Download PDF
Although corneal perforations can be challenging even for seasoned experts, many treatment options are available. A personalized approach, based on the cause of perforation, is key to successful management.
Corneal perforations are ocular emergencies with myriad causes, such as trauma, infection, autoimmune diseases, and loss of corneal innervation. Knowledge of the cause of the perforation is essential for its proper management. Corneal perforations are different from corneal lacerations in that tissue loss is part of the equation, making their treatment more complicated, explained Sonal S. Tuli, MD, at University of Florida, Gainesville.
Whenever possible, of course, the focus should be on early and aggressive prevention. However, multiple medical and surgical interventions are available once the perforation has occurred.
Diagnosing the Perforation
In most cases, the presence of a corneal perforation is unambiguous.
Classic signs. Carol L. Karp, MD, at Bascom Palmer, described the hallmarks of corneal perforation: a perforation site along with shallowing or flattening of the anterior chamber. In addition, aqueous leakage may be observed. The patient may report recent trauma, or there may be an obvious infection or corneal melt from a peripheral or central ulcerative keratitis. Symptoms usually include vision loss, some pain, and leakage that may be mistaken as tears.
Leakage. Occult perforation should be suspected if the patient says, “All of a sudden, I started tearing a lot. It comes and goes,” said Elmer Y. Tu, MD, at the University of Illinois at Chicago. However, some perforations don’t appear to leak. For these, the Seidel test can be helpful. Concentrated fluorescein (formulated as drops or a dye strip) is applied to the eye. On slit-lamp examination with cobalt blue light, dilution of the green fluorescein by aqueous leakage becomes visible as blue fluid cascading down the eye. The experts also suggest applying gentle pressure on the globe with a finger to see if aqueous egress can be induced. Dr. Tu explained, “You may measure the pressure in the eye and it’ll be kind of low—maybe under 10 mm Hg—but there’s no obvious leak. What’s happening is that the leak is pressure dependent and you need to challenge the eye to reveal it.”
Pigment in the wound. Another telltale sign of corneal perforation is brown pigment from the iris in the wound itself. “The iris is like the omentum of the eye,” said Dr. Tu. “It’s a floppy tissue, and any time there’s an exit of fluid from the eye that’s anywhere near the iris, the iris will move toward it and plug the hole.” A clinician can be fooled when he or she sees some pigment but everything else looks normal inside the eye. “It usually means that the iris had been drawn up to the area, left a mark behind indicating that some fluid had escaped there, and then fell back later,” said Dr. Tu.
Infected tissue. In some cases, diagnosing a perforation can be more challenging. The site may be obscured by necrotic or edematous tissue. “In the setting of an infectious corneal ulcer, for example, everything may be white. It’s difficult to judge what’s happening because you can’t see well into the eye,” said Dr. Karp.
Keys to Management
Dr. Tuli described 2 main management goals: treat the cause and reconstitute the globe.
Treat the cause. Deepinder K. Dhaliwal, MD, LAc, at the University of Pittsburgh School of Medicine, emphasized that “you have to differentiate the cause of perforation before you can make any treatment decisions. Perforations from infectious corneal ulcers or autoimmune disorders are usually more difficult to treat than those caused by trauma, which are typically amenable to standard surgical repair.”
Dr. Tuli added, “One of the ways to distinguish autoimmune disorders from other causes is their location, which is almost always peripheral. In addition, the edges are often overhanging as opposed to sloping or sharp.”
When the cause of a perforation is trauma, Dr. Karp advises clinicians to check both eyes for additional perforations, a foreign body, or another type of injury. “For nontraumatic perforations as well, always examine the other eye, especially if the etiology appears to be autoimmune,” she added.
Reconstitute the globe. Treatments for corneal perforations run the gamut from short-term fixes to long-term repair. “The optimal approach depends on the cause, size, location, degree of stromal involvement, and potential visual effects,” said Dr. Tuli, “Multiple treatments are often used simultaneously or in a staged fashion.”
Medical Treatments
“In all cases, optimize healing while taking care of the underlying cause,” said Dr. Dhaliwal.
Autoimmune tx. For instance, Dr. Dhaliwal said, if the cause is an autoimmune condition, the patient needs systemic workup and management. Dr. Tuli noted that she will put these patients on high-dose oral steroids and refer them to a rheumatologist for more definitive systemic immunosuppressive treatment.
Infection tx. For patients with an infectious ulcer, it’s essential to identify and eliminate the causative agent and treat the patient aggressively with topical antibiotics. Except for very small, noncentral ulcers, Dr. Tuli said that commercially available antibiotic drops are usually not enough. She has a compounding pharmacy make more powerful antibiotics that broadly cover the majority of infectious organisms typically seen in corneal ulcers. The ulcers are also cultured to determine the causative organism so that targeted antibiotics can be used.
Ocular surface tx. “If there’s an ocular surface problem, like severe dry eye, we are really aggressive about plugging the puncta with thermal cautery, using autologous serum drops to help the cornea heal, perhaps using a bandage contact lens or amniotic membrane, and fixing poor lid apposition with a tarsorrhaphy,” said Dr. Dhaliwal.
Promoting corneal healing. To optimize healing, every patient with a corneal melt or perforation seen by Dr. Dhaliwal and Dr. Tuli is treated with oral doxycycline to inhibit collagenase and oral vitamin C to facilitate collagen synthesis.
For a microperforation (less than 0.5 mm diameter), Dr. Tuli recommends aqueous suppressants to promote healing. “Just like any other fistula, a corneal perforation will not heal as long as fluid is flowing through it,” she said. “Using aqueous suppressants will decrease the intraocular pressure and may stop fluid flow through a small perforation, allowing it to heal spontaneously.”
Observation. In the absence of abundant, spontaneous leakage and if the anatomy of the eye is otherwise intact (e.g., the iris and lens are in their normal locations), the experts indicate that close observation and broad spectrum topical antibiotic coverage may be the best option. In these cases, the cornea can heal spontaneously, as there is minimal to no tissue loss. Following the patient daily for the first few days is necessary to ensure that the cornea does not begin to leak later.
Causes of Corneal Perforation
I. Trauma
A. Extrinsic
1. High-velocity projectiles
2. Fishhooks
B. Iatrogenic
1. Removal of corneal foreign body
2. Surgical complications
II. Keratitis
A. Infectious
1. Gram-negative bacteria (most common)
2. Fungal keratitis
B. Noninfectious
1. Neurotrophic keratitis
2. Peripheral ulcerative keratitis
3. Rosacea-related blepharokeratitis
III. Degenerative disorders
A. Pellucid marginal degeneration
B. Terrien marginal degeneration
IV. Dystrophies
A. Keratoglobus
B. Peters anomaly
—Courtesy of Sonal S. Tuli, MD
|
Surgical Treatments
Glue. If the perforation is less than 2 mm in diameter, the experts recommend tissue adhesive or glue. Dr. Karp uses cyanoacrylate glue with a contact lens on top. “When I glue, I always cover the cyanoacrylate with a soft contact lens because the surface is rough and very uncomfortable for the patient,” she explained. This also prevents friction, caused by blinking lids, from dislodging the glue.
When gluing a perforation, the surgeon uses 1 of 2 basic techniques, depending on the structure of the area, according to Dr. Tuli.
- With tissue loss. If the perforation involves loss of surrounding tissue, the crater can be directly filled with glue. “Care must be taken to underfill the crater because the glue expands when it polymerizes,” Dr. Tuli emphasized. “Too much glue would result in an elevated mass, which is uncomfortable for the patient and prevents the contact lens from fitting well.” Likewise, touching any wet glue with an instrument or a Weck-Cel can pull away a hardened strand of glue. This strand, like an elevated mass, can cause discomfort and prevent the contact lens from fitting properly.
- Without tissue loss. To treat a perforation without much surrounding tissue loss or with iris prolapse from the opening, a modified technique must be used. Dr. Tuli uses a 2- to 3-mm skin punch to cut a disc of sterile drape and places this on the wooden end of a cotton-tipped applicator. A very small amount of glue is placed on the drape, after which the drape is inverted and pressed onto the perforation. This allows the drape to adhere to the periphery of the perforation and seal it shut without creating an elevated mass.
Dr. Dhaliwal emphasized that the cornea must first be dried with either a cotton-tipped applicator or a surgical sponge spear. “You want to take a Weck-Cel in one hand and the glue in the other hand. As you move the Weck-Cel out of the way, try to apply the glue right away on to the corneal surface,” she advised. Dr. Tuli explained that “since fluid causes the glue to polymerize, a wet wound will solidify the glue before it can adhere to the perforation. Ideally, the glue should polymerize slowly in the perforation by using the traces of moisture in the surrounding tissues and adhere strongly.”
Pedicle conjunctival flap. In small, peripheral perforations, another option is to suture a pedicle conjunctival graft to tamponade the hole. Dr. Tuli finds this especially useful in nonhealing, neurotrophic ulcers, which are associated with low levels of growth factors in their tear film. The flap’s fibrovascular tissue covers the area, not only providing serum growth factors to help with healing but also preventing infection.
Dr. Tuli creates a flap of conjunctiva that has a feeder blood vessel. After removing the epithelium from the area around the ulcer and the adjacent limbus, she sutures the conjunctival flap to the denuded area.
Amniotic membrane. According to Dr. Tu, amniotic membrane can be useful for nontraumatic corneal perforations with loss of stroma, small perforations, impending perforations when the stroma melts away without a catastrophic entrance into the eye, and descemetoceles. Amniotic membrane is particularly helpful for reconstructing the eye surface when the pattern of tissue loss involves irregular borders or depths. “Amniotic membrane is very easy to shape to the area of tissue loss, and multiple layers can be used to create a smooth surface that will eventually integrate so that you don’t have to use donor corneal tissue,” Dr. Tu explained. You can glue or stitch the amniotic membrane in place. Dr. Tu usually uses a combination of these.
Grafts and transplants. With transplantation, the biggest challenge for the surgeon is to adapt donor tissue so that it fits properly at the recipient site and won’t result in leakage from the edges of the wound. Dr. Tu recommends the following general approach: “Try to make a circular excision large enough to get you into the healthy tissue and then fill it with round donor tissue. If you can get a round peg in a round hole, you’re in good shape.”
For a small perforation outside the visual axis, Dr. Dhaliwal prefers a small patch graft (3 mm in diameter or smaller). With a round dermatologic punch, she removes a section of tissue encompassing the perforation and then debrides the melting cornea to create a clean bed for the graft.
Penetrating keratoplasty (PK). This is the most common procedure for sealing nontraumatic perforations, according to Dr. Tu. PK is essential for treating large perforations as well as small perforations that are surrounded by large areas of tissue necrosis. “You’re typically looking at a catastrophic failure of the cornea, meaning there’s a large hole where you’re unable to keep the anatomy of the eye normal for even a short time, so you’ll need to remove unstable tissue, then replace it,” said Dr. Tu.
Dr. Karp said that PK is the best option to eliminate active infection or to treat a perforation larger than 2 mm that involves tissue loss, or when a lamellar transplant would require cutting or suturing through the visual axis.
- Peritomy. Dr. Tu pointed out that a periotomy should be performed in the presence of an infected ulcer or a condition necessitating transplantation close to the limbus. “You need to take down all the conjunctiva in the area that you plan to either transplant or sew into. Many people will make the mistake of not taking that down,” said Dr. Tu. Typically, the eye is so inflamed that it is necessary to suture through the sclera and conjunctiva to secure the graft. “If you don’t do a peritomy, invariably the transplant will become loose later on because the sutures can’t be tightened over the conjunctiva as well as they should be, and you can’t suture into the sclera where you need to anchor it,” said Dr. Tu. “People end up with loose transplants that need to go back for repair, and that’s usually a disaster.”
- Preserve the limbus. For perforations that require large transplants, the corneal transplant must be designed to maximize preservation of the limbus, said Dr. Tuli. It may be necessary to position the graft off center so that it extends to the limbus in the affected area but preserves maximal host cornea on the opposite side. “This will maintain 2 structures that are crucial for the long-term prognosis of the eye: the limbal stem cells and the trabecular meshwork,” Dr. Tuli said.
Lamellar transplants. Whenever possible, cornea specialists prefer lamellar transplantation to PK because the likelihood of rejection is much higher with a full-thickness graft. (Endothelial rejection is the strongest trigger of failure, according to Dr. Karp.) Rejection is more likely to occur if the transplant site is actively infected or inflamed. When the eye is red-hot from infection, full-thickness grafts are likely to fail, noted Dr. Karp.
If a perforation is larger than 2 mm and involves only partial stromal loss or if the patient can’t tolerate gluing, Dr. Karp advocates lamellar keratoplasty. This approach is better for the patient because “you’re transplanting only stroma. You’re basically providing tectonic tissue reinforcement without implanting any endothelium,” she said.
Dr. Dhaliwal suggests “trephining down to the depth that you intend. If you’re doing a deep lamellar kerato-plasty, you trephine down maybe 80% of the corneal thickness. Start hand dissection in a lamellar fashion and just peel away layers of the cornea starting from the healthy cornea and moving into the perforated area. You can dissect from all different directions.”
In some cases, the melting can create a descemetocele. “You don’t have to dissect down to Descemet’s membrane with deep lamellar keratoplasty, as long as the etiology is not infectious (for example, if it’s a rheumatoid melt). You just want to get to a plane that you can sew into,” she said. Dr. Dhaliwal prefers a crescent blade to remove layers during lamellar dissection because the blade has to be very sharp, given the lack of counterpressure. “At the end of the day, you’re going to put the lamellar cornea on top. If you have to come back, you can later on. That’s the beauty of a lamellar transplant: You can repeat it more easily and with less risk than a penetrating keratoplasty,” she said. Of course, infected corneal tissue must always be removed completely.
- Size the tissue. “Lamellar grafts require more surgical ingenuity because you have to get a piece of donor tissue that is appropriately shaped and sized to match the defect that you have,” Dr. Karp said. This is particularly challenging when there’s a peripheral corneal melt at the limbus, and a crescent-shaped graft is required. “It takes some trough lining and creative cutting,” Dr. Karp said. In such cases, she usually creates a “stencil” by copying the recipient shape onto a sterile piece of paper and outlining this shape onto the donor globe or button. She cuts the donor tissue bigger than the shape needed and trims it once it’s placed on the recipient site. When cutting a donor button for a lamellar graft, an artificial anterior chamber is helpful.
- Central cornea: keep it clear. “If your patient has an eccentric perforation or a small peripheral laceration, try to keep the transplant peripheral and away from the visual or pupillary center of the cornea,” advised Dr. Tu. If a small peripheral transplant fails, it’s not visually significant; the patient can still see through the center of his or her cornea and won’t have any visual deficit. On the other hand, if you need to cut or suture through the center of the cornea to close a perforation, then a larger transplant that encompasses the entire center of the cornea would be preferable. Dr. Tu cautioned that anything crossing the middle of the visual axis will have significant visual consequences in terms of astigmatism, opacity, and irregularity.
- Older, alternative tissues are OK. For centers that have difficulty procuring a fresh globe or fresh tissue in an emergency, Dr. Karp pointed out that cornea in glycerin is an excellent alternative that has a long shelf life and can be obtained from an eye bank.1 For a tectonic lamellar procedure, fresh endothelium is not necessary. Instead, older tissue (i.e., tissue that’s not viable for endothelium transplantation) or glycerin-preserved cornea can be used. The latter is “almost like a rubbery piece of tissue that, in some ways, is even a little easier to dissect than a partial-thickness corneal piece,” said Dr. Karp. Irradiated sterile cornea also has a long shelf life and is applicable to nonendothelial procedures.2 It’s also possible to temporarily transplant other types of banked tissue, such as pericardium.3 Such tissue can seal the eye for a few days until a replacement cornea can be obtained, said Dr. Tu.
- Surgical strategies. When treating perforation with tectonic transplantation, corneal dissection can be difficult because the eye is structurally similar to a squished grape. “If an eye is soft, it’s very difficult to hold the eye in shape while you’re cutting it because there’s no back pressure,” said Dr. Tu. The goal is to reestablish the structure of the eye and restore some back pressure. “You can inject viscoelastic or put an air bubble in the anterior chamber. There are even reports4 of surgeons placing fibrin glue in the anterior chamber to seal the perforation while they’re working,” said Dr. Dhaliwal.
Management of Perforations
Medical
I. Treat underlying cause
II. Protease inhibitors
A. Tetracyclines
B. Vitamin C
III. Antibiotics (topical and/or systemic)
IV. Steroids (used very cautiously in select cases that have significant inflammation)
V. Aqueous suppressants
Surgical
I. Traumatic
A. If mostly linear and minimal loss of tissue, primary closure may be attempted using sutures
B. High risk of leaks and gapes
C. Significant postoperative astigmatism may occur
II. Microperforations
A. May seal spontaneously
B. Bandage contact lens to tamponade (tight lens)
C. Pressure patching may help
D. Amniotic membrane graft
III. Perforation with the iris plugging, or prolapsed from, the perforation
A. Recent (within 48 hours)
1. Reposition iris
2. Tamponade perforation with air bubble
3. Glue
B. Older
1. Leaking around iris
a. Glue with sterile plastic drape circle
2. Not leaking
a. Usually has fibrin overlying
b. Will heal with iris adherent
c. Option of observation
IV. Small perforations (2-3 mm in diameter)
A. Peripheral
1. Gluing as definitive procedure
a. Cyanoacrylate glue is preferable
i. Simple gluing
ii. Gluing with sterile plastic drape
2. Pedicle conjunctival flap
a. Especially in neurotrophic ulcers
b. Allows fibrovascular tissue to cover area
c. Provides serum growth factors
3. Amniotic membrane grafts
a. Multilayer or pleated
b. Decrease inflammation (theoretically)
c. Sutured or glued in place
4. Patch grafts
a. Small circular
b. Crescentic
c. Other shapes
B. Central
1. Gluing as temporizing measure
2. Definitive treatment corneal transplant
V. Large perforations
A. Emergent corneal transplantation (good anatomic success but poor optical success)
B. Lamellar versus full thickness
1. Fresh corneal tissue
2. Cryo, glycerin, or irradiation preserved
—Courtesy of Sonal S. Tuli, MD
|
Preventing Perforation
If you suspect an impending perforation, bear in mind that it’s much easier to repair an eye before it opens up. If a patient’s cornea is becoming progressively thinner, Dr. Dhaliwal warns against waiting for a descemetocele. “Refer earlier! If you’re a cornea specialist watching a thinning cornea, glue early. As it’s thinning, put a thin layer of cyanoacrylate glue or amniotic membrane with fibrin glue at the base; be aggressive,” she said. “I’ve become much more aggressive in patients whose corneas are thinning, and I’ve been very happy with the multilayer amniotic membrane with fibrin glue approach.”
___________________________
1 Chen W et al. Invest Ophthalmol Vis Sci. 2010;51(2):775-781.
2 Utine CA et al. Am J Ophthalmol. 2011;151(1):170-174.
3 Yoo C et al. Ophthalmic Surg Lasers Imaging. 2011;42(6):E1-E3.
4 Por YM et al. Cornea. 2009;28(4):451-455.
Meet the Experts
DEEPINDER K. DHALIWAL, MD, LAC Professor of ophthalmology; director of the cornea, external disease and refractive surgery services; director and founder of the Center for Integrative Eye Care; director of the University of Pittsburgh Medical Center Laser Vision/Aesthetic Center; associate director of the Charles T. Campbell Ocular Microbiology Laboratory; and director of the cornea and refractive surgery fellowship at the University of Pittsburgh School of Medicine. Relevant financial disclosures: None.
CAROL L. KARP, MD Professor of ophthalmology and Richard K. Forster Chair in Corneal Diseases, Bascom Palmer Eye Institute at the University of Miami Miller School of Medicine. Relevant financial disclosures: None.
ELMER Y. TU, MD Associate professor of clinical ophthalmology and director of the cornea service at the University of Illinois at Chicago. Relevant financial disclosures: None.
SONAL S. TULI MD Professor and chair of ophthalmology, director of the cornea and external diseases service, and residency program director at the University of Florida, Gainesville. Relevant financial disclosures: None.
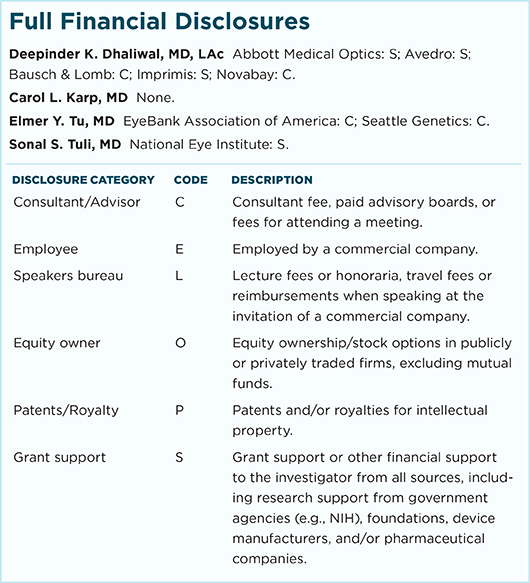
For full disclosures and the disclosure key, see below.
|