Download PDF
A patient tells you anxiously that he’s started seeing shimmering light around his wife—and also around his coffee cup and other ordinary objects. Another patient says she sees strange bugs crawling on her skin. How do you respond?
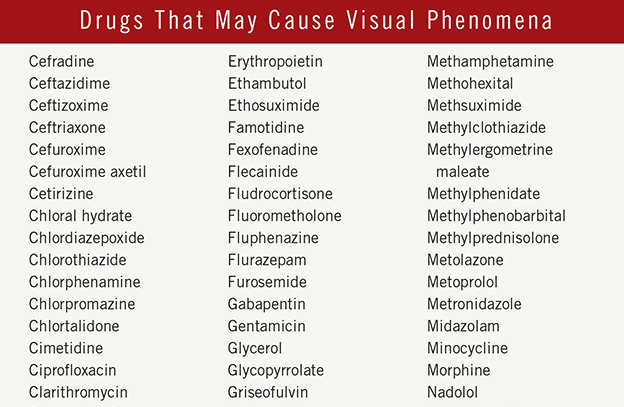
Although visual phenomena often have an ocular cause, the ophthalmologist should rule out ocular etiologies while considering systemic or ophthalmic drug side effects. One important question to ask such patients, said Frederick W. Fraunfelder, MD, MBA, is whether they’ve started taking a new medication or higher doses of their usual medications. Dr. Fraunfelder is an expert on medication-related visual disturbances and hallucinations at the University of Missouri, Columbia.
“Visual hallucinations are commonly caused by certain medications and are even more likely when a patient is taking several meds,” said Dr. Fraunfelder. “A person using just one medication is much less likely to experience a related visual hallucination than someone who’s on four or five, due to potential drug interactions.” He added that older patients are more likely than younger patients to be receiving treatment for several conditions and may be at greater risk.
Most ophthalmologists will encounter patients with medication-related hallucinations at some point in their career. Neuro-ophthalmologist Bokkwan Jun, MD, PhD, at the University of Missouri, Columbia, estimates that 1 of every 100 of his patients reports hallucinations that turn out to be related to medication. He noted that it is important to keep several considerations in mind when managing such patients.
The Ophthalmologist’s Role
Visual hallucinations are a personal and subjective experience, said Dr. Jun.
What to ask. “Through taking a detailed patient history, the ophthalmologist can try to determine whether the hallucination is monocular or binocular, where it occurs in the visual field, whether it moves around, when and how often it occurs, and how long it lasts,” said Dr. Jun. “If your patient has a psychiatric condition or drug or alcohol abuse problem, getting an accurate description may be more difficult, since the patient’s report may not be fully reliable.”
Note that some patients may be reluctant to admit they’re having hallucinations for fear that they may be sliding into dementia or will be labeled as crazy. They are likely to be relieved to learn that a medication could be causing their visual disturbances and that adjusting or switching their regimen might bring relief, said Dr. Jun.
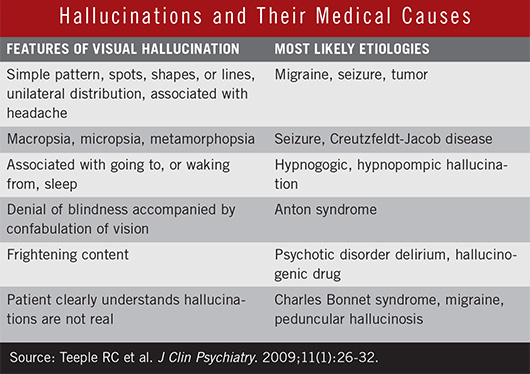
Rule out medical causes. Because hallucinations can have more than one cause, ophthalmologists should inquire about medical conditions that could be involved, said Dr. Jun. These include migraine, posttraumatic stress disorder, tumor, and Charles Bonnet syndrome, a relatively common condition in which patients with visual loss see complex formed images. If warranted, order a blood test to detect drugs or alcohol. (See “Hallucinations and Their Medical Causes.")
When drugs are the problem. If you determine that a medication or drug interaction is causing significant visual disturbance, the next step is to confer with your patient’s primary care physician and cardiologist, neurologist, or psychiatrist as needed, on the overall treatment plan, said Dr. Jun. Discuss whether adjusting, changing, or eliminating the problem medication is an option.
If the current medication is the only or best option, consider whether education or support could help the patient cope with disruptive hallucinations, he said. In most cases, patients know their hallucinations aren’t real. Some patients find hallucinations relatively easy to ignore, especially if they understand that the medications causing the effects are important to their overall health, he said.
Web Extra: Clinical Update
|
 |
Common Culprits
It’s important to ask patients to describe their experiences in detail because different types of drugs cause distinctly different visual effects, ranging from colorful auras to highly realistic images.
Types of hallucinations. Dr. Jun defines a hallucination as a visual perception or distortion that cannot be explained by external visual stimuli. Simple hallucinations, also known as elementary or nonformed, appear as lights, colors, lines, shapes, or geometric designs; complex, or formed, hallucinations may include images of people, animals, objects, or lifelike scenes.
The medications most often associated with visual hallucinations include those used to treat high blood pressure, erectile dysfunction, psychiatric and mood disorders, movement disorders like Parkinson disease, and some antibiotics, Dr. Fraunfelder said. He recommends asking all new patients, as well as anyone you suspect may be experiencing visual disturbances, whether they are being treated for these conditions.
Vasoconstrictors or vasodilators. Visual phenomena can result from constriction or dilation of the middle cerebral artery, which supplies the occipital cortex, or other key blood vessels. Widely prescribed drugs of this type include blood pressure medications, especially beta-blockers, and antianginal drugs like nitroglycerin. All vasodilator/constrictor drugs can cause patients to see shimmers or halos outlining objects. Scintillating phenomena are also common. This is typically described as a luminous appearance that is accompanied by a jagged outline.
People who take Viagra or other erectile dysfunction drugs may perceive a distinctive bluish tinge in their vision. These drugs have dose-dependent effects: For example, only about 5 percent of patients taking 50 mg a day have symptoms, but 100 percent of patients taking 200 mg a day will be affected, said Dr. Fraunfelder.
Medications intended to affect the brain itself. These may be antiseizure medicines or psychotropic drugs taken by patients with psychiatric illnesses or mood disorders. Hallucinations caused by these drugs are usually more vivid, detailed, and seemingly real than those caused by the vasoconstrictors/vasodilators.
Antibiotics. The antibiotics most frequently associated with hallucinations are cephalosporins and the sulfa drugs. Again, the effect is more common in patients taking multiple medications. “Just why antibiotics cause hallucinations is uncertain,” said Dr. Fraunfelder, “but numerous patient reports document disturbing hallucinations or vivid nightmares associated with taking antibiotics.”
Dopamine agonists. These are used to treat Parkinson disease and other disorders involving motor control. The quality of hallucinations can range from fleeting images that last only a second to elaborate formed images that can be disorienting or frightening. Use of dopamine agonists for Parkinson’s poses a conundrum because the medication also helps to control visual dysfunction caused by the disease.
Dr. Jun notes that dopamine agonists are also prescribed, in lower doses, for restless leg syndrome (RLS), a condition that affects an estimated 2.5 to 15 percent of the population. RLS interferes with restful sleep; it affects twice as many women as men and may worsen with aging.
(click to expand)
|
Web Extra: Clinical Update
|
 |
Other Medications
In rare instances, a patient can experience visual hallucinations while taking a drug not commonly associated with this side effect. The case of a retired cardiologist offers one illustration. Her story was relayed by her husband, retired ophthalmologist, Jerry Jacobson, MD, of Ogdensburg, N.Y.
“Soon after she started taking Fosamax [alendronate] for osteoporosis, she told me she’d started hearing ‘voices in her head’ and experiencing red-colored visual disturbances,” said Dr. Jacobson.
As a physician herself, Dr. Jacobson’s wife did not hesitate to report the hallucinations to her own doctor, who agreed that Fosamax was most likely the culprit and promptly modified her regimen.
Other bisphosphonates (e.g., etidronate, pamidronate) have reportedly caused reversible and irreversible visual—as well as auditory and olfactory—hallucinations within two hours and up to a week after initiation of the drug.1 The causative mechanism is not fully understood but is thought to be independent of calcium homeostasis.
The Take-Home Message
If a patient describes visual hallucinations to you, or you have reason to think he or she may be experiencing visual disturbances, it’s important to assess both the patient’s medication use and the nature of the hallucinations as you develop a treatment plan. Keep in mind that even drugs not usually associated with hallucinations can cause central nervous system toxicity in rare cases.
___________________________
1 Coleman CI et al. Pharmacotherapy. 2004; 24(6):799-802.
___________________________
Frederick W. Fraunfelder, MD, MBA, is Chairman and Distinguished Professor of Ophthalmology at the Mason Eye Institute at the University of Missouri, Columbia. Financial disclosure: None.
Jerry Jacobson, MD, retired ophthalmologist Ogdensburg, N.Y. Financial disclosure: None.
Bokkwan Jun, MD, PhD, is assistant professor of ophthalmology at the Mason Eye Institute, University of Missouri, Columbia. Financial disclosure: None.