Download PDF
In recent decades, a leading trend throughout all the surgical specialties has been to reduce the size of incisions and area of manipulation—as, for example, in laparoscopic gallbladder surgery or arthroscopic knee repair—in hopes of decreasing tissue trauma, patient discomfort, and complications. These “minimal access” procedures have been made possible by the increasing miniaturization and sophistication of instrumentation and imaging technologies.1
This less-is-more approach is especially suitable for the small spaces and delicate tissues encountered in ophthalmic surgery. Phacoemulsification for cataracts and miniature drainage implants for glaucoma are examples of this trend. Similarly, minimally invasive strabismus surgery (MISS) is designed to be a kinder and gentler way to access the extraocular muscles. However, the technique is controversial and has not yet gained wide acceptance.
Here is a look at some of the techniques and indications for MISS, as well as considerations that may affect its widespread adoption. What does the future hold for this novel surgical approach?
What Is MISS?
Although several strabismus surgeons employ small-incision or “mini” techniques,2,3 the term MISS is most frequently associated with Daniel S. Mojon, MD, who is head of the Airport Medical Center Eye Clinic, Zurich, Switzerland. He first reported it in 2007 as a new way to gain access to the horizontal rectus muscles for recession or plication.4
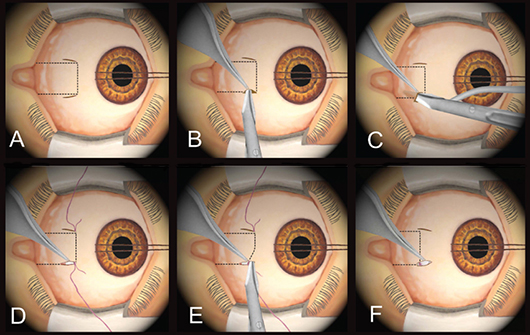
MISS surgical approach. The hallmark of MISS is the placement of several keyhole openings, rather than one large conjunctival opening (Figs. A-C). This technique is also demonstrated in a video available at www.aboutmiss.com/pages/publications-about-miss.html.
Incisions are placed where the main surgical steps will be performed, as far from the limbus as possible. The placement of the keyhole cuts makes it possible to convert to the usual large limbal opening, if necessary for increased visibility or other surgical considerations. This placement also preserves the majority of the perilimbal episcleral vessels, thus reducing the risk of postoperative corneal complications, particularly ischemia. “As long as the conjunctiva is not cut at the limbus, you and your patients will immediately notice a difference for the better,” Dr. Mojon said.
MISS may be performed with the same instruments used for standard, open surgery; however, it does require an operating microscope.
|
Step-by-Step MISS
|
 |
|
ACCESSING THE MUSCLE (for either recession or plication; dotted line indicates underlying horizontal rectus). (A) A limbal traction suture is used to rotate the eyeball away from the field of surgery. Two small cuts are made at the upper and lower muscle margins. Size of cuts depends on amount of muscle to be displaced. (B) With the two cuts as access points, the episcleral tissue is separated from the muscle sheath and the sclera with a blunt Wescott scissors. (C) After the muscle borders have been identified, the muscle is hooked, and the check ligaments and intramuscular membrane are dissected 6 to 7 mm behind the insertion. The resulting tunnel allows a recession or plication to be easily performed. RECESSION. (D) For a recession, two sutures are applied to the superior and inferior borders of the muscle tendon as close as possible to the insertion. (E) The tendon is detached using a Wescott scissors. (F) After the amount of recession is measured, the tendon is reattached with two sutures to the sclera. The tendon must be stretched to keep the central part of the muscle from bowing backward. Continue to J to complete the operation or to G to add a plication (see below).
|
Benefits of MISS
Dr. Mojon has used both the Harms limbal and Parks fornix techniques, but MISS, he said, “dramatically” reduces surgical trauma and improves quality of life in the immediate postoperative period. “I was looking for an approach that further decreases the need for tissue dissection and that also may be used for complex revision surgeries in badly scarred muscles.”
Dr. Mojon first described MISS in a report on a series of horizontal rectus muscle operations.4 He used the MISS technique in 20 patients (25 eyes, 39 muscles) and the “usual limbal approach” in 20 controls (24 eyes, 38 muscles). Although there was no difference in long-term results, in the immediate postoperative period, MISS was superior in terms of visual acuity and lid swelling.
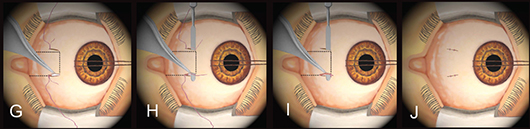
The technique established in these horizontal rectus muscle operations may be applied to all types of strabismus surgery, said Dr. Mojon, including rectus muscle recessions (Figs. D-F), resections, plications (Figs. G-I), reoperations, retroequatorial myopexies, transpositions, and oblique muscle recessions or plications. One exception, however, is reoperation on an already strongly recessed rectus muscle with very restricted ocular motility. For example, in a case of severe thyroid orbitopathy, Dr. Mojon said he would use the Harms limbal approach to better visualize the muscle.
According to Dr. Mojon, the advantages of MISS include the following:
- Surgical openings are covered by the eyelid postoperatively.
- Perilimbal episcleral vessels are preserved, reducing the risk of ischemia.
- Fewer corneal complications, such as dellen formation.
- Decreased scarring of the perimuscular tissue, thus facilitating reoperations
- Reduced redness of the visible conjunctiva.
 |
|
PLICATION. Plication may be performed independently (continuing from part C) or added to recession (continuing from part F). (G) Two sutures are applied to the upper and lower borders of the muscle at the distance from the tendon insertion site corresponding to the amount of plication, and the sutures are passed at the superior and inferior tendon insertions. (H) An iris spatula is inserted between the tendon and the sutures, and (I) the muscle is plicated. (J) Incisions are sutured.
|
Learning curve. Dr. Mojon estimated that about 10 doctors in the United States and 60 more around the world have visited his operating theater and adopted the technique. If less is more, why haven’t more surgeons embraced it? Linda R. Dagi, MD, director of Adult Strabismus at Boston Children’s Hospital, Harvard Medical School, speculated that surgeons accustomed to working with loupes may be discouraged by the use of an operating microscope and the need to work inside a small incision. The benefit to the patient may seem relatively small, she said. And the learning curve is steep. Dr. Mojon acknowledged that most surgeons need a couple of hundred surgeries to feel comfortable with MISS.
Is another technique needed? In publications and presentations, Dr. Mojon generally compares MISS against the limbal approach. Dr. Dagi noted that “if you compare MISS to that, the [MISS] eyes look far better the next day. However, the limbal approach is one I rarely use.”
Dr. Dagi conjectured that MISS may be more attractive to surgeons who ordinarily use a limbal approach. “It’s certainly nicer than having an incision extending all the way from the limbus.” Compared to the limbus-based approach, she said, MISS is analogous to a bikini incision used in abdominal surgery.
Fornix-based procedures are successful. “In the center where I’ve trained and teach, the majority of us use a fornix-based incision,” Dr. Dagi said. “This approach results in minimal postoperative edema or discomfort, and the incision is usually hidden from view.” MISS doesn’t appear to offer much advantage for surgeons already using a fornix-based approach, she added. And it has some disadvantages, specifically, the challenge of working around scar tissue in an enclosed area or trying to stanch bleeding through a small incision.
Although David B. Granet, MD, is enthusiastic about Dr. Mojon’s work, he still hasn’t tried MISS. “We think our [fornix] surgery is already minimally invasive,” he said, adding that his approach, like MISS, avoids disruption of the episcleral perilimbal vessels. “We make very small incisions, hook muscles through these tiny incisions, keep bleeding to a minimum. We have a pretty slick surgery now,” he said. “I’ve been so happy with my technique, and our outcomes have been so good, that I don’t feel the pressing need to change,” he added. Dr. Granet is professor of ophthalmology and pediatrics at the University of California, San Diego.
Finding a role for MISS in practice. Although Dr. Dagi is willing to try MISS, she doesn’t expect it to play a large role in her referral practice, which typically handles reoperations, often in scarred eyes. But she thinks it could have a place in a traditional practice that deals mostly with primary strabismus surgeries, in particular, recessions. “And it’s great for Faden retroequatorial sutures,” she added. “You can forgo the primary incision and just make a small opening through the conjunctiva and Tenon’s directly adjacent to the region where the retroequatorial suture will be placed. That’s an incredibly novel solution, particularly if you’re not recessing the muscle at the same time.”
Switching to MISS
When surgeons ask Dr. Mojon how to switch from standard, open surgery to MISS, he suggests that they come to watch in the operating theater and assist one day. “That’s really the best before starting.”
He recommends beginning with a primary horizontal rectus muscle displacement of 4 mm or less. Use a corneal traction suture and create plications instead of resections, which are more difficult to accomplish through small cuts.
The ideal patient is between the ages of 14 and 40. The abundant Tenon tissue in very young patients can complicate the surgery. In much older patients, the conjunctiva has lost elasticity, increasing the risk of a conjunctival tear.
Although experienced surgeons can use MISS for most types of surgery, Dr. Mojon said, “If you are not experienced, you should only use MISS for small deviations, for virgin eyes, and for simple deviations.” If necessary, the MISS procedure can be converted to a standard procedure by creating a longer incision.
PEARLS FROM DR. MOJON
- Visit an experienced MISS surgeon.
- Practice using the operating microscope with your own procedure before using it for MISS.
- Don’t hesitate to start with two large openings.
- Rule of thumb: The opening cut will be 1 mm less than the amount of muscle displacement to be achieved. For example, a recession or plication of 4 mm can be performed through two 3-mm openings.
- Try 100 cases before giving up.
|
What Does the Future Hold?
Two opinions. Edward Buckley, MD, questioned the added value of a minimalist approach in eye muscle surgery. The surface tissue disruption doesn’t affect a successful outcome, he said, adding that a well-done fornix or limbus-based procedure won’t produce much scarring. “I think MISS is interesting, but I don’t think it’s going to be something a lot of folks are going to adopt,” he said. Dr. Buckley is professor of ophthalmology and pediatrics and dean for medical education at Duke University.
Dr. Granet said that MISS is part of a minimally invasive current flowing through all of medicine. “What we’ve learned from general surgery is that the less invasive, the less traumatic, the better it is for the body,” he said.
Dr. Dagi agreed. “The concept of minimally invasive surgery is appealing generally to surgeons, but more particularly to the public. They like less invasive [procedures]. It has a kind of street appeal.”
Greater awareness about MISS. Dr. Granet suggested that surgeons may need to hear about MISS multiple times before trying it. “Dr. Mojon is taking something that we consider a done deal and looking at a whole new way of approaching strabismus surgery,” he said. “The surgical principles he is using are very sound. He secures the muscle carefully. He just does it through a much smaller opening.”
Dr. Granet predicted that a new generation of doctors may learn MISS along with the standard techniques, the way he was required to learn both extracapsular cataract extraction and phacoemulsification.
Finding the best surgery. “In the end, we all have the same goal—to accomplish an improvement in outcome with the least amount of impact to the eye,” Dr. Granet said. “We’re always trying to impact the eye less and less.”
The beauty of MISS, he continued, is that it gets surgeons to ask: What can we do differently? What can we do better? “We’re not far away from what he’s doing. Our small fornix incision is pretty good. But I owe it to myself to see the new techniques,” he said. “If a patient has less pain in the first 24 hours, isn’t that enough of a goal? And if recovery is a day faster, isn’t that better for the patient? The biggest issue for me is keeping our minds open and listening to new approaches. Daniel Mojon is making us rethink some of the things we thought we already knew.”
___________________________
1 Darzi A. BMJ. 2002;324(7328):31-34.
2 Jethani J et al. Indian J Ophthalmol. 2009;57(6):477-478.
3 Leenheer RS, Wright KW. J AAPOS. 2012;16(4):327-330.
4 Mojon DS. Br J Ophthalmol. 2007;91(1):76-82.
___________________________
Drs. Buckley, Dagi, Granet, and Mojon report no related financial interest.