Download PDF
Interoperability is still very much a work in progress. But ophthalmology is developing ways to comprehensively store, analyze, and exchange data—with the potential to transform practices nationwide.
It’s an ambitious goal: By enabling health information systems to work together—both within and across organizations—interoperability can advance effective delivery of health care for individuals and communities.
Widespread use of EHRs. According to Academy membership surveys, the proportion of its U.S. members using electronic health records (EHRs) increased from 29% in 2009 to up to 75% in 2015. For many practices, the decision to invest in an EHR system was motivated partly by the financial incentives and, increasingly, by penalties from the Centers for Medicare & Medicaid Services (CMS) meaningful use (MU) program. This program provided a road map for EHR adoption, but it didn’t include directions for communications capabilities. Without that mandate, health information technology (HIT) interoperability has lagged behind EHR adoption.
The challenge of multiple nomenclatures. “In medicine, a vast number of nomenclatures has made it difficult to reliably exchange information,” said Jeffery Daigrepont, health care consultant and senior vice president at the Coker Group. “You can go anywhere in the world and use an ATM because of clear standards within the financial industry. But in medicine, there are many ways to describe a bellyache.”
That’s why it’s so essential to achieve semantic interoperability, which allows systems or elements to exchange and use information.1 This is the highest level of interoperability. The 2 lower levels are foundational interoperability, which simply allows exchange of data from one system to another, and structural interoperability, which defines the syntax of the data exchange and allows its interpretation.1
Future payment models will promote interoperability. With the shift to reimbursement models based on quality of care, the drive toward interoperability has intensified. Within the next 3 to 4 years, said Mr. Daigrepont, Medicare projects that 50% to 60% of reimbursement will be based on shared savings or value-based reimbursement tied to outcomes. While the details of these new payment models have not yet been finalized, the emphasis on measuring quality and costs is likely to be accompanied by a renewed focus on the infrastructure required to support improved exchange of data.
|
Competing nomenclatures. “You can go anywhere in the world and use an ATM because of clear standards within the financial industry. But in medicine, there are many ways to describe a bellyache.”
—Mr. Daigrepont
|
Trouble Acquiring & Exchanging Data
For practices that want to move toward increased interoperability, some of their current frustrations stem from the EHR system itself, particularly in the United States. In a recent Academy survey, for example, international respondents were quite favorable in their assessments of EHRs, but only 16% of U.S. ophthalmologists said their EHR increased productivity.2
Here are a few of the challenges.
Generic EHRs. Many ophthalmologists working at large institutions have an EHR system that is designed to collect information about general medicine, which means that “it doesn’t meet the needs of eye care or other specialties,” said Linda Wedemeyer, MD, RN, MS, a consultant on the Academy’s Committee on Medical Information Technology (MIT).
Data entry problems. Manual input of data has led to inconsistent identification of patients, said Mr. Daigrepont, both within practices and between them. “Doctors are terrified about using corrupt data or making decisions from data applied to the wrong patient.”
To compound matters, a device might be in one room and the EHR interface in another, she said, which requires getting the data from the device and then walking down the hall to input the results in the electronic record.
Diversity of devices. The number and diversity of ophthalmology’s in-office tests are also greater than in most other specialties, said Michael V. Boland, MD, PhD, cochair of the Academy’s Committee on MIT. “Diagnostic devices for retina, optic nerve, and cornea, for example, all produce different kinds of data,” he said, “which is difficult to put together in a coherent way and integrate with the EHR.”
Proprietary interfaces. Some offices have connected their devices to the EHR but have not done so in a standardized fashion, said Dr. Wedemeyer. “One of the biggest challenges of integrating these diagnostic devices with EHR systems relates to problems with proprietary interfaces. This forces physicians to buy devices based on what their EHR can connect to, rather than what they think is best for their patients. If you decide to swap devices a month after setting up your electronic office, you have to have the vendor and EHR coordinate on developing a proprietary interface. Chances of getting them to do this are slim, or they may charge you a significant fee for this custom work.”
Disparate entities. In addition, said Mr. Daigrepont, an ophthalmology practice can be 3 entities in 1—the medical practice, optical shop, and surgery center—which complicates the goal of interoperability.
Meaningful use? The CMS EHR incentive program includes 3 stages of MU, with each progressive stage necessitating a more advanced use of EHRs. Modifications are needed, however, to help ophthalmologists meet requirements, said Dr. Wedemeyer. “For one, meaningful use requirements are often not targeted to specialties like ophthalmology.” There is also some concern, she said, that the requirements are too complex and prescriptive and are creating new problems due to usability issues with the EHR. Furthermore, there is not enough focus on data exchange. “It’s appropriate to think about how to use this model to better drive real interoperability,” said Dr. Boland. “As the biggest player—and payer—in the room, the federal government can really help facilitate interoperability.”
|
Seamless workflow. “When you set up your office using our IHE workflows, you get the right data connected to the right patient.”
—Dr. Wedemeyer
|
Standardization: Paving the Way to Interoperability
Patient safety, efficiency, functionality—interoperability promises this and more. But these promises cannot be realized without first laying the groundwork through standardization, a major effort of the Academy for many years.
IHE Eye Care determines which standards are needed. Under the sponsorship of the Academy (and, later, the American Society of Cataract and Refractive Surgery), Integrating the Health Care Enterprise (IHE) Eye Care has developed specific protocols for ophthalmology, deciding which standards can best solve interoperability challenges in eye clinic workflows. “When you set up your office using our IHE workflows,” said Dr. Wedemeyer, “you get the right data connected to the right patient. The only way to get it wrong is if the wrong patient is selected from a work list on the device—but this is an infrequent occurrence.”
DICOM provides standards for medical images. Much of the progress toward interoperability has been made with Digital Imaging and Communications in Medicine (DICOM), a standard for collecting, storing, printing, and transmitting information in medical imaging. The Academy sponsored the DICOM standards for eye care devices. “One aspect of DICOM systems is a standard for generating work lists,” said Dr. Boland. “Rather than manually inputting demographics, the technician simply selects the patient’s name from the master work list.” So when an image is acquired, the patient demographics are added before it is pushed to the image archive.
The DICOM standard doesn’t only greatly reduce the risk to patients due to mismatches, said Jeffrey L. Marx, MD, chair of ophthalmology at the Lahey Hospital and Medical Center in Burlington, Mass. It also allows various machines to speak to one another and dramatically reduces time wasted due to patient-name confusion. “We’ve calculated that the amount of work involved in sending images through capture stations was at least double that required for DICOM-compatible systems,” he said.
Today, very few vendors—whether manufacturers of OCT, visual field perimeters, or cameras—lack the ability to provide some level of DICOM standardization, said Dr. Marx. However, David Pfennighaus, imaging informatics systems administrator at the Lahey Hospital and Medical Center, emphasized that DICOM compliance isn’t going to stifle innovation. “In other words, DICOM is not a protocol to eliminate ‘best in class,’” he said. “There’s still a lot of room for vendors to do what they do best.”
HL7 provides standards for data management. With 40 or 50 variations, said Mr. Daigrepont, Health Level Seven International (HL7) is the language used to manage textual data transfer between information systems. “As part of HL7, IHE Eye Care has developed clinical document architecture (CDA) documents to specifically address the needs of eye care professionals along with [the needs of] general medicine,” said Dr. Wedemeyer. “Vendors must generate these CDA documents in order for ophthalmologists to meet their MU requirements, and including eye care data makes the documents helpful for eye care practices rather than just for fulfilling regulatory requirements.”
SNOMED CT provides standards for the EHR’s clinical content. SNOMED CT is one of the more robust nomenclatures for the EHR’s clinical content—for diseases, clinical findings, therapies, procedures, and outcomes, said Dr. Boland. “Both HL7 and SNOMED CT help with communication outside your organization. For example, through the Academy, ophthalmology is defining which standardized data is needed to communicate a standard eye exam between systems.”
|
Buyer be wise. “Do your best to structure your payments based on deliverables and successful outcomes. … Don’t just write a big check and keep your fingers crossed.”
—Mr. Daigrepont
|
Before You Set Up an Integrated EHR
Setting up an interoperable practice is a huge undertaking, said Dr. Wedemeyer. You need to have everyone weigh in, and you need to do your research. “From EHR system reviews to guidance on writing an RFP, there’s a wealth of information available on the Academy’s website.” (See “Resources.”)
Know your ecosystem. “Make sure you clearly understand all the components in your ecosystem,” said Mr. Daigrepont. “Each ‘spoke’ of the ‘wheel’ may have a different language or database, but they’re all trying to come into the same hub. Remember, however, that it may not be cost-effective to integrate all your equipment, especially devices you are unlikely to use much in the future or ones nearing the end of life.”
Clarify work lists and workflow. The EHR generates the demographics for work lists, said Dr. Boland, so you want to make sure you have a clearly defined pathway for how it will get from the EHR to a device—or, more likely, from the EHR to the image management system, which will then talk to the devices.
“If you are placing orders for tests in your EHR, you want to make sure these will trigger the right workflow for the device,” he said. “We’re moving to a model where the provider orders a test before the person shows up on the work list, since we need to make sure that work list is clearly defined.”
In addition, orders, test results, and charges can all live in different places, said Dr. Boland, but this must be clearly defined. “For example, the interpretation of OCTs and visual fields in our clinic is done in the EHR,” he said. “I look on one screen at imaging and type my findings into another screen.”
Know system requirements. Vendors will typically lowball the requirements for their system, said Mr. Pfennighaus. “For our image management system, we were told we needed a server and 4 gigabytes of memory, as well as 1 Xeon dual processor with 2 terabytes of space. We’ve already upgraded to 20 gigabytes of memory on this machine, and now have 6 processors that have used about 4 terabytes of disk space.”
It’s also important, he said, to ask about costs for infrastructure and maintenance requirements as well as whether a system uses cloud-based software or a local client-server architecture.
Clarify DICOM conformance. When purchasing equipment, said Dr. Boland, first have your vendor provide a DICOM conformance statement. “It systematically describes which aspects of the system meet DICOM standards.” Does it do photography, but not visual fields or OCT? Does it only provide work list functionality, but no more? “You, or someone who represents your interests, need to get into the details to know whether or not it will do everything you want.”
Ask the right questions. In addition, Mr. Daigrepont said to be sure to ask questions like these:
- Can the database support multiple instances of the software; can it be partitioned?
- Can the database support multiple patient identification numbers?
- Does the database have the ability to send out messages to locate patient records in other systems?
- If you transition to a different vendor, how will the vendor make your data available to you?
- Is there a third-party relationship or is the relationship built into the product? “Dissolution of a partnership between a vendor and another party may mean you’ll need to start over in the future,” said Mr. Daigrepont.
Negotiate up front. It’s critical that your image management system be able to use different sources of data from different companies, said Dr. Marx. “Make sure this is included in the package.” If you need to integrate newer devices with DICOM, added Dr. Boland, ensure that you are able to purchase the DICOM licenses you need. Also, define what you are trying to accomplish in a statement of work and build testing into your contract, said Mr. Daigrepont.
“Do your best to structure your payments based on deliverables and successful outcomes, for example, 20% down at signing of the contract, 20% at installation, 20% after training and testing, 20% after going live, and the final 20% 30 days after go-live,” he said. “Having a structured payment term will create leverage for having a successful outcome, and it will spread out the payments. Don’t just write a big check and keep your fingers crossed.”
Find out what works for other practices. Don’t be afraid to pick up the phone and ask colleagues about the systems they’ve purchased, said Dr. Marx.
|
Image management. “A key part of your workflow is reviewing images and tests, so you’re likely to need very specialized software that allows you to analyze details in images.”
—Dr. Boland
|
Integrating Image Management
The first thing to do when putting together an electronic office is to establish an image management system, said Dr. Wedemeyer. Sometimes this is part of the EHR system, but often it is separate.
Archiving images. Most ophthalmology practices have multiple vendors supplying various pieces of equipment that are used on a daily basis, said Dr. Marx. “Images from all that equipment are usually archived via an image management system on a separate server.” But not all image management systems rise to the level of a picture archiving and communication system (PACS) with DICOM transfer and storage capability, said Dr. Boland.
Images in the EHR. Sometimes images will actually stay where they were generated, said Mr. Daigrepont, and there will be links back to the EHR. Or the image management system may be embedded within the EHR itself.
“That can work, but a lot of EHR vendors don’t do imaging well,” said Dr. Boland. “A key part of your workflow is reviewing images and tests, so you’re likely to need very specialized software that allows you to analyze details in images. The average EHR is not ophthalmology specific and imaging is not its main function, so it doesn’t build that kind of efficiency into its product.”
Workflow features. “You want to be able to order an image from your exam room,” said Dr. Marx, “and transmit it [the order] via DICOM to your photographers so they can easily—without entering patient demographics—perform the task and then notify the physician that the test was done.”
In addition, an interpretation is attached to the image, and the imaging procedure is dropped as a bill associated with a diagnosis so the physician can be paid. “It’s critical for all those steps to be readily available to a physician so they know when a test has been done and still needs to be interpreted.”
Lobbying for Interoperability
In addition to pouring resources into the development of standards and IHE EyeCare profiles, the Academy has lobbied Congress to move interoperability forward.
The problem of information blocking. In a report published last year, the Office of the National Coordinator (ONC) focused on those EHR vendors that have been impeding physician efforts to use and share EHR data. It noted that “current economic and market conditions create business incentives for some persons and entities to exercise control over electronic health information in ways that unreasonably limit its availability and use.” For instance, not all EHR vendors have cooperated with the Academy IRIS Registry, which is a robust clinical database that can help ophthalmologists look at outcomes and improve quality of care. “It also allows our physicians to participate in physician quality initiatives required for meaningful use payment [and PQRS, see “IRIS Registry Web Portal Launches the Diabetic Retinopathy Measures Group”],” said Dr. Wedemeyer. And while some EHR vendors have refused to work with the IRIS Registry, other vendors have charged doctors significant fees for integrating their EHR system with it.
MU can help provide a solution. The MU program should do more to deter information blocking and promote interoperability. Last year, under pressure from the Academy and other health care stakeholders, congressional leaders added provisions to the 21st Century Cures Act that would make interoperability a prerequisite for EHR certification under the MU program. The proposed legislation would also require EHR vendors to publish their application program interfaces and make it easier for EHR users to share data with clinical registries, like the IRIS Registry. The legislation was passed by the House of Representatives last year. At time of press, a separate health care IT legislation was under consideration in the Senate. If that passes, the House and Senate will have to reconcile the 2 bills before the interoperability provisions can become law.
For the latest news on Academy advocacy, go to www.aao.org/advocacy/eye-on-advocacy.
|
What’s Next for Interoperability?
What is the future of interoperability in ophthalmology?
“The move toward base-level DICOM compliance will continue,” said Dr. Boland, “but what we’ll really need is for vendors to implement the ability to capture every pixel of data—ophthalmology-specific DICOM objects for OCT, visual fields, photography, and corneal topography. Standards with this level of detail exist now.”
In the future, said Dr. Marx, image management systems will give us the ability to highlight differences between scans or other modalities and rigorously run that data through new algorithms to see whether patients are progressing. “We may even be able to combine information—the patient’s vision, IOP, and imaging results, for example—with the EHR to better care for our patients and help us deal with a deluge of data.”
Companies are starting to embed proprietary algorithms within their image management systems to analyze data generated by their equipment, said Dr. Marx. “Not only do the individual devices like OCT compare images from one visit to the next, but the system can also provide value-added analysis, which streamlines the process and helps us better manage these patients. For example, it might allow us to quickly pull up only right eyes, or only one type of scan.”
With future advances in interoperability, it would be great to be able to compare images from different equipment vendors as well, said Dr. Wedemeyer. “In the ideal scenario, data from each type [of device] would be comparable regardless of where—and in what system—it was created; that is an ideal end point for interoperability.”
Eventually, said Dr. Boland, ophthalmology will arrive where radiology was 10 years ago—able to send data from one practice to another without the “complicated gymnastics” of moving information onto a disk or riffling through piles of notes.
___________________________
1 Health Information and Management Systems Society (HIMSS). “What Is Interoperability?” Accessed Feb. 15, 2016.
2 Academy 2015 EHR survey. EyeNet. 2016;20(3):77.
Meet the Experts
MICHAEL V. BOLAND, MD, PHD Director of Information Technology, Wilmer Eye Institute; associate professor of ophthalmology, Johns Hopkins School of Medicine, Baltimore; cochair of the Academy’s Committee on Medical Information Technology. Relevant financial disclosures: None.
JEFFERY DAIGREPONT Health care consultant and senior vice president at the Coker Group, a nationwide consultancy group based in Atlanta. Relevant financial disclosures: Coker Group: E.
DAVID PFENNIGHAUS Imaging informatics systems administrator at the Lahey Hospital and Medical Center in Burlington, Mass. Relevant financial disclosures: None.
JEFFREY L. MARX, MD Chair of ophthalmology, Lahey Hospital and Medical Center; chief medical officer, Lahey Peabody Medical Center in Burlington, Mass. Relevant financial disclosures: None.
LINDA WEDEMEYER, MD, RN, MS Physician informatician, clinical quality, Health Solutions Management Office, Office of Informatics & Analytics, Veterans Health Administration, Los Angeles; consultant on the Academy Committee on Medical Information Technology; cochair, IHE Eye Care Planning Committee. Relevant financial disclosures: None.
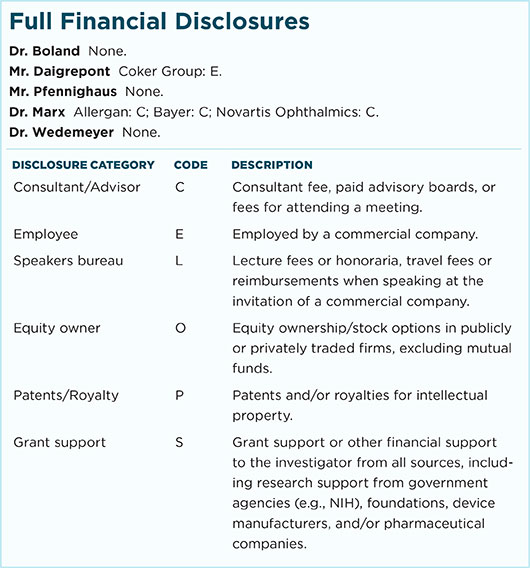
For full disclosures and the disclosure key, see below.
|