By Gabrielle Weiner, Contributing Writer, interviewing Deborah S. Jacobs, MD, Shahzad I. Mian, MD, and Sanjay V. Patel, MM
Download PDF
While awareness of the potential benefits of scleral lenses—large-diameter rigid gas-permeable lenses—has steadily increased over the past decade, it still lags among ophthalmologists.
Although fitting contact lenses is typically managed by optometrists, it is important for ophthalmologists to understand the potential role for scleral lenses, particularly in corneal ectasia and ocular surface disease, noted Sanjay V. Patel, MD, at the Mayo Clinic in Rochester, Minnesota.
Scleral Lenses 101
Designed to vault over the entire corneal surface and rest on the sclera, scleral lenses can morph an irregular cornea into a smooth optical surface to correct vision problems caused by keratoconus and other forms of corneal ectasia. Furthermore, the space between the cornea and the back of the scleral lens acts as a fluid reservoir, continuously bathing the cornea. This can provide relief for people with severe ocular surface disease and may help the ocular surface to heal.
Indications. The primary indications for scleral lenses are corneal irregularity, ocular surface disease, and severe refractive error.
At the Kellogg Eye Center in Ann Arbor, Michigan, Shahzad I. Mian, MD, has been using scleral lenses for 16 years. “Scleral lenses have transformed the management of both corneal ectasia and ocular surface disease,” he said. “They’ve helped reduce the need for surgical intervention and significantly improved the quality of life for so many patients, especially those with severe ocular surface disease [e.g., Stevens-Johnson syndrome, graft-versus-host disease, neurotrophic keratitis, exposure keratitis, and neuropathic pain] who have symptoms [that are] refractory to other therapies.”
When Dr. Mian first started prescribing scleral lenses, it was only for dry eye disease. That is still a common indication, but he is more likely to use them nowadays for corneal ectasia—both the ectasia seen with keratoconus and that which occurs following refractive surgery—and refractive error from irregular corneal shapes, including that occuring after corneal transplantation or linked to scarring.
Advantages. The main benefit of scleral lenses is that they can be designed to accommodate any degree of corneal steepness or irregularity, said Deborah S. Jacobs, MD, at Massachusetts Eye and Ear and Harvard Medical School in Boston. They provide better centration and stability than corneal lenses, and they are more comfortable because the conjunctival tissue on which scleral lenses rest is less sensitive than corneal tissue.
Furthermore, in patients who have experienced damage to corneal tissue, scleral lenses do not touch the cornea but rather bathe it continuously in preservative-free saline so that scar formation is not exacerbated.1
Drawbacks. Availability of scleral lenses has improved over the last decade, but other obstacles remain, namely cost and convenience.
Time. The optometrist who is fitting the lens requires special training, and the fitting process is time consuming, requiring several visits.
Cost. The fitting process is reflected in the cost, which ranges broadly from $500 per lens plus a fitting fee to an all-inclusive fee of several thousand per eye, depending on the type of lens and the fitting process (see below). This is not covered by many health insurance plans, though some vision care plans may cover it all or in part, Dr. Jacobs noted.
Convenience. “Other limiting factors are debris collection in the reservoir, fogging, and fouling of the front surface of the lens,” Dr. Jacobs said. In addition, Dr. Patel pointed out, “Patients may need to pop them out in the middle of the day to give them a scrub, then pop them back in. It can be inconvenient for some patients.”
 |
|
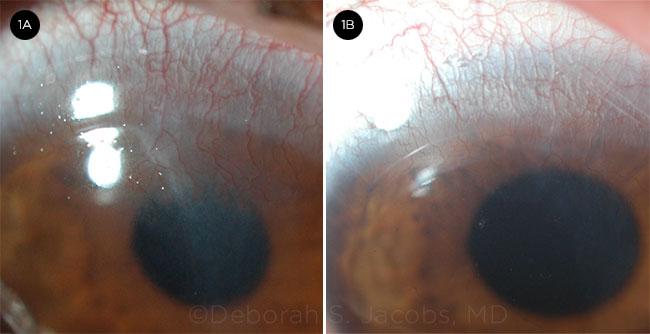
IMPROVEMENT. This 10-year-old was diagnosed with Stevens-Johnson syndrome at age 5. (1A) Six months after being switched from extended-wear soft contacts to PROSE treatment. (1B) At the 24-month mark after being switched to PROSE, the eye is quiet and regression of pannus is evident.
|
Which Lens Is Best?
At Kellogg Eye Center, Dr. Mian and his colleagues have fitted many hundreds of patients with sclerals. Initially, they used only PROSE (Prosthetic Replacement of the Ocular Surface Ecosystem) and sent patients to Boston, where PROSE was developed by BostonSight in the early 1990s. About 10 years ago, Kellogg became one of the early satellite clinics for PROSE treatment.
Since then, “there has been an explosion of different types of scleral lenses, and our contact lens specialists fit both PROSE and commercially available lenses,” Dr. Mian said. “Often PROSE is still the preferred lens for the most severe patients, particularly the severe dry eye patients. That said, many patients can be fit successfully with the other types of sclerals,” he added.
PROSE. “PROSE is really a treatment approach more than a piece of plastic. Yes, it produces a large-diameter gas-permeable lens that the patient wears on a daily basis, but the endpoint of the whole design, fit, and customization [process] is prosthetic function, and that involves an assessment, then customization, then monitoring,” explained Dr. Jacobs, formerly with BostonSight.
Fitting and customization. “The capability of the fitter in customizing the design and shape of the lens is different for PROSE than it is for the commercial lenses, for which there are just a few parameters the fitter can adjust and then communicate to the lab that makes the lens,” Dr. Jacobs said. In contrast, in PROSE, fitters use a computer-assisted design system that enables them to manipulate directly each prosthetic device to the patient’s precise and unique eye shape.
“The academic centers that became PROSE satellites brought on an optometrist who typically had specialized in cornea and contact lens in a ‘residency’ year following optometry school. In that year, optometrists learn to fit specialty lenses and get comfortable with a broader spectrum of corneal disease,” said Dr. Jacobs.
Delivery and cost. PROSE is delivered through a medical model, with a single fee per eye set by the institution with all services related to treatment wrapped in, Dr. Jacobs said.
The approximate cost for PROSE, which is sometimes referred to as the Rolls Royce of scleral lenses, is on the order of $5,000-$7,000 per eye for the entire process.
Commercially available scleral lenses. At Mayo, Dr. Patel and his colleagues popularized fitting lenses from a diagnostic set. “It is cheaper for the patients, and most eyes—not all—can be fit that way,” he said.
Fitting and customization. As with PROSE, the goals of fitting are that the lens is completely supported by the sclera, achieves complete clearance over the cornea and limbus, and achieves an even bearing zone on the sclera to avoid compression of blood vessels. The fitter uses the diagnostic set of trial lenses to determine the correct sagittal depth and then does overrefraction to obtain lens power. The back surface peripheral curve system can be modified to provide the best fit.
Although commercially available sclerals can’t offer complete customization, like that offered with PROSE, they meet the needs of most patients at a lower but variable cost.
Delivery and cost. Scleral lenses are sold through a optometric model: The lab sells them to the optometrist who fits the lenses. In turn, the optometrist sells them to the patient. Thus, it is up to the optometrist to determine what to charge for the lens and what the fitting fees are.
In the United States, the estimated average overall cost per eye (the lens plus the fitting) runs from $1,000-$5,000, depending on the complexity of the condition and the technology required.
Another option: Scleral variations. Modified, smaller rigid gas-permeable lenses are separated by size into miniscleral, semiscleral (also called intralimbal), or corneoscleral types. Respectively, their edges rest slightly outside the limbus, slightly inside it, or partly on the cornea and partly on the sclera.
These smaller lenses are not true scleral lenses and may only be used for corneal irregularity, not for ocular surface disease. Definitions and terminology are still evolving, but Dr. Jacobs defines true scleral lenses as having a diameter greater than 18 mm. In contrast, the diameters of the lenses mentioned above range from 13-17 mm.
Updated Treatment Algorithms
New paradigm for keratoconus. It used to be that treatment of keratoconus consisted of glasses or soft lenses for mild stages, rigid gas-permeable corneal contact lenses for moderate stages, and corneal transplantation for severe cases. The indication for surgery was contact lens failure.
But the advent of specialty lenses, including custom soft lenses, better hybrid lenses, and now scleral lenses and PROSE treatment, has extended the limit of what can be accomplished with contact lenses. “A case [of keratoconus] is not a ‘contact lens failure’ without a trial of specialty lens,” Dr. Jacobs emphasized.
“Many patients who would have come to surgery a decade or 2 ago can retain good vision for life with specialty lenses and particularly scleral lenses,” said Dr. Jacobs. “The surgeons who have access to scleral lenses for their patients report anecdotally that their rate of corneal transplant for ectasia and astigmatism has gone way down.” Indeed, Drs. Patel and Mian confirmed a significant reduction in surgery rates in their practices. And in a Belgian study published earlier this year, 40 of the 51 eyes with severe keratoconus that would have undergone transplant surgery were successfully treated with long-term scleral lens wear, reducing the indication for keratoplasty by more than half.1
Management of ocular surface disease. Scleral lenses are usually used later in the disease course. One exception, according to Dr. Mian, is patients with severe ocular surface disease associated with graft-versus-host disease. “Those patients often progress quickly to the very severe stage and typically don’t respond to other therapies, so we will move to scleral lenses faster.”
In all cases, over-the-counter lubricants are started immediately, then topical medication (e.g., cyclosporine or a topical steroid) and punctal occlusion are considered. The next option may be serum tears. Dr. Mian then turns to PROSE treatment before considering amniotic membrane contact lenses like Prokera (Bio-Tissue). Tarsorrhaphy and conjunctival flap come after that.
Clinical Pearls
Especially in patients who have ocular surface disease, Dr. Patel urged ophthalmologists to think about a scleral lens as an alternative to tarsorrhaphy or jumping to amniotic membrane or keratoplasty. “Think of scleral lenses and seek them out,” he said.
Don’t count out the young—or the old. Dr. Mian reported that some of his youngest patients have greatly benefitted from scleral lenses. These children had severe dry eye or neurotrophic disease (from herpetic infection) and were unable to heal the surface of their eye on their own. “Despite multiple other treatments that hadn’t worked, scleral lenses made a big difference in improving the health of their eyes and maintaining vision in their eyes,” said Dr. Mian. “My youngest patient was 2 years old.”
With regard to the other end of the age spectrum, he added, “It’s also feasible to fit patients into their 80s or 90s, as long as they can take care of the lenses.”
Work with the optometrist. When scleral lenses are used for ocular surface disease, the comprehensive ophthalmologist or cornea specialist will need to collaborate on an ongoing basis with the optometrist, because the underlying disease that will need to be monitored for neovascularization or potential infection continues to exist, Dr. Patel said.
“Supplemental treatments are still needed, especially when the patient takes the lenses out. They’ll still use lubricants; they’ll often still use topical steroids; they might still use serum tears,” he said. For corneal ectasia, the optometrist can often handle the case alone, but the lines of communication should be kept open if a complication arises, Dr. Patel noted.
Observe your patients with their lenses on. Dr. Jacobs encouraged all ophthalmologists to have a look at their patients with their scleral lenses on so that they can gain an appreciation for fit and physiologic function. “In contemporary practice, where there is so much emphasis on volume, the standard is that the staff measures vision in lenses, then takes them out to proceed with the rest of the eye exam prior to the physician seeing the patient,” Dr. Jacobs said. “But even if not trained in fitting, the ophthalmologist can gain a better understanding of scleral lenses when examining the eyes with them on and then off.”
Lowering the Clinical Threshold
Because severe refractive error is an indication for scleral lenses, what’s stopping clinicians from using them for more typical refractive errors?
No added value. Soft lenses remain the primary way to correct refractive error because most patients can tolerate them, they’re easy to use, and there’s less maintenance. “Convenience is the No. 1 factor,” said Dr. Mian, “and sclerals are inconvenient. Using them solely for refractive error doesn’t add more value to the average patient and is far more expensive.”
Concerns over long-term use. In order to consider using scleral lenses for vision correction, not for disease, ophthalmologists need to know more about potential long-term side effects. Although the lenses sit on the sclera, they come very close to the limbus. “If scleral lenses damage the limbus, it can cause big problems long term. We have no clinical evidence of that happening, but we worry about it,” said Dr. Mian.
Possible exception: Athletes with astigmatism. One exception to physician reluctance to prescribe might be the use of minisclerals for serious athletes with astigmatism.
Take a professional baseball player, for example. “Soft lenses don’t correct sharply enough, glasses are a problem if you’re diving after a line drive, and corneal lenses move around and can get dirt and grit under them,” Dr. Jacobs said. “For serious baseball players with ordinary astigmatism, a miniscleral would be easy to fit and would correct them well.” To address concerns regarding long-term use, the athlete could wear the miniscleral lenses just for games and practices.
But can an athlete—or anyone else —wear minisclerals for 12-14 hours a day over many years? “The miniscleral world is working on answering that question,” Dr. Jacobs said.
___________________________
1 Koppen C et al. Am J Ophthalmol. 2018;185:43-47.
___________________________
Dr. Jacobs is associate professor of ophthalmology at Harvard Medical School. She is also faculty on the Cornea Service and director of the Ocular Surface Imaging Center at Massachusetts’ Eye and Ear in Boston. Relevant financial disclosures: BostonSight: E (through February 2018).
Dr. Mian is professor of ophthalmology and visual sciences, the Terry J. Bergstrom Collegiate Professor for Resident Education in Ophthalmology and Visual Sciences, and associate chair for education at the University of Michigan’s Kellogg Eye Center in Ann Arbor, Mich. Relevant financial disclosures: None.
Dr. Patel is professor and chair of ophthalmology at the Mayo Clinic in Rochester, Minn. Relevant financial disclosures: None.
For full disclosures and the disclosure key, see below.
Full Financial Disclosures
Dr. Jacobs BostonSight: E (through February 2018); Simple Contacts: C; TecLens: C.
Dr. Mian Shire: S; Visioncare: S.
Dr. Patel None.
Disclosure Category
|
Code
|
Description
|
| Consultant/Advisor |
C |
Consultant fee, paid advisory boards, or fees for attending a meeting. |
| Employee |
E |
Employed by a commercial company. |
| Speakers bureau |
L |
Lecture fees or honoraria, travel fees or reimbursements when speaking at the invitation of a commercial company. |
| Equity owner |
O |
Equity ownership/stock options in publicly or privately traded firms, excluding mutual funds. |
| Patents/Royalty |
P |
Patents and/or royalties for intellectual property. |
| Grant support |
S |
Grant support or other financial support to the investigator from all sources, including research support from government agencies (e.g., NIH), foundations, device manufacturers, and/or pharmaceutical companies. |
|