophthalmol. Published online April 7, 2016. doi:10.1001/jamaophthalmol.2016.0588.
2 Varma R et al. JAMA Ophthalmol. Published online April 7, 2016. doi:10.1001/jamaophthalmol.2016.0445.
___________________________
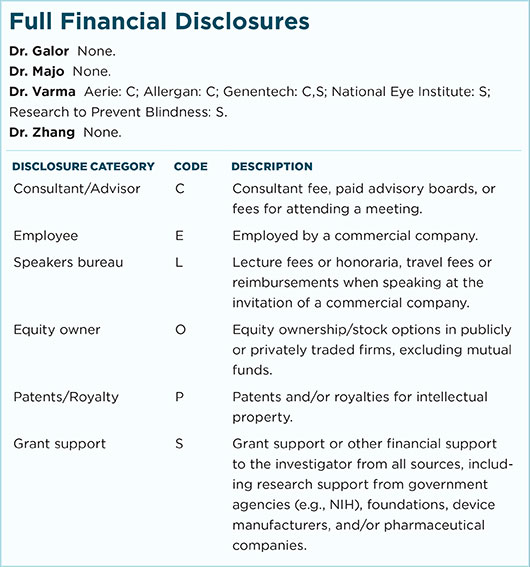
Relevant financial disclosures: Dr. Varma—National Eye Institute: S.
For full disclosures and disclosure key, see below.
More from this month’s News in Review