By Gary N. Holland, MD, with Debra A. Goldstein, MD, James T. Rosenbaum, MD, and Russell N. Van Gelder, MD, PhD
Download PDF
In the last 2 issues of EyeNet, Gary N. Holland, MD, of the UCLA Stein Eye Institute, hosted a roundtable discussion on laboratory testing for patients with uveitis. In this third and final installment of the uveitis series, Dr. Holland continues his conversation with Debra A. Goldstein, MD, of Northwestern University’s Feinberg School of Medicine; James T. Rosenbaum, MD, of Oregon Health & Science University’s Casey Eye Institute and the Legacy Devers Eye Institute; and Russell N. Van Gelder, MD, PhD, of the University of Washington. The experts share thoughts on evaluating uveitis at its first occurrence, emerging technologies for assessment, cost-benefit analyses, and other considerations.
Ordering Tests at First Occurrence
Dr. Holland: Some clinicians say that a patient’s first episode of nonspecific anterior uveitis doesn’t need to be evaluated. What are your thoughts on this concept?
Dr. Van Gelder: As tertiary uveitis specialists, we live in a bit of a different universe. Generally, we don’t see patients with mild acute anterior uveitis who walk into a comprehensive ophthalmologist’s office, are treated for the episode, and get better. We see a more select population. By the time a patient makes it to me, he or she will be evaluated if we don’t have a cause of disease at hand.
I don’t see a downside to testing patients on first presentation. You may be able to provide prognostic information if the human leukocyte antigen (HLA)-B27 result is positive. If a test result indicates systemic or treatable disease, such as syphilis or sarcoidosis, it is crucial for the patient to be aware of the diagnosis, and the treatment for uveitis may need to be modified.
I don’t think there are strong data regarding outcomes for patients who did or did not receive testing at the time of their first uveitic episode. Although those data would be helpful for assessing the cost of testing or not testing, I’d rather identify the rare case of a systemic or infectious disease at a patient’s first presentation than let the disease declare itself over time and potentially involve some morbidity.
Dr. Rosenbaum: I agree. In the community, approximately 80% to 85% of uveitis cases are anterior. If you have sudden-onset anterior uveitis and live in North America or Europe, your likelihood of HLA-B27 positivity is approximately 50%. According to the SENTINEL study,1 if you’re HLA-B27 positive and experience sudden-onset anterior uveitis, your chance of having spondyloarthropathy is 90%. In the SENTINEL study, patients were excluded for known spondyloarthropathy. Because many patients with spondyloarthropathy are undiagnosed, we have a huge opportunity to provide diagnostic information. Everyone deserves a careful history and clinical exam, and the results of a uveitis workup may indicate inflammatory bowel disease, Behçet disease, or Vogt-Koyanagi-Harada disease. I regard every episode of uveitis, including the first episode, as an opportunity to recognize associated conditions.
Dr. Goldstein: When I teach courses on uveitis, people always ask, “Do I need to work up the first case?” If a patient presents with nonsevere unilateral anterior uveitis that lacks fibrin or hypopyon, if the uveitis is nongranulomatous—because granulomatous uveitis increases the likelihood of systemic disease—and is associated with a completely negative review of systems, then you do not need to perform a workup for that patient. However, I have yet to see such a patient.
As tertiary referral physicians, we have a biased view, but why wait until a second episode to evaluate a patient for ankylosing spondylitis? Why wait if a patient has hypopyon uveitis, which we know means that he or she is statistically more likely to have unrecognized spondyloarthropathy?
Dr. Rosenbaum: When performing a review of systems, you have to know how to structure the questions appropriately. For example, back pain is ubiquitous, and many people have chronic back pain and simply assume it’s part of daily living. I’ll never forget one patient who was in my office with florid ankylosing spondylitis. He denied any back pain but couldn’t straighten up. A week after taking nonsteroidal anti-inflammatory drugs, he came back and said, “I am the Tin Man, and I just got oiled.”
Dr. Goldstein: I was called to see a patient by one of our retina fellows. The patient had a diagnosis of acute retinal necrosis but wasn’t responding to treatment. It was apparent to me that she likely had Behçet disease. I asked the fellow, “What about the review of systems?” He said, “The review of systems was completely negative.” Then I talked to the patient, and I asked about oral ulcers. She affirmed that she had frequent oral ulcers that were so severe she couldn’t go to work for 2 weeks at a time, would lose weight, and couldn’t brush her teeth. I asked the patient about skin lesions, and she described having pustular lesions on her scalp and erythema nodosum. When I asked about genital sores, she was offended, as if I had “outed” her as having severe herpes that didn’t respond to anything.
Clearly, she had Behçet disease, and when I asked the fellow about the negative review of systems, he said he had asked the patient if she was healthy. I had to explain that it is not sufficient to ask, “Are you healthy?” We actually have to review all relevant organ systems.
Dr. Rosenbaum: For something like a genital sore, which has a pejorative connotation, you have to ask that question in a reassuring and nonjudgmental manner. You might say something like, “Sometimes, recurrent sores in the genital area are not related to sexual activity and can be associated with uveitis. Have you experienced anything like that?”
Dr. Holland: I think we’re in agreement that tests should be ordered if indicated, regardless of whether it’s the first or the 21st uveitic episode.
Ordering Your Own Testing
Dr. Holland: When you see a patient and are considering a diagnosis, do you order laboratory tests yourself, or do you ask the patient’s primary care provider to order the tests?
Dr. Van Gelder: I think most, if not all, uveitis fellowship–trained specialists handle their own lab testing. There’s a danger in requesting that tests be ordered by the patient’s primary care provider or rheumatologist. The differential diagnosis and probabilities of potential causes for the uveitis would not necessarily be apparent to physicians who are not ophthalmologists. Having others order testing could be inappropriate or wasteful. I think it behooves ophthalmologists to order their own lab testing based on the history obtained and the exam they performed. If an ophthalmologist is in doubt, a quick phone call or an email to a uveitis specialist can provide some insight into appropriate tests for a particular presentation.
Dr. Holland: That’s an important point. I have seen patients referred by other ophthalmologists to a rheumatologist or to the patient’s primary care provider with a request simply to evaluate the patient for uveitis. The rheumatologist, not knowing anything about the patient’s manifestations, might order a lot of unnecessary testing.
However, I might advise a patient to return to the primary care provider or rheumatologist for a test if I knew that the patient would be undergoing other tests—just to save them from multiple blood draws. In that case, I would provide the other physician with specific recommendations for which tests to perform.
Dr. Goldstein: By not ordering our own testing, we can end up with patients who have undergone analyses of antinuclear antibody, rheumatoid factor, erythrocyte sedimentation rate, and Lyme serology that all were irrelevant to their disease. I order my own testing, and I recommend at least having a differential diagnosis and informing the rheumatologist of any tests you don’t want to be ordered. Say, “This is a patient with acute anterior uveitis, and I’m worried about ankylosing spondylitis,” or “This is a patient with granulomatous uveitis, and I’m worried about tuberculosis and sarcoid.” It’s not up to the rheumatologist to decide on a differential diagnosis without any exam findings.
Dr. Van Gelder: On the flip side, excellent communication with other specialists is essential when you do have a lab test or a diagnosis at hand. I may initiate lab testing for granulomatosis with polyangiitis (formerly Wegener’s granulomatosis). If I get positive results on a test for anti-myeloperoxidase and anti-proteinase 3, my next call would be to the rheumatologist to coordinate a full workup for other systemic manifestations and to discuss treatment options for the patient. We don’t work in a vacuum, but I do think that the ophthalmologist should order the initial testing for a uveitis presentation.
Cost-Benefit Considerations
Dr. Holland: As a department chair, Dr. Van Gelder, you have to consider cost-benefit analyses and authorizations for billing. In that context, what are your thoughts about the frequency and number of lab tests that ophthalmologists order?
Dr. Van Gelder: Several colleagues and I conducted a study of testing practices among members of the Executive Committee of the American Uveitis Society.2 There are no guidelines for testing patients with uveitis, and we found no consistency regarding how testing is performed for any given patient scenario. In this study, we calculated the costs of testing for 13 patient scenarios.
We found that radiologic tests and ophthalmic imaging are among the most expensive tests ordered, when you account for facility costs and professional fees. In fact, more than half of all costs were attributable to imaging. One magnetic resonance imaging (MRI) scan easily can cost several thousand dollars if you’re performing a workup for multiple sclerosis or intraocular lymphoma. Computed tomography scans of the chest for sarcoid can cost many hundreds of dollars. Fluorescein angiography has high associated facility costs when it is performed in a hospital setting, which includes many uveitis clinics. However, our serologic testing is relatively inexpensive. Testing for syphilis and the Quantiferon assay for tuberculosis cost $100 or less, each. I think very carefully before ordering imaging analyses, but I tend not to scrimp on serologic tests.
Nowadays, physicians belong to panels, and we are constantly being scrutinized for resource utilization. Uveitis specialists are at risk for being regarded as “high utilizers” or “high-cost providers” relative to other ophthalmologists. We order a lot of laboratory testing, and that can result in our exclusion from provider panels. It behooves our subspecialty to explain to insurance panels that uveitis specialists see a unique patient population. Treatment of these patients involves more testing than does treatment of patients in a standard ophthalmology practice.
Dr. Holland: Have any of you encountered problems obtaining authorization for laboratory tests or imaging studies?
Dr. Rosenbaum: Sometimes insurers will object to expensive studies, such as brain MRI.
Dr. Goldstein: I have encountered resistance to using imaging tests such as optical coherence tomography or angiography, but not to blood tests.
New Testing Modalities
Dr. Holland: What are some new developments for laboratory evaluation of uveitis?
Dr. Van Gelder: I think we’ll have some interesting new modalities in the near future. Dr. Holland, you’ve been a pioneer in the use of laser flare photometry. At least in the United States, I think that this is an underappreciated modality that can yield prognostic, and potentially diagnostic, information. I expect that laser flare photometry will become more accessible and more useful. The utility of anterior chamber paracentesis also is increasing.
There has been progress in understanding cytokine profiles, proteomics, and transcriptomics of the aqueous and vitreous for diagnosis of infectious diseases. Along with her colleagues, Dr. Thuy Doan demonstrated that she could distinguish infectious from noninfectious posterior uveitis with high reliability by examining the transcript profile of the vitreous.3 For many disease presentations, you can’t perform a clinical exam of the eye and determine with certainty whether the condition is infectious or noninfectious. I think that laboratory testing of ocular fluids will continue to develop and become more mainstream.
Dr. Rosenbaum: We’re still classifying about 35% of uveitis cases as idiopathic, at least in referral centers. This was confirmed in 2 high-profile randomized clinical trials involving a biologic drug.4,5 Gene expression profiling from peripheral blood may be a means to reduce the percentages of cases categorized as idiopathic. There may be patterns of gene expression that will help us recognize occult inflammatory bowel disease, spondyloarthritis, or tubulointerstitial nephritis with uveitis syndrome.
Dr. Holland: I agree. I think that immunogenetics research will contribute to better understanding of individual risk and disease mechanisms. Eventually, this approach may enable more personalized care for patients with uveitis—both in terms of diagnosis and treatment.
___________________________
Listen to the roundtable below:
___________________________
1 Juanola X et al. Ophthalmology. 2016;123(8):1632-1636.
2 Lee CS et al. Am J Ophthalmol. 2016;170:161-167.
3 Doan T et al. Genome Med. 2016;8(1):90.
4 Jaffe GJ et al. N Engl J Med. 2016;375:932-943.
5 Nguyen QD et al. Lancet. 2016;388(10050):1183-1192.
___________________________
Dr. Holland is Professor of Ophthalmology and Jack H. Skirball Chair in Ocular Inflammatory Diseases, David Geffen School of Medicine at University of California, Los Angeles, UCLA Stein Eye Institute. Relevant financial disclosures: None.
Dr. Goldstein is Magerstadt Professor of Ophthalmology at Northwestern University Feinberg School of Medicine in Chicago. Relevant financial disclosures: None.
Dr. Rosenbaum is Professor of Ophthalmology, Medicine, and Cell Biology; Head of the Division of Arthritis and Rheumatic Diseases; and Edward E Rosenbaum Professor of Inflammation Research at Oregon Health & Science University’s Casey Eye Institute in Portland. He is also the Richard Chenoweth Chair of Ophthalmology at Legacy Devers Eye Institute in Portland. Relevant financial disclosures: UpToDate: P.
Dr. Van Gelder is Boyd K. Bucey Professor and Chair of Ophthalmology at the University of Washington in Seattle. Relevant financial disclosures: None.
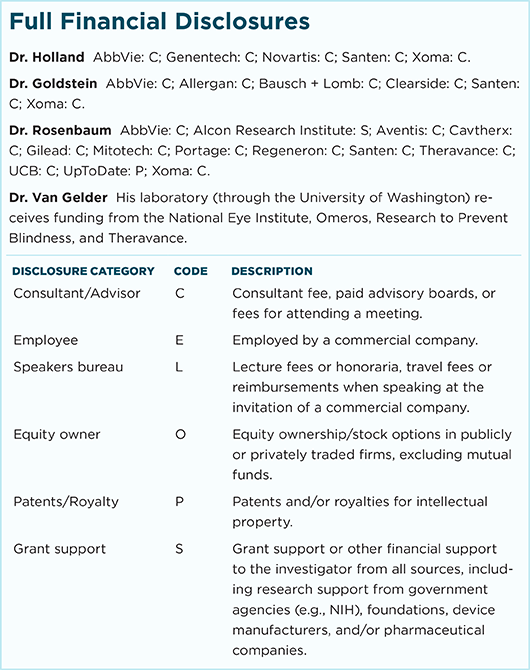
For full disclosures and the disclosure key, see below.