Download PDF
Currently, treatment for amblyopia is based on the following assumptions: Amblyopia is a primary disorder of monocular vision; patching is the right approach; and it responds to therapy only in children, the younger the better. But recent research has upended these assumptions.
A growing body of evidence shows that patients with amblyopia have a structurally intact binocular visual system that is rendered functionally monocular by suppression. The primary problem, in other words, is that the two eyes stop working together—usually due to strabismus or anisometropia—with the secondary consequence being amblyopia.1 “Function is not lost; it’s only suppressed,” emphasized Robert F. Hess, PhD, at McGill University in Montreal.
In the clinic, this new understanding means addressing the loss of binocular function as a first step in treatment, with the expectation that function of the amblyopic eye will improve as a result of reduced suppression from the fellow eye.
Current Approach
Approximately 3 to 5 percent of children and 3 percent of adults are affected by amblyopia. The disorder is conventionally viewed as a monocular visual acuity deficit resulting from discordant monocular images—and that because of early deprivation, part of the visual system doesn’t develop.
Amblyopia treatment typically consists of refractive correction followed by part-time patching or atropine penalization of the fellow eye to promote use of the amblyopic eye. Six months to two years of patching results in improved function in a majority of cases. When the patch is removed, however, the two eyes often don’t work together as they should. “Trying to implement a recovery under one-eye viewing, hoping it will help binocular vision, isn’t logical,” Dr. Hess said. Stereopsis typically remains elusive, and the fellow eye may continue to suppress the amblyopic eye, eventually leading to some reduction in acuity.
In children who were patched between the ages of 3 and 7, residual amblyopia of 20/32 or worse is still present in 54 percent of children at age 10 and 40 percent at age 15.2 The effectiveness of penalization falls precipitously—and residual amblyopia outcomes sharply increase—with age at treatment initiation, according to studies by the Pediatric Eye Disease Investigator Group (PEDIG).3 What’s more, patching can be traumatic for some children, making compliance highly variable.4
|
Web Extra: Clinical Update
|
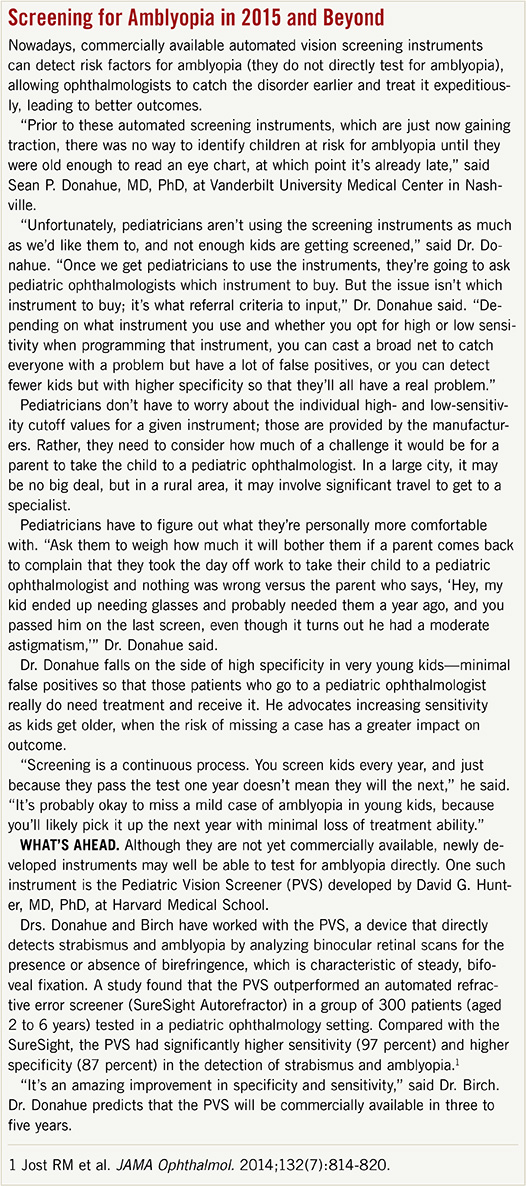 |
Shifting the Emphasis
Everyone with amblyopia has some degree of suppression, in which the better-seeing eye inhibits function of the misaligned or out-of-focus eye to avoid double or blurred vision. Dr. Hess’ team developed a method for measuring that suppression, demonstrating a direct relationship between degree of suppression and amblyopia. Combined with the basic science findings from Dr. Hess’ lab in 2008, which showed early evidence of residual binocular function in adults, this research pointed to a new treatment pathway.
Improving binocularity. In 2008, Eileen E. Birch, PhD, MPH, at the Retina Foundation of the Southwest in Dallas, was doing work in children showing that all the monocular deficits associated with amblyopia were linked to binocular deficits. “Along with Dr. Hess’ work in adults and some physiological research in monkey models that showed some retention of binocular function, we had all the basic pieces,” said Dr. Birch. “By 2010, we had put them all together.”
Researchers began work on treatments that focus on improving binocularity, using methods of perceptual learning training through iPad- or iPod-based video games that force the player to use both eyes. Though still in its infancy, this approach has yielded promising outcomes for amblyopia, leading PEDIG to launch a six-month multicenter trial to test it.
“When we first presented our perspective in 2012 and 2013, it was met with astonishment and disbelief,” said Dr. Birch, “but at the Academy’s 2014 meeting, it felt like people were more accepting of a shift in thinking.”
Visual acuity overemphasized? According to Drs. Hess and Birch, the treatment of amblyopia has focused too much on visual acuity, when it’s binocularity that’s central to a full functional recovery without regression. This doesn’t mean the end of patching altogether, Dr. Birch said. Some kids need an alternative or additional treatment, and a dual approach could meet that need.
“You don’t have to have normal vision in both eyes to train the two eyes to work together,” Dr. Hess said, “and having them work together confers huge benefits in terms of 3-D vision, extent of visual field, etc.” The benefit of binocular vision outweighs the benefit of improved visual acuity in the amblyopic eye, Dr. Hess contends, although visual acuity in the amblyopic eye did improve equally or more with his binocular approach, compared with patching.
|
Web Extra: Clinical Update
|
 |
Therapy Options Expand
Video games. With binocularity as a goal, new therapies are based on dichoptic presentation of the elements of several video games. Dr. Hess’ team used a modified version of Tetris (although an array of simple games amenable to dichoptic presentation are now being used) to set up artificial viewing conditions to reduce the signal strength coming through the subject’s good eye so that it couldn’t suppress the amblyopic eye. The more time the eyes worked together combining information, the stronger the subjects’ binocular capacity became. The viewing conditions could slowly be moved over the course of four weeks in the direction of more normal viewing, where both eyes saw the same images.1
In Dr. Hess’ lab, treatment has been administered to adults on an iPod device equipped with a lenticular screen. For children, Dr. Birch’s team adapted treatment to age-appropriate games administered on an iPad.
Surprising results in adults. The McGill team found that the binocular training in adults had to be done for only one to two hours a day, for four to six weeks, after which the two eyes could work together under natural viewing conditions. “This has been the holy grail of treatment, and it was relatively easy to achieve,” said Dr. Hess. The team also showed improvements in 3-D vision, with some patients experiencing stereopsis for the first time—something experts didn’t think was possible. As a result of eliminating suppression from the fellow eye, the acuity of the amblyopic eye also improved, and there was no regression. These results were obtained in adults, some of whom were middle aged. Previously, there had been no effective treatment for adults.1 A related “app” is being developed by Amblyotech.
Confirmation in children. “Our four- to eight-week proof-of-concept studies in children found that one hour daily of iPad treatment adapted from Dr. Hess’ lab achieved the same benefit as patching,” said Dr. Birch. Two-thirds of the children had prior patching, which might have limited their response to the iPad.5 “One problem with the iPad is that you can’t do anything else at the same time, and that made some of our children noncompliant,” said Dr. Birch.
Practical Benefits
The benefits of binocular therapy regarding stereopsis in children are important to note. Besides the joy of achieving 3-D vision, patients reap practical rewards. A number of studies in children with strabismus have found that the risk for recurring amblyopia is lower when stereopsis is recovered. Children are less likely to have a recurrence of strabismus (and therefore less likely to need a second surgery), and they’re less likely to develop anisometropia with consequent need to wear glasses. “The whole process is easier if children develop 3-D vision early in the course of treatment,” said Dr. Birch.
What’s more, research has revealed many minor motor skill deficits (such as problems with gait or catching balls) in people with binocular deficits, and all those minor impairments can add up.6 Dr. Birch has just started a study of eye movement control related to binocular deficits and how it might affect reading skills in children. It appears that amblyopic children may have instability in their eye movements that can slow their reading speed, with implications for test results as well as lifelong learning.
___________________________
1 Hess RF et al. Restor Neurol Neurosci. 2010;28(6):793-802.
2 Repka MX et al. JAMA Ophthalmol. 2014;132(7):799-805.
3 Repka MX et al. J AAPOS. 2009;13(3):258-263.
4 Felius J et al. J AAPOS. 2010;14(5):389-395.
5 Birch EE et al. Abstract 10. Presented at: American Association for Pediatric Ophthalmology and Strabismus; April 3, 2014; Palm Springs, Calif.
6 Grant S, Moseley MJ. Strabismus. 2011;19(3):119-128.
___________________________
Eileen E. Birch, PhD, is director of Crystal Charity Ball Pediatric Eye Research Laboratory at the Retina Foundation of the Southwest in Dallas, and adjunct professor of ophthalmology at the University of Texas Southwestern Medical Center. Financial disclosure: None. Sean P. Donahue, MD, PhD, is chief of pediatric ophthalmology at Vanderbilt Children’s Hospital in Nashville and professor of ophthalmology, neurology, and pediatrics at Vanderbilt University Medical Center. Financial disclosure: Has been a consultant for GoBiquity, WelchAllyn, PediaVision, and PlusOptix. Robert F. Hess, PhD, DSc, is director of the McGill Vision Research Unit and professor of ophthalmology at McGill University in Montreal. Financial disclosure: McGill University has U.S. patents on which Dr. Hess is a named inventor; the patents have been licensed to Amblyotech.