By Joel S. Schuman, MD, with Louis B. Cantor, MD, and Dale K. Heuer, MD
Introduction by Kurt F. Heitman, MD, Academy Secretary for State Affairs
Download PDF
Sparked by a new study born of concerns about patient care and scope of practice, a discussion among 3 glaucoma experts looks at the clinical nuances of an important surgery.
For approximately 50 years, optometrists have been campaigning to increase their scope of practice nationwide. Because they do not have a plenary license, they must go to the legislature in each of their states to gain new privileges. Some of these privileges involve surgery. Today, 3 states—Oklahoma, Kentucky, and Louisiana—have optometric surgical authority that includes laser, scalpel surgery, and injection. A few other states have limited optometric surgical authority, mostly injection.
Since 1998—when Oklahoma became the first state to grant laser surgical privileges—some form of ophthalmic-related surgical scope legislation has been proposed in more than 40 states. Such legislation is often justified as an access-to-care issue, with optometrists asserting that there is a substantial need to expand their scope of practice because there simply are not enough ophthalmologists to address the need. In some instances, optometrists have framed it as a cost issue—that they can perform surgery less expensively than ophthalmologists. Or they may state that they are as well trained as ophthalmologists, so they should be granted these privileges.
To analyze the Oklahoma experience, Joshua D. Stein, MD, at the University of Michigan, and several of his colleagues undertook a Medicare claims data study with a grant from the Academy.
The first paper to come from those claims data (see “Landmark Study”) contrasts laser trabeculoplasty (LTP) performed by optometrists with LTP performed by ophthalmologists and reveals a difference in usage of this procedure. It was accompanied by two editorials, one by Alan Robin, MD, and another by Murray Fingeret, OD.
These new data shed light on cost and utilization issues and raise important clinical questions of interest to ophthalmologists and optometrists alike. This study is the basis for a thoughtful discussion among 3 leading glaucoma specialists.
Common Practice
Dr. Schuman: Let’s start with LTP itself. What would you say is generally accepted practice for LTP in glaucoma?
Dr. Cantor: For initial LTP, argon laser trabeculoplasty (ALT) and selective laser trabeculoplasty (SLT) have equal efficacy. Which laser you use first is not critical, although most ophthalmologists in the United States use SLT.
In terms of treatment parameters, 180° or 360° treatment of the trabecular meshwork is acceptable. Most of the evidence suggests that with SLT, a 360° treatment is more effective, and that’s what I do in the overwhelming majority of patients. Although treating 360° is the norm, there is nothing wrong with fractionating the treatment if indicated in an individual patient.
Dr. Heuer: I have shifted almost exclusively to SLT, in large measure because of the hope—which has some early support—that we will have better procedures that may involve Schlemm’s canal. ALT seems to cause collateral damage there, whereas SLT causes little, if any, such damage.
With SLT, I do 360° treatment except in patients with advanced glaucoma (where, frankly, I’m usually inclined to go straight to trabeculectomy). In the vast majority of mild to moderate glaucomas, if you’re in for a penny you’re in for a pound, so go 360°.
In a handful of patients with advanced glaucoma who may be infirm, elderly, or have other conditions that make incisional surgery difficult—and who may need only a couple points lower IOP—I may do a 180° SLT, primarily to reduce the risk of an undetected elevation in pressure. In patients in whom I have done 180°, I feel obligated to wait to see its effect. Although a 360° is usually more effective, a 180° treatment will often reduce the IOP to target, allowing me to reserve the other 180° for the next time I might need a little additional IOP reduction. Therefore, I was somewhat surprised by the data in the Stein study, showing how frequently second treatments were being done by optometrists.
Dr. Schuman: The efficacy of SLT and ALT is the same, and the literature bears that out. But with ALT you get much more damage to the tissue than you do with SLT. There doesn’t seem to be significant harm in re-treating with SLT as many times as necessary, whereas we know that re-treating with ALT can result in a permanent and sudden pressure increase, even requiring emergency surgery in the operating room.
Variation From Norm?
Dr. Schuman: Do you think that the study by Stein et al., comparing numbers of LTP sessions performed by optometrists versus ophthalmologists, describes a variance from the standard that we all just discussed? Also, what are your thoughts on the editorial from Murray Fingeret, in which he says that all of the optometrists during the study period were trained in a single institution that was instructing its students specifically to treat only 180° at a time?
Dr. Heuer: We have to be careful when we use the term standard of care, which tends to have medicolegal implications. It is entirely within the standard of care to treat 180° and then treat the other 180°. If that is going to be the approach, however, treating the second 180° should be driven by the clinical indication of inadequate IOP reduction. The data from the Stein study suggest that retreatments—or the second treatments—were being done before it was even possible to know if the first 180° treatment had had an adequate effect.
It often takes 6 to 8 weeks to see the full effect of LTP, whether it has been done with argon or with the frequency-doubled Nd:YAG laser, the selective approach. Treating the second 180° before you even know how much IOP reduction your first 180° achieved would be similar to prescribing an ocular hypertensive patient an initial glaucoma medication at one visit and then prescribing a second glaucoma medication without an intervening visit to assess the efficacy of the first medication. It doesn’t make good medical sense.
Although I accept Murray Fingeret’s suggestion that this pattern is related to the training provided to all of the Oklahoma optometrists in this study, I would suggest 2 things: 1) The training itself needs to be revisited. 2) The timing between the treatments should have been discussed in that training, specifically recommending at least 6 and, ideally, 8 weeks between treatments to adequately assess the effect of the first 180°.
Dr. Cantor: Certainly, common practice and the evidence suggest that there is a time period of 4 to 6 weeks before which you cannot assess the effect of any LTP, whether 180° or 360°. The claims data would suggest that a very high percentage of second laser treatments by optometrists were done very early, in an 11- to 30-day window. This leaves open several questions that we can’t precisely answer based on the study, including why the second laser was being done that early.
Pressure Spikes
Dr. Schuman: Is it possible that the second lasers were being done within that time period because the risk of a pressure spike may be a little bit lower if you split treatment into 2 sessions?
Dr. Cantor: From a historical perspective, 20 or 30 years ago, we used to see a lot more pressure spikes when we were primarily using ALT. That was when we really didn’t have a good handle on how much energy to use and probably used higher energies than necessary. We subsequently learned how the treatment effect could be obtained with lower energies with ALT and, more recently, with the SLT. The risk of pressure spikes has really declined; although they can occur, they are infrequent.
As Dale alluded to, in those really advanced patients, if you’re worried enough about a pressure spike from laser, you’re probably doing the wrong procedure. You should be in the operating room.
But there may be some cases where, because of patient preference or other circumstances, you try to do everything short of [incisional] surgery. Certainly, LTP is a reasonable treatment in that setting. Pressure spikes could be a concern, but I think that the risk is relatively low.
Dr. Schuman: It does seem like the old ALT model was being taught [in the optometry school], in that we always try to balance risk and benefit. With ALT it used to be that it was a scary thing to do 360° because that patient may have a pressure spike, but now with apraclonidine, as Alan Robin pointed out, that risk is extremely low as well.
Alpha Agonists
Dr. Schuman: Do you use alpha agonists when you do laser?
Dr. Cantor: If the pressure is high enough that you’re worried about it, doing pretreatment with an alpha-2 agonist or other medications and then post laser treatment with the same medication, and monitoring in the office can minimize the pressure spikes from laser.
Dr. Heuer: One additional patient group in whom 180° treatment, even with alpha-2-adrenergic pretreatment, is prudent is patients with pigmentary glaucoma with very dense trabecular meshwork pigmentation. Such patients have been noted to have a risk of pressure spike even with SLT. But given the minimum age of 65 years and average age of 77 years for the Stein study participants, pigmentary glaucoma patients would not be expected to have comprised a substantial number of patients in this study.
Repeat Laser
Dr. Schuman: The study data show that 3 years after the initial treatment, the proportion of eyes having multiple lasers was 34% for the ODs and 18% for the MDs. Does this matter? Is it a bad for the patient to have multiple LTPs? Is there an increasing risk of complications as the number of treatments go up?
Dr. Heuer: If argon laser was being used, there is certainly a greater risk of pressure increases with repeat thermal laser treatment.
Otherwise, the disadvantage to the patients, to family members who drive them to their surgeries, and to society include the additional economic burden related to traveling, missed work, missed personal time, as well as the extra cost of the repeat procedure itself. As we increasingly consider constrained health care spending, we need to think wisely about where to use those scarce dollars, such that doing 2 treatments instead of 1 in the absence of a known risk really is not prudent.
Dr. Cantor: There is some risk to LTPs. You can have a corneal abrasion, inflammation, and hyperemia. Photophobia and headache can follow laser. There have even been rare reported cases of iritis following laser, and reports of corneal haze and clouding. So, as with any therapy, you want to do the least amount of treatment to achieve the desired effect. Limiting the number of laser sessions can certainly minimize some of the side effects.
Dr. Schuman: I suppose one could argue that doing 180° and waiting to see if the patient is going to respond may be doing the minimum amount. But since the optometrists’ second treatments were done so soon after the first, it would be difficult to make that argument.
Dr. Cantor: And there is another evolving common practice in glaucoma: to get to the target IOP quicker. We can spend a lot of time trying different treatments with medications or laser. Meanwhile, the patient’s glaucoma is not adequately controlled and is progressing.
Doing a 360° treatment and knowing that in a 4- to 6-week time window we will know whether laser is effective allows us to assess whether we’re now at target or whether we need to go to the next step. The next step is generally scalpel surgery, unless laser has been used in place of medications or as a primary therapy.
Wait Times After Initial Tx
Dr. Schuman: How long do you usually wait after your LTP to determine if there’s an effect?
Dr. Heuer: I usually wait 6 to 8 weeks because I’ve seen it take that long to achieve its effect. Certainly, if a patient were very marginal, and I had done the laser more because of patient preference to avoid scalpel surgery, and if I haven’t seen any effect in 4 weeks and I’m up against a wall, I might repeat treatment at 4 weeks. But my sweet spot is about 6 weeks, and I’ll usually procrastinate till 8.
Dr. Cantor: I do a 360° treatment and, as a standard, generally see patients approximately 4 weeks later. If there’s zero effect at 4 weeks, I’ve found it very unlikely that the IOP is going to improve subsequent to that time period. If the pressure is down some, and it looks a little bit better though maybe we’re not quite at target, I will check it again in another month.
Dr. Schuman: I usually wait at least 6 to 8 weeks, and the literature supports this. But I sometimes wait as long as 3 months because there has been the occasional patient who is a late responder, and it’s always nice when the treatment effect kicks in. But if you’re pushed to the wall, obviously you have to treat sooner.
Primary LTP
Dr. Schuman: Can we discuss primary LTP? Do you see support in the literature for the use of LTP as a primary modality for glaucoma treatment? Have you seen an increase in primary LTP in your own practice or the practices of others around you?
Dr. Heuer: Reflecting back to when the Glaucoma Laser Trial [GLT] results were first presented at the American Academy of Ophthalmology meeting, I was surprised that half the audience didn’t get up, walk out to the exhibit floor, and buy a laser immediately after Hugh Beckman completed his presentation.
It has always been mystifying to me that, as enamored as ophthalmologists are by technology and the public seems to be by “laser” treatments, LTP has not achieved more traction as primary treatment, particularly given that we have good evidence that it is fairly effective. It is relatively comparable to—though not quite as potent as—the prostaglandin analogues as initial therapy. There are some economic analyses that suggest that it is also cost-effective vis-à-vis initial medical therapy.
I certainly offer it to my newly diagnosed glaucoma patients, but I don’t see a lot of those; I tend to see the other end of the spectrum. Nonetheless, it is remarkable that—and perhaps I unconsciously project my traditional approach of trying a drop first—vanishingly few patients take the laser approach, maybe 1 in 10 in my practice. It just does not get a lot of uptake.
Dr. Schuman: What interests me is that the evidence is there, in the Glaucoma Laser Trial, in the SLT trial that Jay Katz ran, and in other studies, that primary LTP works just as well as medical treatment. In fact, in the GLT there was better visual field preservation with the use of LTP first [compared with timolol 0.5% first]. With SLT, because the risk is so low, I’ve switched over to using laser as first-line treatment that I recommend for my patients. It’s what I’d want if I had glaucoma.
But I guess how you speak to your patients determines what their decision is, and I’ve noticed little resistance to SLT as first line. What I’m seeing at meetings is that more people are going to SLT as their first-line treatment for glaucoma. That last part is anecdotal obviously.
Dr. Cantor: Even if we’re not talking about primary laser treatment, I think that there is greater acceptance of LTP earlier in the treatment—maybe after 1 medication or 2—so that we don’t have to go to maximum tolerated medical therapy. There is a trend toward earlier laser treatment because of all the compliance and cost issues that we have with medical therapies.
Trend Toward Repeat Laser?
Dr. Schuman: If the number of LTPs increases as it is used more commonly as first-line therapy, are you concerned about multiple laser treatments if the trend seen among the ODs in the study continues in the same direction?
Dr. Cantor: Yes, if the use of LTP were to increase, especially if it follows the same trend in other states as in Oklahoma, that would raise concerns about patients getting more laser than indicated, with the additional burdens on the health care system in dollars, cost, and inconvenience for the patients.
Study Limitations
Dr. Schuman: Are the OD editorialist’s arguments valid, especially with regard to the study limitations? Do you think that further studies should be undertaken to better understand the differences in the quality of care between ophthalmologists and optometrists in Oklahoma?
Dr. Heuer: The study authors also pointed out the limitations. There are data that we would all love to see, such as severity of disease, treatment parameters, and preoperative and postoperative pressures.
Even without these specifics, some of the study findings are hard to explain, not the least of which is the relative frequency of second treatment by the optometrists vis-à-vis the ophthalmologists. From my perspective, the retreatment within 4 weeks—and just outside the global period, by the way—tends to implicate financial issues rather than medical issues. It is really hard for me to understand how anyone could justify retreatment in that short time period.
Dr. Cantor: In deference to Murray, he’s right, this really isn’t an outcome study per se. It’s utilization data. It’s not the type of Level I evidence that would stand up to a Cochrane type of study, but it does raise a lot of questions, as most studies do.
To answer your question, would it be great to have more data and further studies? Absolutely. Any data that marries the claims data in terms of any clinical data—if that’s possible—would be very interesting to see and to learn from. I think everybody, ophthalmologists and optometrists, would want to know that.
In today’s era, we want to look at treatments through every different lens to see not only whether it’s effective in individual patient disease but also what the cost is, how it is utilized, and what its impact is on the health care system and our ASC cost structures. These issues are relevant and are raised by the study.
More at the Meeting
Learn how the Surgical Scope Fund works with state ophthalmological and medical societies to ensure patient safety and surgical standards; write a letter to Congress; or get a summary of legislative issues. Visit the Advocacy desk in the Academy Resource Center in Booth 508. Or you can go to aao.org/advocacy.
|
Study Conclusions
Dr. Schuman: Murray Fingeret ends his first paragraph saying that the conclusions of Stein et al. are misleading and not supported by their data. Is that an accurate statement? If not, why not?
Dr. Heuer: Well, certainly from Murray’s perspective I understand that statement; however, I think the study’s authors were very circumspect and tried not to draw unsubstantiated conclusions from the data.
I am pleased that Murray is pointing to the Academy’s Preferred Practice Patterns (PPP). I think we need to revisit them and be more explicit—based on new data—about the relatively infrequent indications for split treatment. We may need to emphasize the role of LTP in initial treatment or earlier treatment. There are teaching points not only for the optometrists but also for ophthalmologists who may not be as immersed in the literature as the 3 of us are. I think the study authors and Murray have done us a service to draw our attention to the need to revisit the PPP recommendations. [Editor’s note: The Primary Open-Angle Glaucoma PPP was revised in November 2015 and is due for revision in 2020.]
Dr. Schuman: I definitely hear what you’re saying, but I do want to just press on this point a little bit. I think that Murray is referring to the study’s conclusion that says, “Health policy makers should be cautious about approving laser privileges for optometrists practicing in other states until the reasons for these differences are better understood.”
Dr. Heuer: I personally think that the study comes to a reasonable conclusion, particularly given that more than 90% of patients in many states, even somewhat rural states, are within an hour of an ophthalmologist. So it is a stretch to advocate on behalf of laser privileges for optometrists on the basis of access, especially if it is unclear that optometrists are providing cost-effective care. Consequently, I would say that some of the burden is on Murray and his colleagues to show that these data do not suggest that the policy makers ought to think twice.
Dr. Cantor: I also believe that the conclusions drawn are reasonable based on the data. We could probably cite multiple other instances where health policy is instituted on much less information than what’s presented in this article—often just on testimony and hearsay, and who talks the loudest. This is a Medicare database objective assessment of utilization, and it points out a difference in providers.
If all the indications were the same, and if ophthalmologists and optometrists were treating the same populations and using similar laser settings, modalities, and treatment parameters, then—apart from individual practitioner variability—there shouldn’t be much of a difference in practice patterns. The fact that there is a difference raises a question. The authors aren’t saying that laser privileges for optometrists in other states shouldn’t be considered. Instead, they are urging caution, given the data that they’ve been able to generate, and saying that these data should help inform any decisions going forward.
Dr. Schuman: And perhaps the number of subjects in the study also speak to the veracity of the findings.
What Patients Should Know
Dr. Schuman: Is there a message for the public from this study?
Dr. Heuer: Regrettably, the public does not understand the distinctions among ophthalmologists, optometrists, and opticians—the educational and training backgrounds of eye care professionals remain a mystery to the public, such that most cannot tell us apart. But like any surgery—and, after all, LTP is a surgical procedure—patients for whom it is being recommended need to do their due diligence, including asking their doctor: How many of these have they done? Why are they doing it the way they’re doing it? How many treatments will I need? And to the extent that this degree of granularity gets out into the lay press, even asking: Are you going to do a 360° treatment or not?
Dr. Cantor: To the public, I would also say that part of the mission that we all share is to ensure that the most effective treatments are being used in the most cost-effective manner. In order to do that, we need to ask questions like this study by Stein and colleagues did and seek answers, which might result in modifications to practice and policy, to provide the best health care to the public.
Landmark Study
The JAMA Ophthalmology study by Joshua D. Stein, MD, et al., titled “Comparison of Outcomes of Laser Trabeculoplasty Performed by Optometrists vs Ophthalmologists in Oklahoma,” looked at Medicare claims of 891 glaucoma patients (1,384 eyes) who had LTP in Oklahoma between Jan. 1, 2008, and Dec. 31, 2013.1 The authors evaluated LTP retreatments in the initial eye by type of surgeon. They found that, overall, more than double the percentage of eyes were retreated when the surgeon was an optometrist (35.9%) versus an ophthalmologist (15.1%).
At all points during the study, proportions of retreatment were significantly higher if the initial surgeon was an optometrist. For example, at 6 months, optometrists had retreated 24.9% of eyes, whereas ophthalmologists had retreated 3.9% of eyes. At 3 years, the percentages were 34.3% and 17.7%, respectively (p < .001).
The authors found that among patients treated by optometrists, the probability of retreatment during the 10-day global period for LTP was 0.4%; just after the global period (11-30 days after the first procedure) the probability of retreatment was 10.3%. Ophthalmologists’ patients underwent no additional procedures during the global period; the probability of retreatment was 1.1% from 11 to 30 days after the first procedure.
OD editorial. In response to the study, Murray Fingeret, OD, noted that the 27 optometrists included in the study were trained at a college of optometry that teaches students to start by treating only 180° of the trabecular meshwork. If pressure reduction is not sufficient, they should consider treating the remainder of the angle.
He also said that claims data merely report on utilization rates for the procedure without consideration for clinical details, which might shed light on quality, safety, or efficacy of the procedure. He concluded that the study “does not represent Level I evidence suitable for informing decisions about health care delivery or policy.”
MD editorial. Alan L. Robin, MD, noted in his editorial that the clinically significant difference in frequency of additional surgeries is concerning because repeat treatment has “decreased rates of success and an increased complication profile” and incurs both direct and indirect costs.
Of claims data, he said, in fact, that they “should be used when establishing and guiding policy decisions including who should perform ophthalmic procedures.” He notes that the strength of such data lies in their large numbers of subjects, objectivity, and insight into utilization and costs. He concluded by saying, “We hope that all [policy makers] would desire the safest, best quality, and most cost-effective care for their constituents. Therefore, until these differences are more thoroughly studied and understood and the additional costs and safety concerns are considered, granting optometrists permission to perform LTP should await the outcomes of these further studies.”
___________________________
1 Stein JD et al. JAMA Ophthalmol. Published online July 28, 2016. doi:10.1001/jamaophthalmol.2016.2495.
|
Meet the Experts
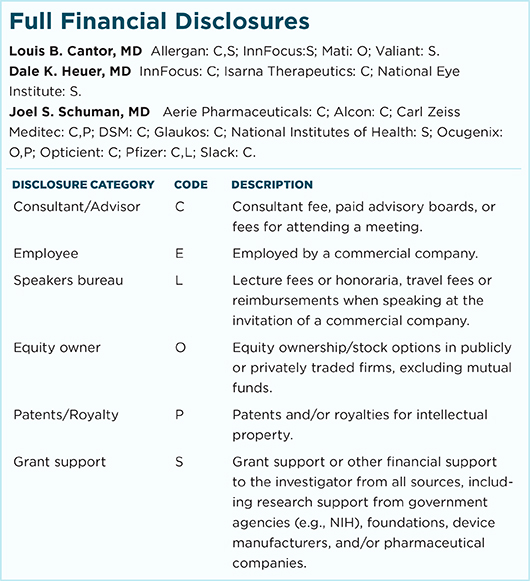
LOUIS B. CANTOR, MD, is chairman and professor of ophthalmology, Jay C. and Lucile L. Kahn Professor of Glaucoma Research and Education, and director of the glaucoma service at the Eugene and Marilyn Glick Eye Institute, Indiana University, Indianapolis. Financial disclosures: Allergan: C,S; InnFocus: S; Mati: O; Valiant: S.
DALE K. HEUER, MD, is Professor and Chair of Ophthalmology and Director of The Froedtert & the Medical College of Wisconsin Eye Institute, Milwaukee. Financial disclosures: InnFocus: C; Isarna Therapeutics: C; National Eye Institute: S.
JOEL S. SCHUMAN, MD, is professor and chairman of ophthalmology and professor of neuroscience and physiology at NYU Langone Medical Center in Manhattan. He is also professor of electrical and computer engineering at NYU Tandon School of Engineering. Financial disclosures: Aerie Pharmaceuticals: C; Alcon: C; Carl Zeiss Meditec: C,P; DSM: C; Glaukos: C; National Institutes of Health: S; Ocugenix: O,P; Opticient: C; Pfizer: C,L; Slack: C.
For full disclosures and the disclosure key, see below.
|