Download PDF
Same-day transplantation of tiny pieces of autologous limbal stem cell tissue onto a patient’s burned cornea can restore the ocular surface long term, without requiring expensive ex vivo cultivation of a larger limbal epithelial sheet before the transplant,a large case series has found.
This simple limbal epithelial transplantation (SLET) procedure repaired the corneal epithelium and maintained it for at least 1 year in 76% of 125 study eyes, the researchers at the L.V. Prasad Eye Institute, in Hyderabad, India, reported.1 That was comparable to the group’s previously reported success rate of 71.4% with cultivated limbal epithelial transplantation (CLET).2 Success was defined as a completely epithelialized, clinically stable, and avascular corneal surface.
This technique was particularly advantageous in children, who had a success rate of 71% with SLET vs. 37% with CLET, said study coauthor Virender S. Sangwan, MBBS, MS. “SLET works superbly well in the pediatric population,” said Dr. Sangwan, who is the Dr. Paul Dubord Chair in Cornea and director of the Center for Ocular Regeneration at the L.V. Prasad Institute.
Visual outcomes. Patients in the study had unilateral chemical or thermal ocular surface burns. Prior to surgery, 93.3% of the children (n = 60) and 92.3% of the adults (n = 65) had best-corrected visual acuity (BCVA) of 20/200 or worse. After surgery and a median follow-up of 1.5 years:
- In the eyes in which SLET was successful (n = 95), 67% improved to BCVA of 20/60 or better (p < .0001). The continued poor acuity in the other eyes was due to dense amblyopia, stromal scarring, or cataract.
- BCVA of 20/200 or worse fell to 38% for children and 30% for adults.
- Risk factors associated with transplant failure were history of acid burns; presence of symblepharon extending onto the cornea; concurrent keratoplasty; and postoperative loss of the transplanted tissue.
Technique for transplant. As described by the authors, autologous SLET requires a limbal biopsy sample, measuring 1 clock-hour, from the patient’s uninjured fellow eye. The tissue is divided into 6 to 8 pieces, which are laid onto an amniotic membrane scaffold atop the bared cornea and then secured with fibrin glue and a bandage contact lens.
The tiny limbal tissue fragments can regenerate the entire corneal surface, eliminating the expensive and technology-dependent practice of expanding the biopsy sample in the laboratory before transplantation, the authors wrote. Further, this method requires harvesting substantially less tissue from the fellow eye than either CLET or standard autologous limbal stem cell grafting.
“It seems that the conventional assumption of needing 3 to 6 clock-hours of donor tissue based on animal studies may not necessarily hold true in humans,” they wrote. “It does not seem to matter whether a 1-clock-hour limbal biopsy sample is cultured ex vivo on a Petri dish with laboratory reagents or in vivo on the corneal surface itself.”
Wider adoption encouraged. Dr. Sangwan’s group and others previously have reported positive outcomes with SLET,3-6 fueling early adoption of the procedure. “My colleagues and I have trained groups from Southeast Asia, Africa, North America, Brazil, Mexico, and many other countries,” he said.
Now, because of its larger population and longer follow-up, this study validates the earlier research and supports wider adoption of the technique, Dr. Sangwan said.
“Based on accumulated personal experience and published literature, I am more than 100% confident in recommending SLET for patients anywhere in the world,” Dr. Sangwan said. “Surgeons need minimal training for this surgery, and they can expect results as good as in my hands.”
—Linda Roach
___________________________
1 Basu S et al. Ophthalmology. 2016;123(5):1000-1010.
2 Sangwan VS et al. Br J Ophthalmol. 2011;95(11):1525-1529.
3 Sejpal K et al. JAMA Ophthalmol. 2013;131(6):731-736.
4 Vazirani J et al. Br J Ophthalmol. Published online Jan. 27, 2016. doi:10.1136/bjophthalmol-2015-307348.
5 Amescua G et al. Am J Ophthalmol. 2014;158(3):469-475.e2.
6 Mittal V et al. Cornea. 2015;34(10):1227-1232.
___________________________
Relevant financial disclosures—Dr. Sangwan: None.
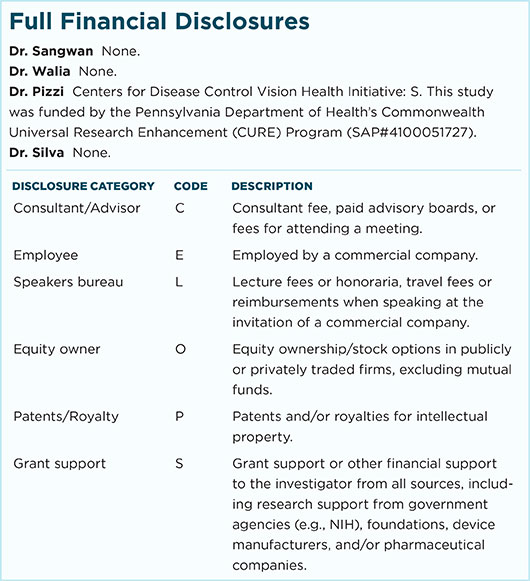
For full disclosures and disclosure key, see below.
More from this month’s News in Review