By Sanjay G. Asrani, MD, with Paul J. Foster, FRCS, Paul F. Palmberg, MD, PhD, and Robert Ritch, MD, FACS
Download PDF
This article is part of an occasional series of MD Roundtables, in which a group of experts discuss a topic of interest in their field. Here, Sanjay G. Asrani, MD, of the Duke Eye Center, leads a roundtable on plateau iris. He is joined by Paul J. Foster, FRCS, of University College London, Paul F. Palmberg, MD, PhD, of Bascom Palmer Eye Institute, and Robert Ritch, MD, FACS, of the New York Eye and Ear Infirmary. Following are edited excerpts from their conversation.
Identifying Plateau Iris
Telltale sign: ciliary body displacement. Dr. Palmberg: We were interested in plateau iris years ago, and I came up with a theory that the ciliary body rolled forward, which, I later learned, Paul Chandler had observed in 1965 when he looked through a surgical iridectomy and saw the forward-lying ciliary process.
In 1982, Doug Anderson and I treated a patient; I was doing indentation gonioscopy, and Doug was watching me. As we pushed, he said, “Oh, I think [your theory is] right because the peripheral iris, that little bicycle tire out in the periphery of elevated iris, is breaking up into individual parts that look like iris draped over ciliary processes,” but we couldn’t do ultrasound to confirm our finding. Fortunately, Bob Ritch and folks in Toronto then got ultrasound biomicroscopy (UBM) and definitively defined the mechanism.
Dr. Ritch: If you look at UBMs, the ciliary body in plateau iris is actually about 3 times the normal size. So, I think it’s a hereditary, enlarged, anteriorly positioned ciliary process rather than the kind of anterior rotation you’d get with malignant glaucoma or a supraciliary effusion. And 30 years ago, maybe more, you [Dr. Palmberg] sent me a slide of a ciliary process that was sitting on the lens in a patient with plateau iris. And now I think that’s a classic indicator. If you do an iridotomy peripherally and see those big ciliary processes on the anterior surface of the lens, you’re looking at plateau iris.
Clinical characteristics. Dr. Palmberg: If patients who are 30 to 50 years old come in with appositional angle closure but are not hyperopic—about 50% of them will turn out to have plateau iris. A very high index of suspicion is required for appositional angle closure if a 30-year-old walks in with no lens swelling, has no forward bombé of the iris, and the iris is perfectly flat.
A young woman who had had a 500-μm laser iridotomy kept coming to the emergency room at Bascom Palmer with angle-closure attacks and intraocular pressure (IOP) of 30, 40, and 50 mm Hg. They brought her to me, and she had plateau iris. We did iridoplasty, and those things stopped happening to her. So, I think this needs to be emphasized about patients with plateau iris: They have to have appositional closure, and they have to have the configuration with closure. These people respond extremely well to laser iridoplasty. But most people with elevated IOP after laser iridotomy probably have synechial closure, and they wouldn’t benefit from iridoplasty.
Dr. Ritch: That’s one of my rules: Anybody under the age of 50 with angle closure has plateau iris until proven otherwise, and 80% are women. It’s hereditary, so check their siblings also.
 |
|
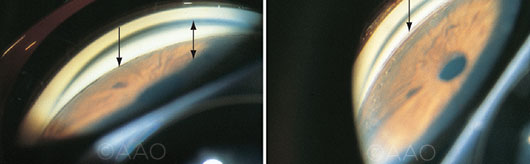
PLATEAU IRIS SYNDROME. Left: A flat iris plane but shallow angle recess (arrow). Note that the midperipheral angle appears deeper (double arrow) than the narrow angles associated with pupillary block. Right: A much deeper angle recess (arrow) following laser peripheral iridoplasty.
|
Limited Utility of Pilocarpine
Dr. Asrani: Bob, what about the role of pilocarpine versus iridoplasty for plateau iris?
Indications for pilocarpine. Dr. Ritch: The only plateau iris patients I’ve had to maintain on pilocarpine were people who still had a very sharp angle, a very sharp plateau, even after iridoplasty. They still have very far peripheral iris up against the meshwork—out past the iridoplasty burns even when we do them very peripherally. (I have done this all over Asia, and I found that Filipinos have the thickest irides.) I maintained them on 2% pilocarpine at bedtime just to keep them from closing up with peripheral anterior synechiae (PAS).
For most patients, I’ve been able to use much smaller spots, 100 to 200 μm, and low-power, long-duration burns in the very periphery to open those portions of the angle. So, I have very few patients on pilocarpine after iridotomy, and I think that you can get rid of the need for it with iridoplasty in virtually all patients.
Contraindications for pilocarpine. Dr. Ritch: Way back, patients were treated with pilocarpine when they had chronic angle closure and didn’t want surgery. And pilocarpine is OK and will open the angle in a patient who has pupillary block or plateau iris.
However, if you give pilocarpine chronically to people who have lens-related glaucoma, you’re going to bring the lens forward, and you’re going to close the angle over time. So pilocarpine is contraindicated in those patients. If the angle is still appositionally closed after iridotomy, then indentation gonioscopy will tell you whether it’s plateau iris or lens-related angle closure. In either case, iridoplasty opens the angle in virtually 100% of patients.
Dr. Asrani: Paul Foster, what do you think is the role of pilocarpine versus iridoplasty in patients who have appositionally closed angles after a patent iridotomy?
Dr. Foster: These days I’m loath to give people long-term pilocarpine treatment because I think we’re heading into an era when the definitive control of angle-closure disease is going to be through lens extraction. If patients have been on pilocarpine for a few years, their pupil is relatively immobile, and they’ll have posterior synechiae. For lens extraction surgery, you’ll have to use iris hooks or some other form of mechanical iris dilation, and those patients get less favorable results specifically because they’ve been on pilocarpine.
Managing Plateau Iris
Laser iridotomy. Dr. Palmberg: Some patients with an acute angle-closure attack not only have pupillary block but often may have some severe ischemia of the iris that will cause swelling of the ciliary body and a pseudo-plateau iris. So, you do the laser iridotomy. Say the IOP goes from 70 to 35 or 40 mm Hg but the angle is still closed. You say, “OK, we’re going to have to do a trabeculectomy in the morning.” Then you come back in the morning, and the IOP might be 8 mm Hg, and the angle is open, and you say, “Gee, what happened?” Well, what happened is that you got the IOP down low enough so that, with medical therapy and the laser iridotomy, the congestion resolved—you created better blood flow to the ciliary body, which caused the swelling to go down.
When iridotomy is insufficient. Dr. Palmberg: But if the IOP doesn’t go down and the angle is still closed, that’s when an iridoplasty really helps to get the angle open and bring down the IOP right away. It gets rid of the pain, and it probably prevents the formation of synechiae.
So, for patients with a narrow angle and a plateau configuration, I don’t think they need iridoplasty if their angle opens up, but they need to be monitored. They’re not necessarily going to have been cured by the iridotomy. Years later, you may see that the angle has closed; in such cases, iridoplasty is helpful.
We also found that some patients needed retreatment 5, 10, 13 years later—because the ciliary body had come forward again.
Considerations for iridoplasty. Dr. Ritch: I think that some iridoplasty procedures are not done far enough in the periphery. I’ve seen many patients who had iridoplasty burns in the midperiphery of the iris—that’s not going to open the angle. Peripheral iridoplasty means peripheral.
We reviewed the charts of 14 patients (23 eyes) who had been treated for plateau iris by iridotomy but experienced residual appositional closure after iridotomy, for which iridoplasty was performed. Six to 15 years after iridoplasty, the success rate was 100%; only 3 eyes needed retreatment.1
Dr. Palmberg: Doug Anderson and I looked at 1,700 laser iridotomies that were done in our institution, then followed up to determine how many of them underwent iridoplasty, and it was about 3%. Most of those were done soon after we did an iridotomy if the angle didn’t open up. Some cases were 2 to 9 years later, when the IOP was up again. There can be a progressive form of ciliary body rolling forward.
The value of iridoplasty. Dr. Ritch: Clement Tham in Hong Kong started doing immediate iridoplasty, and I do that, too. Now, when the patient comes in with angle closure, I don’t even bother treating them medically. We just do immediate iridoplasty, and an hour later the IOP is 16 mm Hg.
___________________________
1 Ritch R et al. Ophthalmology. 2004;111(1):104-108.
___________________________
Dr. Asrani is professor of ophthalmology at Duke Eye Center, Durham, N.C. Financial disclosures: Alcon: L; Dose Medical: C; Heidelberg: L; Lumenis: L.
Dr. Foster is professor at University College London Institute of Ophthalmology and at Moorfields Eye Hospital, London. Financial disclosures: Alcon: L,S; Allergan: L; Carl Zeiss Meditec: L.
Dr. Palmberg is professor of ophthalmology at Bascom Palmer Eye Institute, Miami. Financial disclosures: Abbott Medical Optics: S; Aeon Astron, Europe: C; AqueSys: C,L; Aurolab: C; InnFocus: C,L; Pfizer: C.
Dr. Ritch is the Shelley and Steven Einhorn Distinguished Chair, professor of ophthalmology, Chief of Glaucoma Services, and Surgeon Director Emeritus, New York Eye and Ear Infirmary, New York, N.Y. Financial disclosures: Aeon Astron: C; Diopsys: C; Glia: C; Guardion Health Services: C; iSonic: C; Mobius: C; Ocular Instruments: P; Sensimed: C.
See the disclosure key at www.aao.org/eyenet/disclosures.