By Louis Savar, MD, Patrick Coady, MD, and Rona Z. Silkiss, MD
Edited by Steven J. Gedde, MD
Download PDF
Jane Smith,* a 32-year-old woman, was dropped off at the airport after a long weekend visiting family. The one-hour commercial flight seemed uneventful. After catching a taxi from the airport, she went to bed. When she woke the next morning, she was distressed to experience pain, lid swelling, and blurry vision in her left eye. After suffering for 10 hours, she arrived at the emergency department.
Early Misdiagnosis
Examination by the emergency staff demonstrated a fixed pupil in the left eye with an intraocular pressure of 60 mmHg. Blood pressure was normal.
Her past medical history included intravenous drug abuse, for which she was currently taking methadone. She denied any history of trauma or surgery, or recent straining, vomiting, or headaches.
She was treated for the presumptive diagnosis of angle-closure glaucoma and given acetazolamide intravenously. We were consulted.
What We Saw
Our examination in the emergency department revealed visual acuity of 20/20 in the right eye and 20/400 in the left. There was an afferent pupillary defect in the left eye. Intraocular pressure was 13 mmHg in the right eye and 22 mmHg in the left. Extraocular motility was full in the right eye and limited in all directions in the left eye.
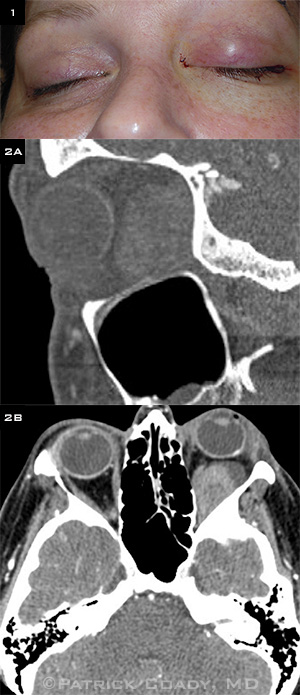
The left eye was proptotic without bruit. The left eyelids were edematous, and there was significant resistance to retropulsion on the left side (Fig. 1). The funduscopic examination was normal.
What Tests Revealed
Laboratory tests—including platelet count, partial thromboplastin time (PTT), and international normalized ratio (INR)—were normal. A urine drug screen was negative.
CT with contrast of the orbits revealed a large mass with multiple densities occupying the majority of the inferolateral left orbit (Figs. 2A, 2B). The intraconal location of the mass displaced the rectus muscles and optic nerve, and there was significant proptosis of the globe. The remainder of the scan, including the sinuses, was normal.
|
What's Your Diagnosis?
|
 |
|
(1) The patient complained of a swollen left eyelid. We reviewed (2A) sagittal and (2B) axial CT images.
|
Treatment
We performed a lateral canthotomy and inferior cantholysis to relieve the orbital compartment syndrome. After 30 minutes, the patient’s status remained unchanged, and we took her to the operating room for definitive treatment.
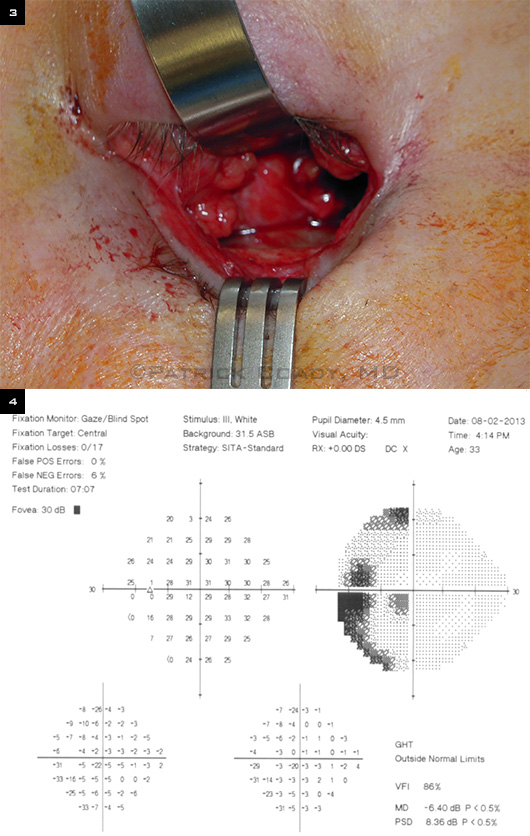
General anesthesia was administered, and we performed an orbitotomy, using a lower lid–transconjunctival approach. Blunt dissection through the orbital fat revealed dark, clotlike material (Fig. 3). We submitted a portion of this for histopathological examination and evacuated the remainder. There was no other obvious soft-tissue abnormality.
Hemostasis was secured and the orbit decompressed considerably at the conclusion of the procedure.
By postoperative day three, the patient’s visual acuity had improved to 20/25 in her left eye, with full extraocular motility and a trace afferent pupillary defect. On postoperative day five, automated visual field testing of the left eye showed a paracentral and arcuate scotoma inferotemporally (Fig. 4). We ordered magnetic resonance imaging, but the patient was lost to follow-up.
The pathology report noted blood with fibroadipose and vascular tissue. There was no evidence of malignancy.
 |
|
WE OPERATE. (3) Intraoperative photograph of the orbitotomy with clotlike material visible through the periorbital opening. (4) On postoperative day five, 24-2 Threshold Humphrey Visual Field (HVF) testing of the left eye.
|
About the Condition
Intraorbital hemorrhage is a rare entity, which most commonly presents in association with an identifiable underlying etiology such as trauma, vascular malformation, bleeding diathesis, sinusitis, surgery, neoplasm, or hypertension.1-4
Sullivan and Wright reviewed all cases of nontraumatic orbital hemorrhage presenting to their clinic over a 24-year period. Of the 115 cases, only six had no orbital vascular anomaly or other identifiable predisposing factor. Approximately two-thirds of the patients had complete resolution without intervention. Interestingly, there was a bimodal age distribution, with one peak before 20 years and a smaller peak after 50 years of age. Among patients younger than 20 years, an orbital vascular anomaly was present in 97 percent; among patients older than 50 years, it was present in 62 percent. The authors conjectured that orbital hemorrhages in the older group were more likely attributable to vascular, connective tissue, and circulatory changes that occur with age. The authors observed that hemorrhages in the younger patients tended to be encysted or localized, while those in the older patients tended to be diffuse, likely due to changes in the orbital connective tissues.5
Although reports in the literature often do not specify the location of the hemorrhage anatomically within the orbit, several recent series describe subperiosteal locations. In one report, Crawford and Mazzoli discuss three cases of spontaneous subperiosteal hemorrhage, all of which required surgery. All were located in the superior orbit and had associated predisposing factors: violent emesis, facial trauma after motor vehicle accident, and Valsalva maneuver while scuba diving. Each patient had at least 20/40 vision or better, had no afferent pupillary defect on presentation, and was observed for between two and 10 days before surgical intervention.6
Our Case Was Urgent
Ms. Smith developed an intraconal hemorrhage extending to the edges of the orbital soft tissues. Because of the grave presentation with optic nerve compromise, she required urgent treatment.
In mild cases, more conservative treatment such as steroids or observation alone may be sufficient.7 It is important not to overlook other possible orbital masses when considering the differential diagnosis. Subacute orbital hemorrhages also may be present and can easily be confused with other space-occupying lesions of the orbit.8
Identification and treatment of the underlying pathology that led to the hemorrhage, such as a vascular anomaly or a neoplasm, is imperative.3 In our case, despite imaging and surgical exploration, no underlying pathology was identified at the time of presentation and treatment.
Conclusion
Orbital hemorrhage is one of the few true ophthalmic emergencies. Spontaneous hemorrhages without predisposing factors are exceedingly rare but should be in the differential diagnosis of acute pain, proptosis, and visual decline. Workup must include a review of the patient’s medical history and a complete ophthalmic examination with particular attention to the orbit and optic nerve. Accurate anatomical localization of the hemorrhage may help determine the etiology and best approach for management.
___________________________
* Patient name is fictitious.
___________________________
1 Krohel GB, Wright JE. Am J Ophthalmol. 1979;88(2):254-258.
2 Wolter JR. Trans Am Ophthalmol Soc. 1979;77:104-120.
3 Yoon MK, McCulley TJ. Ophthal Plast Reconstr Surg. 2012;28(4):e79-80.
4 Yoshimoto M, Matsumoto S. J Cataract Refract Surg. 2004;30(3):722-725.
5 Sullivan TJ, Wright JE. Clin Experiment Ophthalmol. 2000;28(1):26-31.
6 Crawford C, Mazzoli R. Digit J Ophthalmol. 2013;19(1):6-8.
7 Wiwatwongwana D, Wiwatwongwana A. Graefes Arch Clin Exp Ophthalmol. 2012;250(10):1557-1558.
8 Matsuura H et al. Neurol Med Chir (Tokyo.) 1995;35(1):45-47.
___________________________
Dr. Savar is an ophthalmic plastic and reconstructive surgery fellow, Dr. Coady is a third-year ophthalmology resident, and Dr. Silkiss is chief of ophthalmic plastic and reconstructive surgery; all are at California Pacific Medical Center. The authors report no related financial interests.
(click to expand)
