Download PDF
Once dismissed as a fringe interest in ophthalmology, nutrition gained mainstream respect when AREDS showed its effect in macular degeneration. Sample some of the latest findings from a smorgasbord of research.
Several major population-based studies have pointed to the influence of dietary factors in eye health, and AREDS1 and 2 homed in on specific micronutrients that affect the course of age-related macular degeneration (AMD).
Researchers are continuing to press forward, looking at a range of nutrients—delivered through foods or supplements—not only in retinal conditions but also in dry eye, cataract, and glaucoma. And, as a healthy bonus, some of the nutrients found to be beneficial to the eye may prove helpful to the joints, skin, and cardiovascular system as well. Good nutrition could well be our best bargain in health care.
Retina: Evolutionary Effects
The retina is the most metabolically active tissue in the body. It has the highest demand for oxygen and gets nearly constant exposure to light. This creates high vulnerability to light-initiated oxidative damage. Fortunately, our eyes evolved to be highly responsive to nutritional factors that are protective against such stress, said Billy R. Hammond Jr., PhD, at the University of Georgia in Athens.
Carotenoids: protective pigments. The most important of these protective factors for the eye are carotenoids, organic pigments derived from plant sources, which counteract the ravages of free radicals. Of the hundreds of carotenoids found in nature, just two end up in the retina, said Elizabeth J. Johnson, PhD, at Tufts University. They are lutein and zeaxanthin—isomers of each other—both abundant in leafy greens, such as spinach and kale. These carotenoids make up the macular pigments, which give the macula its characteristic yellow color.
“If you don’t get them from your diet, however, you don’t have them at all,” Dr. Johnson said, adding that while the average intake of lutein in the United States is about 1 to 2 mg a day, some cultures get up to 20 mg daily. “Epidemiology suggests that we need about 6 mg a day.” When present in sufficient concentration, these macular pigments fill many ocular needs.
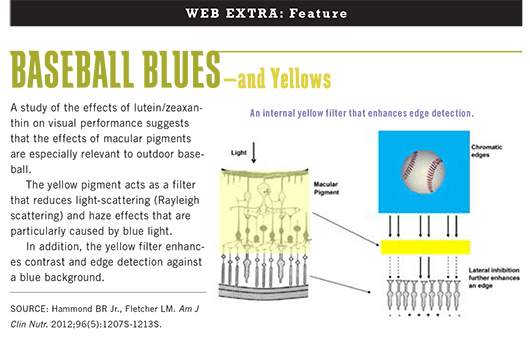
Absorbing harmful rays. “Although the cornea and crystalline lens absorb most of the long-wave component [of light], the retina’s macular pigments help filter out the short-wave component that is most pernicious to vision,” said Dr. Hammond. “It’s the 400 to 500 nanometer range of blue light that is energetic enough to turn oxygen into reactive oxygen and damage the retina."
Distance vision. Macular pigments also may have evolved at a time when distance vision was at a premium, for example, in answering survival question such as: Is that a lion? “Some studies show that—all things being equal—someone with high macular pigment can see about 20 to 30 percent farther than someone with low macular pigment,” he said.1
Internal sunglasses. Macular pigments are uniquely suited to reduce the effects of scattered light on the eye—another evolutionary bonus for our ancestors out on the savanna in the blazing sun. “By absorbing a lot of scattered light, they clean up the image, reducing glare disability,” said Dr. Hammond.
(click to expand)
Dietary Devolution?
Once brimming with these antioxidants, many eyes are now starved for them due to a dearth of these nutrients in contemporary diets. “Somewhere between 60 and 70 percent of all the food eaten on planet Earth today comes from about 10 species—corn, rice, cows, for example,” said Dr. Hammond. “These have been altered and grown to be high yield, yet less nutritious, and there are biological consequences to this."
Dramatic changes. “Our systems are still geared for the Paleolithic diets we had many thousands of years ago and not for processed foods containing refined grains, fats, sugar, salt, and additives,” said August L. Reader III, MD, at Pacific Eye Associates in San Francisco. Western diets are leading to increased inflammation and oxidative stress, speeding degenerative processes—whether in the macula of the eye or collagen of the joint. And adding insult to injury is the obesity epidemic, he said.
Multiple insults. Extra fat not only increases inflammation but also affects the concentration of certain nutrients in the body. The retina and the brain concentrate fat-soluble antioxidants, said Dr. Hammond, but so does fat. “And it’s hard to compete with an enormous amount of fat.” In addition, smoking and a high intake of alcohol have been linked to lower blood levels of certain antioxidants such as lutein.2
AMD: Micronutrients Slow Progression
“Macular degeneration is the sine qua non of ophthalmic research in free radicals and antioxidants,” said Dr. Reader. Interest in certain nutrients has stemmed from their high concentration in the retinal pigment epithelium and retina, as well as their anti-inflammatory and the retina.” antioxidant properties. Large population-based studies examining their effects have included the Beaver Dam Eye Study, Blue Mountains Eye Study, and Rotterdam Study.
The research that arguably has had the greatest impact on reining in AMD through nutrition is the Age-Related Eye Disease Study (AREDS), sponsored by the National Eye Institute. In 2001, AREDS researchers reported that a formulation of 500 mg of vitamin C, 400 IU of vitamin E, 15 mg of beta-carotene, 80 mg of zinc, and 2 mg of copper reduced the risk of progression to advanced AMD by 25 percent.3
AREDS2. The research didn’t stop with that achievement. “Beginning in 2006, the goal was to see if we could improve the AREDS formulation currently used as a treatment,” said Emily
Y. Chew, MD, who chaired the study. This work culminated in the 2013 publication of the AREDS2 report.4
For this second study, the research group tested 1,000 mg of omega-3 fatty acids, in the form of 650 mg of eicosapentaenoic acid (EPA) plus 350 mg of docosahexaenoic acid (DHA), and 12 mg of carotenoids consisting of 10 mg lutein plus 2 mg zeaxanthin. In previous studies, these dietary nutrients had been linked to a lower risk of advancing AMD, said Dr. Chew. For five years, more than 4,000 AREDS2 participants from 82 sites added one of the following regimens to the AREDS1 formulation they were already taking: lutein/zeaxanthin (L/Z), omega-3 fatty acids, both, or placebo. The researchers also tried substituting the two antioxidants for beta-carotene, which prior studies had linked with a higher risk of lung cancer in smokers and former smokers.
Lutein/zeaxanthin. Although these two carotenoids offered no overall benefit, said Dr. Chew, analyses comparing L/Z versus no L/Z showed a beneficial effect in reducing the risk of advanced AMD. Two subgroups benefited further, showing a significant reduction in advanced AMD in those taking a formulation containing L/Z but no beta-carotene and in those with a low dietary intake of L/Z. Beta-carotene is known to suppress the absorption of L/Z, which could partly explain these results. More important, beta-carotene was found to double the risk of lung cancer in former smokers.
“In a head-to-head comparison,” said Dr. Chew, “lutein and zeaxanthin offered an additional effect of 20 percent above the effects of the AREDS formulation, especially in the prevention of neovascularization.” This incremental improvement may be important for such a huge public health problem, she added.
Omega-3s. These fatty acids were found to be safe but did not provide additional benefit for macular degeneration, at least in the supplement form AREDS2 used, said Dr. Chew. She added that many unanswered questions remain: Is there something in fish that’s absent from the supplement? Is the ratio of omega-3s to omega-6s a critical factor? “Clearly, the dietary data suggest we should eat a diet replete with fish and green leafy vegetables.”
Application of study findings. Given the results of AREDS2, the new formulation will substitute L/Z for beta-carotene but will not add omega-3s. Patients who may benefit from this supplement are not those with early drusen or early AMD, said Dr. Chew, but rather people with intermediate AMD or large drusen in both eyes or advanced AMD in one eye.
Concerns about interpretation. Although they applaud the addition of L/Z to the formulation, both Drs. Hammond and Johnson have concerns about how AREDS2 may be interpreted. This was a well-nourished, atypical population, said Dr. Johnson. “Supplementation helps when there’s a gap in nutrition.”
Nutrition studies are also inherently problematic, being essentially devoid of placebo. “The gold standard of medical evidence is the double-blind, controlled study, but you’ll never find someone who is ‘nutrient naive,’” said Dr. Hammond, adding that this was especially true in AREDS2, in which all participants—even those in the placebo group—were taking the AREDS1 formulation. “In addition, whole foods contain thousands of components with specific interactions, yet we test nutrients individually as if they were drugs.”
Further study. With sequestration and other funding constraints, there won’t be an AREDS3, said Dr. Chew, noting that it is possible that other nutrients are important. For example, the large, randomized Women’s Antioxidant and Folic Acid Cardiovascular Study found that those taking B vitamins reduced their risk of early macular degeneration by more than a third after seven years.5 The NIH is now also conducting a study of 20,000 patients, looking at vitamin D for cardiovascular disease and cancer, which will also provide information about macular degeneration.
“It would be great to have the opportunity to study primary prevention of AMD,” said Dr. Chew. “I think the pathways to drusen and then from drusen to advanced disease might be quite different. Those pathways need to be elucidated, and genetics may be helpful in understanding them.”
Caution: Avoid Excess Supplementation
Make sure your patients don’t fall for the “more is better” fallacy. “Every once in a while, I’ll have a patient come in with 17 bottles of supplements,” said Dr. Sheppard, “and find they’ve duplicated nutrients and become toxic.”
Zinc. For example, a patient could be taking separate supplements for macular degeneration, diabetes, and dry eye and not realize that they all contain zinc, he said. “Over time, it all starts to add up.” Excessive zinc intake above 100 mg/day may cause fever, fatigue, stomach cramps, dysgeusia, and fatigue, he said, and has been associated with an increased risk of prostate cancer.
Nutrients with anticoagulant properties. Be aware of the anticoagulation effects not only of vitamin E supplements but also of fish oil and Ginkgo biloba, said Dr. Sheppard. Make sure that patients know what to discontinue before eye surgery, when bleeding may present risks, he advised. These operations include trabeculectomy, iris reconstruction, eyelid surgery, dacryocystorhinostomy, orbital surgery, and pars plana vitrectomy.
Beta-carotene. It’s not entirely clear why beta-carotene increases the risk of lung cancer in smokers and former smokers. “But any antioxidant can become a pro-oxidant under the right conditions,” said Dr. Hammond, explaining that in high doses, beta-carotene may become a pro-oxidant in the lungs. “This doesn’t happen, however, when you get it from food,” as opposed to supplements.
Vitamin A palmitate. Before a patient starts taking this supplement, Dr. Berson recommends a fasting serum A and liver function profile. Patients over age 49 should have a bone density measurement; long-term vitamin A use slightly increases the risk of hip fracture. He also cautions that too much DHA can cause excessive release of vitamin A from IRBP, with possible long-term adverse effects; RP patients should limit oily fish to no more than two or three servings weekly. Women who are pregnant—or planning to be—should avoid high-dose vitamin A treatment due to increased risk of birth defects.
|
RP: Benefits From Supplements Plus Fish
The telltale night blindness that results from vitamin A deficiency is well known. Yet some physicians remain skeptical that something as simple as vitamin A can help ameliorate visual loss from a group of genetic diseases with more than 100 different causative genes, said Eliot L. Berson, MD, at Harvard University.
He has conducted three five-year randomized trials, exploring the potential benefit of vitamin A combined with other supplements for the typical forms of retinitis pigmentosa (RP) that lead to degeneration of the light-sensing rods and cones across the retina. Dr. Berson and colleagues subsequently developed the first nutritional regimen to slow the course of RP in adults.
Vitamins A and E. The first trial, conducted in the 1980s with 601 adults with RP, found that supplementation with 15,000 IU of vitamin A palmitate a day slowed the decline of retinal function. Optimal results were seen in patients who obtained about 3,000 IU of vitamin A more per day through their diet in addition to taking the study supplement. Higher amounts of supplementation produced no greater benefit, and lower intake was not therapeutic.
The study also looked at the effect of vitamin E supplementation and found that 400 IU per day hastened visual decline. “Due to competitive transport, vitamin E inhibits the uptake of vitamin A,” said Dr. Berson. “Anything that takes vitamin A away from an RP patient appears adverse; once rods die, cones become vitamin A deficient. We are treating an imbalance between rods and cones, not a gene.”
Something fishy? In a second trial in the late 1990s, 221 patients were randomized to either 1,200 mg of DHA per day or placebo capsules; all received vitamin A as well. Overall, no benefit was observed. However, a subgroup analysis among the control plus vitamin A group revealed that those who obtained 200 mg per day of DHA by eating oily fish (i.e., one or two 3-ounce servings of salmon or tuna each week) had a 40 to 50 percent slower loss of central visual field sensitivity than those eating less.
What’s the connection? From the rods, four molecules of vitamin A hitch a ride along with one molecule of DHA to the cones via inter-photoreceptor retinoid-binding protein (IRBP), said Dr. Berson. “If there’s no DHA in this ‘delivery vehicle,’ the A is not released, and the cones become vitamin A deficient.” It is not known whether oily fish contain other ingredients beneficial to cones of RP patients receiving vitamin A, he said.
Third trial adds lutein. Completed in 2008, the third trial evaluated the addition of a 12-mg lutein supplement in patients already taking vitamin A. Although it did not preserve central field sensitivity, it slowed midperipheral field loss by an estimated 10 years.
The combined analysis. Combining these three trials—which increased the sample size—a post hoc analysis published in 2012 showed that patients who took vitamin A along with a diet high in omega-3 oily fish had a 40 percent slower mean annual rate of decline in distance visual acuity than those with a diet low in omega-3 oily fish.6
Dr. Berson estimates that the combination of vitamin A, oily fish, and lutein could add up to 20 more years of vision for RP patients starting this regimen by age 40. Patients who would usually go blind at age 60 could retain useful vision to age 80. He added, “And with 25 years of data, we haven’t observed any toxic effects among adults on vitamin A 15,000 IU per day.”
Dry Eye: EFAs Show Benefits
“There’s a compelling and growing level of evidence that nutritional deficiencies are related to ocular surface disease and dry eye,” said John D. Sheppard, MD, at Eastern Virginia Medical School in Norfolk. The nutrients that have attracted the most attention in connection with dry eye syndrome are the omega-3 and omega-6 essential fatty acids (EFAs).
Over the last decade, many studies have explored the relationship between EFAs and dry eye syndrome.7 Benefits have been demonstrated in large retrospective observational studies of EFAs obtained through fish consumption8 as well as prospective randomized, multicenter clinical trials of supplements. A recent randomized double-masked trial showed statistically significant improvements in tear breakup time, Schirmer tests, and Ocular Surface Disease Index (OSDI) scores with 180 mg EPA and 120 mg DHA twice daily for 30 days.9
Determining the combinations. However, because these various studies have used several different types of EFAs—for example, from fish oil supplements, flaxseed and other plant sources, and dietary consumption of fish—the optimal combination remains unknown. Along with Steven C. Pflugfelder, MD, Dr. Sheppard is studying a proprietary supplement (HydroEye) that combines antioxidants and omega-3 fatty acids. In addition to DHA and EPA, it contains gamma-linolenic acid (GLA), which, he said, can be more difficult to obtain from the diet.
Success in a targeted group. Dr. Sheppard said they found “powerful results” in mitigating dry eye among postmenopausal women who were relatively nutritionally deficient.10
“We achieved statistically significant results in four different categories, including ocular surface inflammatory markers and improvement of the eye’s surface topographic regularity,” he said. “We also met the holy grail standard of the pharmaceutical industry by showing that symptoms improved significantly,” as assessed by the OSDI.
Cataract: Mixed Results
Thus far, the picture of nutrition’s role in cataract prevention remains cloudy.
AREDS. In a separate analysis, the AREDS1 formulation was not found to reduce the risk of progression to cataract surgery; and, for the most part, the same held true with AREDS2, said Dr. Chew. However, just as with AMD, a subset of participants low in dietary L/Z gained some protection. “This was a secondary outcome that needs further evaluation,” she added.
Antioxidants? Present. Lutein and zeaxanthin are present in the lens, as they are in the retina, where benefit accrues to both AMD and RP patients, said Dr. Johnson. Antioxidant vitamins C and E are also found in the lens, and their presence is the first step toward biological plausibility of a possible protective effect. In fact, a few studies have shown that vitamin C and E supplement users have achieved some benefit with regard to cataract, she said.
Multivitamins. In a large Italian trial, an over-the-counter multivitamin/multimineral supplement benefited those with nuclear sclerotic cataracts but increased the risk for posterior subcapsular cataract, said Dr. Chew.11
A low priority? Cataract also raises a question of priorities, added Dr. Sheppard. “Why are people going to make gargantuan efforts with nutrition to prevent a readily treatable disease, where it’s possible to markedly improve their quality of life with safe and highly effective surgery?”
Glaucoma: Dietary Links
Several solid articles have shown that reducing oxidative stress benefits glaucoma, said Dr. Reader. For example, among 584 older African-American women in the Study of Osteoporotic Fractures, those who consumed more fruits and vegetables high in vitamins A and C and carotenoids were less likely to have glaucoma.12 The study’s authors theorize that one or more mechanisms may be at work involving the trabecular meshwork, individual retinal ganglion cells, or vascular system nourishing the optic nerve.
Ginkgo biloba has also been found to be effective for glaucoma in some studies, said Dr. Sheppard, but these have not been multicenter, prospective, randomized trials. “The clinical data on Ginkgo biloba is Level III U.S. Preventive Services Task Force: based upon the opinions of respected authorities, on clinical experience, descriptive studies, or reports of expert committees.”
Seeing the Big Picture
Given multiple competing demands, what is the ophthalmologist’s role with regard to nutrition? “We should remember that we’re physicians first and subspecialists second,” said Dr. Reader. “At the very least, discuss nutrition and other lifestyle changes with patients who have early degenerative eye diseases.”
The ophthalmologist should also stay alert to specific vitamin deficiencies or toxicities, making appropriate referrals as needed, he said. For example, patients who’ve had bariatric surgery are at greater risk for problems with vitamin A absorption and may ultimately need to be seen by a gastroenterologist.
Collateral advantage. By addressing one organ system with nutrition, we may promote better function elsewhere as well, said Dr. Sheppard. “By taking fish oil for the eye, for example, the patient’s skin, joints, and serum cholesterol may improve. Or with zinc for macular degeneration, acne and muscle cramping may improve.”
It’s virtually the same recipe, added Dr. Johnson. “What benefits the eye and brain benefits the heart, as well. When you take a deep-down look at what’s going on with those blood vessels in macular degeneration, it looks the same as what’s happening with the heart’s vessels.”
Food first. Researchers have come to appreciate the diversity and synergy of nutrients found in food—a point to underscore with patients. “There are thousands of phytochemicals in vegetables and fruits,” said Dr. Johnson, “and we may never know what they all are and what they all do. The more diverse your diet, the better, because there is no one perfect food. So it’s not just your apple a day, but also your bananas, cherries, oranges, and so on.”
Studies have also begun to reveal how synergistically these nutrients work. “With AREDS1, the antioxidants alone didn’t do much until the mineral zinc was added,” said Dr. Johnson. “Likewise, you need vitamin C to regenerate vitamin E, and the omega-3s work together with the lutein.”
Genetic connections. Researchers are also beginning to understand what foods do molecularly as well as how they can turn genes on and off. “There are genes involved in carotenoid metabolism or absorption, for example, and in the elongation of omega-3 fatty acids,” said Dr. Johnson. “This helps explain why there is so much variability in terms of people’s responses to nutritional interventions.”
When supplements make sense. In general, people who eat a healthy diet with lots of fresh vegetables and fruits, and minimal sugar, salt, and meat don’t need heavy supplements, said Dr. Reader. “But only about 1 in 10 Americans eat this way. For everyone else, a natural vitamin/mineral supplement is probably worthwhile.”
It’s also a reasonable strategy to suggest supplements for those with beginning eye disease, said Dr. Hammond. With AMD, for example, you can achieve what amounts to a pharmaceutical effect, going right to the target tissue. Improving visual function in this way is a great achievement, he said, but it’s the wrong overall direction—trying to reverse a poor lifestyle that’s lasted 60 years or longer.
“I don’t have anything against modern biochemistry,” said Dr. Hammond, “but it’s a better strategy to rely on food. We’re trying to fool Mother Nature, and she’s had many millions of years to get it right.”
__________________________
1 Hammond BR Jr., Fletcher LM. Am J Clin Nutr. 2012;96(5):1207S-1213S.
2 Gruber M et al. J Nutr. 2004;134(9):2387-2394.
3 Age-Related Eye Disease Study Research Group. Arch Ophthalmol. 2001;119(10):1417-1436.
4 Age-Related Eye Disease Study 2 Research Group. JAMA. 2013;309(19):2005-2015.
5 Christen WG et al. Arch Intern Med. 2009;169(4):335-341.
6 Berson EL et al. Arch Ophthalmol. 2012;130(6):707-711.
7 Rand AL, Asbell PA. Curr Opin Ophthalmol. 2011;22(4):279-282.
8 Miljanovic B et al. Am J Clin Nutr. 2005;82(4):887-893.
9 Kangari H et al. Ophthalmology. 2013 May 3. [Epub ahead of print]
10 Sheppard JD et al. Invest Ophthalmol Vis Sci. 2012;53;E-Abstract 581.
11 Clinical Trial of Nutritional Supplements and Age-Related Cataract Study Group. Ophthalmology. 2008;115(4):599-607.
12 Giaconi JA. Am J Ophthalmol. 2012;154(4):635-644.
Meet the Experts
ELIOT L. BERSON, MD Professor of ophthalmology at Harvard Medical School and director of the Berman-Gund Laboratory for the Study of Retinal Degenerations at the Massachusetts Eye and Ear Infirmary, Boston. Financial disclosure: None.
EMILY Y. CHEW, MD Study chair of AREDS2 and deputy director of the Division of Epidemiology and Clinical Applications at the National Eye Institute, Bethesda, Md. Financial disclosure: None.
BILLY R. HAMMOND JR., PHD Professor of neuroscience and researcher in the Vision Sciences Laboratory at the University of Georgia, Athens. Financial disclosure: Has received funding from Abbott Nutrition, DSM, and the National Science Foundation.
ELIZABETH J. JOHNSON, PHD Nutritionist in the Human Nutrition Research Center on Aging (HNR-CA) at Tufts University, Boston. Financial disclosure: Is a consultant for Bausch + Lomb.
AUGUST L. READER III, MD Clinical professor of ophthalmology, California Pacific Medical Center, San Francisco. Financial disclosure: None.
JOHN D. SHEPPARD, MD Clinical director of the Lee Center for Ocular Pharmacology at Eastern Virginia Medical School, Norfolk, Va. Financial disclosure: Is a consultant for Alcon, Allergan, Abbvie, Bausch + Lomb, EyeGate, Gerson Lehman, Lux Biosciences, Santen, SarCode, Vistakon, and 1-800-doctors and is on the scientific advisory board for ScienceBased Health (manufacturer of HydroEye).
|