Download PDF
This article is part of an occasional series of MD Roundtables, in which a group of experts discuss a topic of interest in their field. This month, Leah Levi, MD, of the Scripps Clinic, leads a roundtable on photophobia. She is joined by Kathleen B. Digre, MD, of the University of Utah, and Randy H. Kardon, MD, PhD, of the University of Iowa. Following are edited excerpts from their conversation.
Case Presentation
Dr. Levi: I saw a 58-year-old woman yesterday who had a history of migraine with visual aura for about 3 years when she was in her 20s. That was followed by a long migraine-free interval until her early 50s, when she began to get migraines 2 or 3 times a year. About 5 years ago, the frequency of her migraines started to increase markedly, and they have remained frequent since that time.
Challenging Symptoms. The patient became increasingly light sensitive to the point where she needed to wear dark glasses even in the house and would, when possible, stay in her room with the curtains drawn. She was put on amitriptyline, which allowed her to go outside, tolerate room lights, and continue her job as a teacher. She was also treated with Botox and topiramate, and they helped. However, she has remained intolerant of computer or other digital screens. These make her photophobic and also trigger her headaches. She has tried tinted glasses—and, in fact, had a brownish tint on her glasses when I saw her yesterday—and also tried a computer glare screen. However, these have not helped very much.
In addition, the patient has dry eyes, but artificial tears haven’t helped her light sensitivity even though they help the dry feeling.
Finally, the patient has convergence insufficiencies, and her migraines are also triggered by reading, but she’s unable to do the computer-based convergence insufficiency exercises at this point because she’s so light sensitive to the computer screen.
 |
|
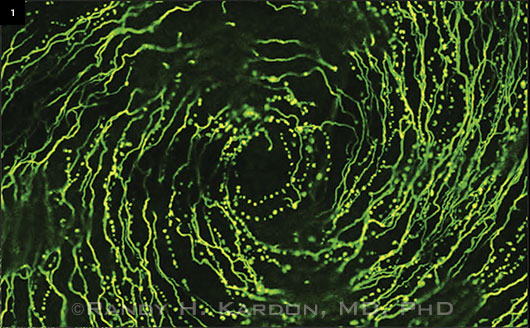
Research Target. The trigeminal nerve may be the link between dry eye symptoms and photophobia. This image demonstrates the density of the trigeminal nerves in a cornea labeled with antitubulin (a marker for nerves).
|
Defining Photophobia
Dr. Levi: Help us understand photophobia. What is it?
Dr. Digre: Photophobia is a misnomer, because photo means light and phobia means fear. But it really isn’t a fear of light; it’s an unusual sensitivity to light. In other words, the light gives people a feeling of discomfort or even pain. You need to differentiate it from things like dazzle or hemeralopia, because photophobia doesn’t cause people to have washout of their vision or blindness. It causes discomfort—and, in extreme cases like this one, it triggers migraines and pain.
Dr. Levi: Randy, can you talk about the connection between light sensitivity and pain?
Emerging Research. Dr. Kardon: This is an emerging area, both from a neuroscience standpoint and from putting this together with patients’ complaints. The pathways in the brain that are stimulated by light are still being elucidated. Some of the evidence shows that light-conducting nerves from the eye have input to the thalamus. The nerves modulate pain fibers that are coming to the thalamus from the meninges lining the brain. This pain signal is also conveyed to the sensory trigeminal nucleus in the lower brainstem. These “way stations” that translate light into pain are still not completely elucidated. It’s important to try to understand them, because knowing the pathways and knowing the neurotransmitters leads the way toward new therapeutic interventions.
CGRP and the Trigeminal Nerve. For example, a major neurotransmitter that modulates pain is calcitonin gene–related peptide (CGRP). Different pharmaceutical companies have been trying to develop new drugs that modulate the CGRP response for treatment of migraines, and these drugs may have an impact on the effect of light on pain. The trigeminal nerve, which has CGRP as its neurotransmitter, innervates the cornea, the orbital structures, and the lining of the brain. Once one part of the trigeminal nerve becomes activated and sensitized to an inciting stimulus, then other divisions may also become sensitized, resulting in different patterns of referred pain to the eye, orbit, or head.
That’s why in your patient, for example, dry eye that may be influencing the trigeminal nerve may in turn adversely increase the sensitivity to other stimuli such as light and even a particular wavelength of light (Fig. 1). Certain neurons that contain melanopsin in the structures of the eye may be more sensitive to blue wavelengths. This might explain why some patients achieve some relief of their light sensitivity by wearing eyeglasses that have an orange tint that blocks the blue component of light. Many of these patients complain of being more light averse under fluorescent lights that have a bluer component of light.
Individual Responses
Dr. Levi: What factors seem to influence the individual variations in light sensitivity?
Dr. Digre: All of us have a threshold for light sensitivity. If you go into a movie theater in the middle of the afternoon and you come out into bright sunlight, your first response is to close your eyes or squint. But it’s clear from studies that people with migraine and blepharospasm have lower light sensitivity thresholds than normal, and that’s probably part of the pathophysiology of these conditions.
Dr. Kardon: One aspect to consider is whether more light is getting to the retina or whether the patient’s reaction to the light is exaggerated. For example, some of the work we’ve published shows that in patients with blue irides lacking melanin pigment, a lot of light goes right through the eye to the retina in spite of the pupil’s size. So, even if these patients have their pupils constricted with a cholinergic agent to make them miotic, plenty of light still gets through to the back of the eye. The extreme of that, of course, would be albinotic patients who are extremely light sensitive no matter what size pupil they have. So, it is important to keep in mind that the pupil and the eyelids may not be efficient at limiting the light getting into the retina in lightly pigmented patients.
Dr. Levi: That’s an interesting point, because I’ve had patients who have just a general complaint that they’re getting more light sensitive as they age, and they don’t have any underlying pathology—and most of those patients, if not all of them, have blue irides.
Measuring Photophobia
Dr. Levi: One of the frustrating things about photophobia is that it seems to be such a subjective complaint. Is there any way of measuring this that either of you know about or are developing? If so, is it going to find its way eventually into the office?
Dr. Kardon: We have funding from the U.S. Department of Defense to try to develop an objective method of assessing light sensitivity. And by light sensitivity, I mean not only the amount of light reacted upon by the retina but also the trigeminal system and the brain’s response to the light.
Exaggerated Response. Of course, the amount of light getting to the input side of the equation can be monitored by the pupil reaction to light. But if you look at patients who have an adverse, painful response to light, their pupil responses aren’t abnormal compared with age-matched subjects who don’t have this reaction to light. So, most cases of light sensitivity cannot be explained by an increase in sensitivity of the retina to light. Rather, the signal from the retina is being acted upon in an exaggerated way by the recipient areas of the brain. Exceptions to this are patients who do have exaggerated sensitivity of the retina to light—for example, patients with achromatopsia.
How can one measure an exaggerated sensitivity of brain areas receiving the retinal light signal? One good candidate would be recording the degree of a photic blink reflex. The photic blink reflex has some similarities to the corneal blink reflex: If something touches the corneal nerves, it initiates an input to the trigeminal sensory nucleus in the brain stem that causes the facial nerve to fire, and the person blinks. Similarly, if a bright light is shined into the eye, the photic blink reflex causes the eye to blink, providing a protective mechanism. We’ve been trying to take advantage of this objective blink reflex by recording the electrical responses around the orbicularis and procerus muscles in response to light. We found that it’s a graduated, involuntary response—the more light stimulus you give, the greater the activation of those muscles.
Involuntary Muscle Contraction. Patients who are migraineurs and who complain of light sensitivity have an exaggerated electrical response and contraction of the muscles around their orbicularis and procerus and brow muscles compared with patients who are not. We’re also trying to monitor this response from a video recording; the amount of contraction of the eye muscles and the brow muscles can be quantified without an electrode using facial features extracted from videos. We’re trying to quantify this involuntary activation of the facial muscles in response to different doses of light to give an objective measure of light responsiveness that might indicate which patients are abnormally light sensitive—and, furthermore, which agents or mitigations might reverse the exaggerated response to light.
Dr. Digre: I would like to point out that as people age, their blink reflex becomes shorter. Babies, for example, can stare at lights for long periods of time without blinking, but older people, even normal older people, will blink more readily.
Examination Aids. Dr. Digre: I’d also like to say that there are questionnaires for photophobia. Not everybody has a machine to test for light sensitivity, but validated questionnaires are available in the literature.
Dr. Kardon: I’d like to amplify on that. One interesting thing is that most of these patients don’t really complain that the light seems brighter than normal. Most of the time, they’re complaining that a certain brightness of light is causing them to feel pain, and the questionnaires that Kathleen mentioned try to capture some of that. It’s not just that the patient reports that the light is brighter, it’s that the patient has an adverse response to a normal brightness of light.
Ocular Causes
Dr. Levi: What are the most common ocular causes that lead to photophobia?
Dr. Digre: I think the number-one thing is dry eyes or dry eye symptoms. This can occur as people get older, as in your patient. Previous corneal injuries or inflammation may change the corneal nerve structure and lead to more light sensitivity and photophobia or pain with light. Photophobia also can occur with any kind of inflammation in the eye, such as iritis, vitritis, or uveitis. And then even in the posterior segment, people who have albinism—or some of the achromatopsias, cone dystrophies, or retinitis pigmentosa—are extremely light sensitive.
Impact of Surgery. Dr. Levi: What about factors such as contact lens use or LASIK?
Dr. Digre: I’ve certainly seen many people who’ve had LASIK or cataract surgery or some other surgical procedure become more light sensitive. Again, sometimes it starts out with a dry eye complaint—but treating the dry eyes, as you did in your patient, does not seem to ameliorate their light sensitivity.
Dr. Kardon: Some of the emerging science behind this is that there are different sensory channels in the trigeminal nerves that innervate the cornea, and they have different functions. Some sense temperature. Some sense acid content. Some are multimodal channels. Some sense just mechanical touch. And some of these channels—and the nerve transmitters in the nerve that mediates them—probably become disturbed after some of the corneal procedures, and they give the feeling of dry eye even though, for example, the eye may be producing tears.
Further research will elucidate how the sensory channels in the cornea modulate light sensitivity and abnormal trigeminal activation during transduction of the signals. Future investigations will focus on how to test these corneal sensory channels: How do you determine if they’re abnormal, and how can you restore the normal sensory function of corneal channels?
Corneal Neuropathy. Dr. Levi: Kathleen, there’s a concept called corneal neuropathy that’s been presented by Perry Rosenthal in Boston. Can you make a few comments about that in light of Randy’s comments?
Dr. Digre: Well, we have looked at corneal nerves in people who have chronic migraine, for example, and there’s some indication that there may be some changes in the corneal nerves. But what’s the chicken and what’s the egg? Are the corneal nerves abnormal—do they take somebody with migraine, like your patient, and turn them into a chronic migraineur? Or is the migraine process actually producing changes in the corneal nerves?
I think Randy’s point about what we’re learning about the cornea is extremely important. We need much more science on the nerves that innervate the cornea as well as these channels. The nerve factors, growth factors, and transmitters are going to turn out to be very important. And so I think there is something like corneal neuropathy. These are people whose corneal nerves are not normal. They have atypical corneal sensation, and they tend to have really bad photophobia.
 |
|
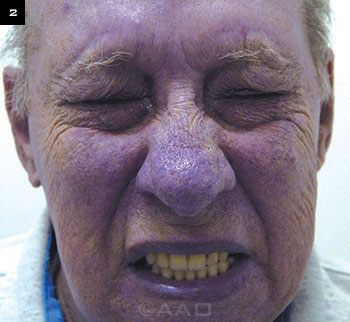
Reflexive blepharospasm is a common nonocular condition associated with of photophobia.
|
Nonocular Causes
Dr. Levi: For most ophthalmologists, the most frustrating patient is the one who’s complaining of photophobia but has a completely normal ophthalmological examination. What are the most common nonocular conditions associated with photophobia?
Migraine and Blepharospasm. Dr. Digre: The first and most common neurologic disorder is migraine. It affects 20% of all women, 10% of all men. As with the patient presented in your case study, photophobia patients often have a history of migraine, and it tells you something about their brain and the way they process pain that can set them up for things like chronic photophobia.
The second one is blepharospasm. Blepharospasm is not just sitting there blinking and squeezing the eyes; there are different types of blepharospasm. Some are just reflexive blepharospasm —in other words, the patient is reflexive to bright light and can be in normal light and not have a problem, but as soon as the bright light hits them, they go into blepharospasm attacks (Fig. 2).
Other neurologic conditions should be considered. For example, pituitary tumors can present with the chief complaint of photophobia. Progressive supranuclear palsy, a kind of Parkinsonism, has been associated with photophobia. Meningitis—anything that affects the meninges—can cause photophobia. Even medications have been associated with photophobia.
Traumatic Brain Injury. Dr. Kardon: One of the common emerging causes that we’re seeing, both in the veteran population and in sports, is that traumatic brain injury and concussions also seem to trigger light sensitivity. In veterans who have returned from recent battle, about 59% report light sensitivity. And the brain injury often causes a migraine-like headache in addition. And so we have a mixture of light sensitivity and headache that worsened after traumatic brain injury. It’s not uncommon for people to show up in the waiting room wearing very dark sunglasses who are disabled and who’ve had a history of concussion and traumatic brain injury.
Dr. Levi: A lot of patients are in motor vehicle accidents, for example, and are rear-ended and have whiplash, and that’s followed by various headaches and photosensitivity. In my practice, that’s a common scenario as well.
Complexity of Pain. Dr. Levi: Many patients who’ve had a concussion and who complain of photosensitivity also have a migraine history. Randy, do you see patients who have no migraine history but then do have photophobia after concussions or traumatic brain injuries?
Dr. Kardon: Almost all of these cases seem to be associated with headache and migraine-like symptoms, in my experience. The light triggers headache, so an important question to ask is, “Are you light sensitive but have no headache from it, and you just feel an aversion to light—or is headache a major component of this?” Most of the time, headache is a major component to the light sensitivity.
Dr. Digre: And it may not just be a headache. It could be eye pain as well. And neck pain, because the trigeminal system also serves some portions posteriorly—so there could be eye pain and neck pain as well as whole head pain.
Dr. Kardon: I agree with that completely.
More on Pituitary Tumors. Dr. Levi: Kathleen, just to elaborate on the point you made that some people with pituitary tumors can be light sensitive. I presume that those patients would have some compression of the chiasm or the optic nerves that might show up on another examination such as a visual field (VF) test that can be done in the office.
Dr. Digre: You could do a VF, but it’s probably the stretch of the dural sheath around the pituitary—again, the dura and the meninges of the brain are innervated by the trigeminal system. So getting a VF is a good first start. Then, maybe asking—both women and men—about galactorrhea or changes in ring size and hat size; those might be reasonable to do in the office.
More on Migraines. Dr. Levi: Can you talk about photophobia in patients with migraine even when they’re not having a headache? A lot of them seem to just be generally more light sensitive than the rest of us.
Dr. Digre: That’s been shown in numerous studies. For the experience of migraine headache, one of the key components is photophobia; 90% or more of people with a migraine will have photophobia. Sound sensitivity is another question to ask that points to migraine. Nausea, also, can go along with migraine. But even between migraine attacks, these individuals have been shown to be more light sensitive. In fact, one study was done just asking people, “Are you light sensitive all the time?” If they answered “Yes,” it was very predictive of them having underlying migraine, even though they weren’t wearing dark glasses in the office or anything like that. They were light sensitive all the time.
Dr. Kardon: I would echo that. Besides light sensitivity, migraineurs, between episodes, seem to be more sensitive to other modalities of stimulation. Referring back to your patient with regard to how sensitive she was to computer screens, it was probably movement. Responses to different types of sensory stimulation and different types of visual stimulation commonly seem to be overexaggerated in migraineurs, even when they’re not having a migraine.
More on Computer Use. Dr. Levi: What is it about computer screens? This is such a common complaint. I certainly hear in my practice about how patients can do everything else, but the computer screen or some other screen or fluorescent lighting really bothers them.
Dr. Digre: Well, fluorescent lights and some computer screens have a little oscillation and movement. As Randy said, this movement—any movement in the periphery—is a great trigger for developing a migraine.
These people just are extremely sensitive to all sensory input and movement and contrast. Heavily contrasted or figured items—stripes or checkerboards or anything with contrast and pattern—can really trigger migraines in certain susceptible people.
___________________________
Dr. Digre is professor of ophthalmology and visual sciences and neurology at the John A. Moran Eye Center at the University of Utah in Salt Lake City. Relevant financial disclosures: None. Dr. Kardon is professor of ophthalmology and visual sciences and director of the Neuro-ophthalmology Service at the University of Iowa in Iowa City. Relevant financial disclosures: Department of Defense TATRC: S; MedFace: O; National Eye Institute: S; Novartis: C; Veterans Health Administration: S. Dr. Levi is director of ophthalmology at Scripps Clinic in La Jolla, Calif. Relevant financial disclosures: None.
See the disclosure key at www.aao.org/eyenet/disclosures.