Download PDF
In a first-ever collaboration, 4 supranational cornea societies joined forces in a complex, multistep process to develop the Global Consensus on Keratoconus and Ectatic Diseases.1 A total of 45 keratoconus (KC) specialists—9 section coordinators and 36 expert panelists nominated by the societies—focused on 3 topics: Definition/ Diagnosis, Nonsurgical Management, and Surgical Management. Here, 3 of the section coordinators talk about the consensus process, key findings, and next steps for clinicians and researchers involved with ectatic disorders.
Impetus for Seeking Consensus
Although keratoconus has been recognized for more than 150 years, technological developments over the past 20 years have wrought substantial changes in its diagnosis and management.1 And along with the wider range of options have come controversies and questions, most notably: How do you define the disease and progression? What is the best time for intervention, and with what modalities?
According to Donald T.H. Tan, MD, at the Singapore National Eye Center, the global consensus project originated with José Gomes, MD, PhD, at that time president of PanCornea, who approached the leaderships of the Asia Cornea Society, the Cornea Society, and EuCornea. “All societies felt that advances in the knowledge of keratoconus had become complex and that an overview of the current knowledge of the etiology, diagnosis, and treatment was needed,” Dr. Tan said.
With funding from the Asia Cornea Foundation, in addition to the 4 societies, the panels embarked on multiple Delphi-style rounds of scenarios and questions, combined with a face-to-face meeting at AAO 2014. From this emerged a number of “agreements”—that is, statements that had the support of at least two-thirds of the panelists.
 |
|
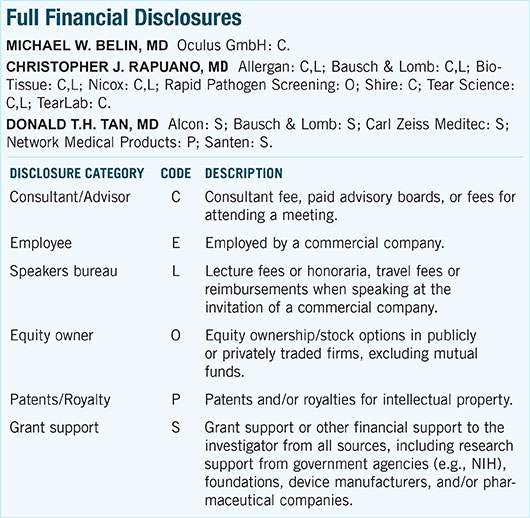
IMAGING KERATOCONUS. Scheimpflug mapping allows analysis of both the anterior and posterior aspects of the cornea. (1A) Anterior instantaneous curvature; (1B) Corneal pachymetry; (1C) Anterior elevation, best-fit spheres (BFS); (1D) Posterior elevation, BFS.
|
Definition and Diagnosis
“Keratoconus is easy to diagnose when it’s moderate to severe. You can see it easily at the slit lamp—you don’t even need a topographer,” according to Christopher J. Rapuano, MD, at Wills Eye Hospital. That diagnostic approach might have been adequate when treatment options for KC were limited, but the advent of corneal cross-linking (CXL) has been a “game-changer,” according to Michael W. Belin, MD, at the University of Arizona.
“When you do full-thickness keratoplasty, you intervene only at a fairly advanced stage, when it is obvious that someone has the disease,” Dr. Belin said. “Now that we have the ability to either slow or maybe even stop progression [with CXL], the goal changes from trying to improve already decreased vision to preventing a decrease in vision—and that requires identifying disease at a much, much earlier stage.”
Importance of the posterior cornea. Accordingly, as part of the definition process, the panel specifically considered the criteria for diagnosing mild or subclinical KC. They reached a consensus that posterior corneal elevation must be present in order to diagnose these stages. Dr. Rapuano noted that “keratoconus really shows up first in the posterior corneal curvature,” thus making early diagnosis possible.
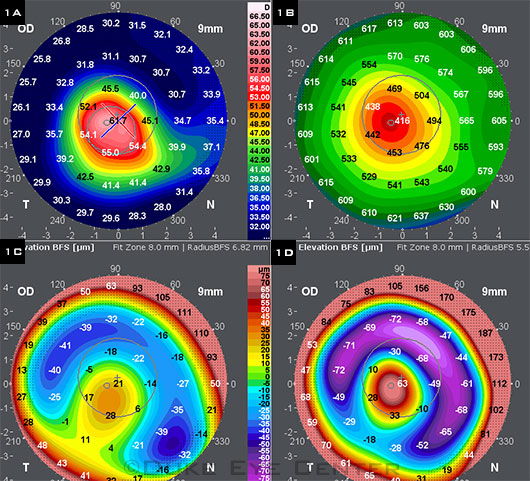
This new criterion follows on recent developments in imaging, such as optical coherence tomography and Scheimpflug photography (Figs. 1, 2). As Dr. Tan said, “Abnormal posterior elevation is now beginning to be recognized as one of the major factors in the diagnosis of keratoconus, simply because of newer instrumentation which can now identify posterior elevation. Previously, we mostly relied on instruments [e.g., corneal topographers] which could only detect steepening of the anterior corneal surface.”
In addition to posterior ectasia, other mandatory findings for diagnosing KC are abnormal corneal thickness distribution and clinical noninflammatory thinning. The experts did not specify numeric values for these parameters, noting that those will vary depending on the measurement device.
Progression. Identifying progression is paramount in treatment and timing decisions. The consensus definition requires the consistent presence of 2 of the following 3 parameters: “1) steepening of the anterior corneal surface, 2) steepening of the posterior corneal surface, and 3) thinning and/or an increase in the rate of corneal thickness change from the periphery to the thinnest point.”1 No decrease in BCVA is required, although it is likely to coexist with the progression-defining attributes.
Other diagnostic points. In all, 18 agreements were reached in the definition/diagnosis section. These included distinguishing true ectatic disorders—keratoconus, pellucid marginal degeneration, keratoglobus, and postrefractive surgery ectasia—from thinning disorders, such as Terrien marginal degeneration. Other areas of consensus were use of imaging and diagnostic devices, pathophysiology of KC, and risk factors for KC.1
Clinical implications of definitions. Although the meticulous parsing of terms and conditions might seem to be hairsplitting, the resultant definitions will have a strong impact on both treatment and research. As Dr. Belin said, “There’s a good argument that we should be intervening at a much, much earlier stage to preserve vision rather than waiting until visual loss occurs. Thus, it’s crucial to establish what constitutes true disease.”
Dr. Tan noted, “The main clinical impact of this has to do with the decision-making process in various treatment approaches ... such as collagen cross-linking, where the main aim is to prevent further progression.”
Benefits for research. In addition, Dr. Tan emphasized the importance of consensus definitions for ongoing and future KC research: “For example, if the inclusion criteria for a cross-linking trial are too broad and include cases which may not actually be considered as progressive disease, there may be erroneously positive results in the trial concluding that cross-linking was successful, simply by including cases which would not have progressed in the first place.”
Nonsurgical Management
The consensus group developed a flowchart of treatment strategies, beginning with the least invasive, to meet the most important goals in KC management: halting disease progression and achieving visual rehabilitation.
Surprisingly simple recommendations. Of the 2 most strongly supported agreements in the area of nonsurgical management, the first is simple, low tech, and low cost: The physician should counsel patients about the importance of not rubbing their eyes. Dr. Rapuano said, “I feel strongly, as do many cornea specialists around the world, that eye rubbing is an important component of either causing keratoconus or making it worse.” He believes that this message is not fully appreciated in the general ophthalmology community and should be more widely communicated.
The other strongly supported agreement concerns patients with ocular allergy: Topical antiallergic medications and lubricants should be prescribed to decrease ocular irritation—and, thus, the urge to rub the eyes.
Is dry eye a factor? The panelists did not reach agreement on the role, if any, of dry eye in KC. Ultimately, they stated, “There is no direct relationship between keratoconus and dry eye.”1 Nevertheless, they added that for patients in whom both conditions are present, preservative-free eyedrops are preferable, as preserved drops may be associated with irritation, microtrauma, and, consequently, eye rubbing.
Optical correction. The panelists confirmed the importance of contact lenses for visual rehabilitation of KC and other corneal ectasias, although they acknowledged that these devices do not slow progression of the disease. Further, they suggested a stepwise approach to optical correction, starting with spectacles or conventional soft lenses if possible and proceeding to gas-permeable lenses as needed. If correction or comfort is unsatisfactory, other lens options include specialized KC models, hybrid, piggyback, and scleral lenses.1
Clinical aspects of specialized lenses. There may be some practical limitations in following these steps, said Dr. Belin. He noted that although there have been improvements in the design and materials of specialized lenses, fitting these lenses is becoming a “lost art” in the majority of U.S. clinics. “Many of us are seeing fewer individuals who either are trained to properly fit keratoconus patients or are willing to undertake it because it is a substantial time commitment, and the reimbursement is relatively low for that effort.” He added, “A lot of third-party companies will deny payment for specialized contact lenses but will pay for a transplant, which, if you think about it, is counterproductive.”
 |
|
KC IN PROFILE. Dual Scheimpflug imaging of a keratoconic cornea.
|
Surgical Management
Taking the next step. How does the ophthalmologist determine when it is time to move on to surgical intervention? The panelists agreed that the decision is based on the patient’s ability to achieve satisfactory vision with optical correction. As Dr. Rapuano explained, “One important point was than even though a patient can see 20/30 in your office with a contact lens, it’s not necessarily satisfactory BCVA. If the patient can’t tolerate the lens for more than an hour, surgery may be indicated.”
According to the panelists, the most important surgical techniques for improving best uncorrected VA are, in order, descemetic deep anterior lamellar keratoplasty (dDALK), penetrating keratoplasty (PK), and intracorneal ring segment (ICRS) implantation. In contrast, CXL is intended to stabilize the cornea rather than improve VA.
Corneal cross-linking. For most clinicians outside the United States, CXL is the first surgical intervention. In fact, more than 83% of the panelists perform it; and the consensus treatment algorithm shows it as one of the earliest management steps to consider, especially in young patients. The panelists agreed that there should be no upper or lower age limit for CLX in KC eyes that show evidence of progression.
Although in one of the U.S. FDA trials, the minimum age is 12 years, said Dr. Rapuano, “In listening to discussions of specialists from around the world, they’re doing it in 8-year-olds or 10-year-olds with keratoconus, even if there is no evidence of progression. Their thought process is that it is extremely likely to progress in such young people, and they don’t want to wait until it’s gotten worse.”
Corneal transplantation. Apart from CXL, the most common surgical procedures are DALK and PK. In choosing between the two, the panelists listed the most important indicators for PK as significant corneal scarring, very thin cornea (<200 μm), risk of acute hydrops, and failure of other surgical methods.
If none of these conditions are applicable, panelists would perform some form of DALK in more than 60% of cases, and the type most commonly attempted is dDALK with big bubble technique (51% of cases).1
Clinical aspects of DALK vs. PK. However, Dr. Tan noted that these figures do not necessarily reflect clinical practice at large.
“Although this panel of experts clearly preferred DALK surgery as the new ‘gold standard,’ it should be noted that the commonest transplant procedure today is still probably PK, due to the fact that it has been the main standard transplant procedure for decades, and in general still has very good results, while the learning curve of DALK remains challenging. Eye Bank Association of America data suggest that ALK surgery constitutes less than 2% of all corneal transplants in the U.S.” He added that ALK accounts for about 25% of transplants in countries such as Brazil, Italy, and Singapore.
Dr. Tan attributed the difference in surgical preferences to the fact the consensus panelists “are corneal experts who have contributed to the scientific literature of keratoconus, including corneal surgeons who have studied various forms of keratoplasty.”
They recognize that “DALK, although more surgically challenging, offers major clinical advantages over PK in terms of less allograft rejection, better preservation of healthy endothelium, and longer-term graft survival, simply because the healthy endothelium in keratoconus is not exchanged in DALK surgery,” Dr. Tan said.
Other surgical interventions. ICRS are employed less commonly than the procedures discussed above. The use of other techniques—including photorefractive, superficial, and arcuate keratectomy; conductive keratoplasty; and clear lens extraction with IOL implantation—is very infrequent among the expert panelists.
More at the Meeting
Expand your knowledge of keratoconus and cross-linking—15 presentations on these topics will take place at AAO 2015 and Cornea Subspecialty Day, including instruction courses, a Learning Lounge program, and a hands-on Skills Transfer lab on CXL. Check the online program to pinpoint the right courses for you.
|
Looking Forward
Now that consensus has been reached by the expert panels on numerous key points in definition and management, what are the next steps in advancing KC care?
Dr. Tan suggested that careful study of the consensus document will benefit both clinicians and researchers. Clinicians can gain an expert perspective on state-of-the art diagnosis and management, and researchers can use it to devise better and more comparable translational, clinical, and epidemiological studies of corneal ectatic disease.
Dr. Belin believes that some of the next steps will involve research on and further developments in CXL techniques. Some of the areas of study include epi-on versus epi-off procedures as well as different lengths of UV exposure and amounts of energy delivered. Even more important, however, will be “getting a better handle on when to intervene with CXL,” he said.
“If we are able to identify with a fair amount of specificity those patients with true disease that is going to progress—and we are able to prevent that progression—that would be a major benefit.”
___________________________
1 Gomes JA et al. Cornea. 2015;34(4):359-369.
___________________________
Michael W. Belin, MD, is professor of ophthalmology and vision science at the University of Arizona, in Tucson. Relevant financial disclosures: Oculus GmbH: C.
Christopher J. Rapuano, MD, is chief of the cornea service at Wills Eye Hospital and professor of ophthalmology at the Sidney Kimmel Medical College at Thomas Jefferson University, in Philadelphia. Relevant financial disclosures: None.
Donald T.H. Tan, MD, is medical director of the Singapore National Eye Centre, chairman of the Singapore Eye Research Institute, and professor of ophthalmology at the National University of Singapore. Relevant financial disclosures: Alcon: S; Bausch & Lomb: S; Santen: S.
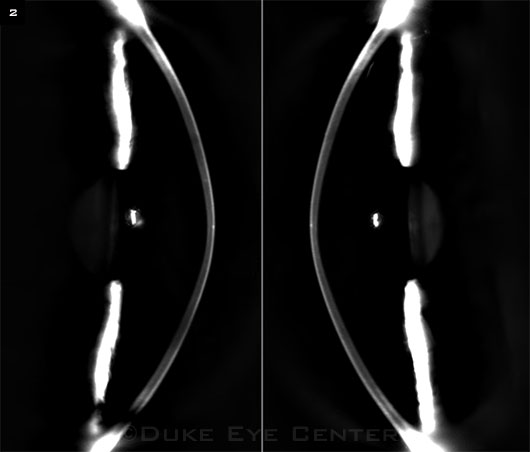
For full disclosures and the disclosure key, see below.