NOV 08, 2015
By Elias I. Traboulsi, MD
A Compendium of Inherited Disorders and the Eye, Oxford University Press
Genetics
Also includes AD simple ectopia lentis
OMIM Numbers
Inheritance
- Autosomal dominant with variable expression and high penetrance
Gene/Gene Map
- Fibrillin 1, a microfibrillar glycoprotein component of the extracellular matrix, is the defective gene product.
Epidemiology
- 1 in 3000 to 1 in 10,000 worldwide
- Paternal age effect for sporadic cases has been described
Clinical Findings
- The syndrome is characterized by abnormalities of the eye (ectopia lentis), aorta (dilation of the aortic root and aneurysm of the ascending aorta and aortic aneurysm), and skeleton (dolichostenomelia, upper segment/lower segment ratio 2 standard deviations below mean for age, pectus excavatum, and kyphoscoliosis).
- In addition to these 3 major criteria, auxiliary signs may be present, such as myopia, mitral valve prolapse, arachnodactyly, joint laxity, tall stature, pes planus, striae distensae, pneumothorax, and dural ectasia.
- About 35% of patients do not develop lens subluxation. There is a large family with Marfan without ectopia lentis in whom the disease gene was mapped to 3p24.2-p25.
- The clinical diagnosis may be difficult in mild cases, and the spectrum of patients with connective tissue abnormalities simulating Marfan is wide.
Ocular Findings
- Ocular abnormalities are present in at least 60% of patients. The most characteristic and usually diagnostic ocular abnormality is lens subluxation, which varies from mild superior and posterior displacement to significant subluxation with the equator of the lens in the pupillary axis (Figure 1). Inferior, nasal, or lateral subluxation also occurs. Subluxation is slowly progressive in some patients and most noticeable in the first few years of life or in the late teens and early twenties. Total dislocation into the vitreous cavity has been documented in older patients in whom it may rarely be complicated by phacolytic glaucoma. Lens dislocation into the pupil or anterior chamber is characteristic of untreated homocystinuria.
- Microspherophakia is present in about 15% of patients and results in high myopia. The cornea is flat with keratometric readings in the high 40s in about 20% of patients. Megalocornea (corneal diameter measuring more than 13.5 mm) may be present in some patients. The iris has a thin velvety texture, and the pupil is difficult to dilate in the more severely affected patients in whom there is atrophy of the dilator muscle fibers. Iridodonesis results from lens subluxation.
- Wheatley et al found fibrillin to be ubiquitous in the eye and a major component of the cornea, sclera, anterior chamber angle, uvea, zonules, lens capsule, and optic nerve septae. The authors concluded that ocular abnormalities could be correlated to the pattern of distribution of fibrillin in the eye. The normal lens capsule has 3 distinct and adjacent zones in the equatorial and peri-equatorial regions that contain fibrillin. Fibrillin fibers are abnormal and disrupted in all 3 zones in Marfan patients.
- Exotropia occurs in 10% of patients and esotropia in 2%. Strabismic and/or anisometropic or ametropic amblyopia should be suspected in all patients with reduced visual acuity.
- Open-angle glaucoma is significantly more common in Marfan patients in all age groups as compared to the general population and becomes more prevalent with increasing age. Pupillary block is unusual, but has been documented. Phacolytic glaucoma has been noted in older patients with mature dislocated lenses.
- Retinal detachment may occur spontaneously in eyes with axial myopia or following cataract extraction, especially in longer eyes. Loewenstein et al identified and retrospectively reviewed the charts of one cohort of 12 patients (15 eyes) with retinal detachment who were operated on at the Wilmer Institute and a second cohort of 16 such patients (24 eyes) who were operated on several years earlier and elsewhere. They concluded that the results of retinal detachment surgery in the past were worse when the eye was aphakic. In most cases operated more recently, the prognosis for successful repair was good regardless of whether the eye was phakic. In another study, Abboud found bilateral retinal detachment in 9 of 13 (69%) patients. The lens was ectopic in all eyes. Retinal breaks were small horseshoe tears or holes located anterior to the equator in 11 of 16 (69%) eyes. The retina of 12 of 16 (75%) eyes remained successfully reattached after a followup ranging from 4 to 132 months. All 12 eyes had a VA of 20/300 or better (range: 20/30 to 20/300); 8 had a VA of 20/125 or better, and the cause of failure in the remaining 4 eyes was proliferative vitreoretinopathy.
- Cataracts develop earlier than in the general population.
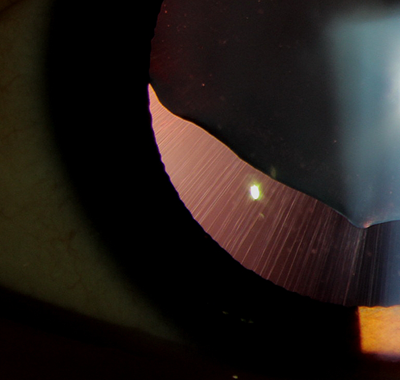
Figure 1. Subluxated lens in a patient with Marfan syndrome; note stretched zonules.
Therapeutic Aspects
- Periodic echocardiography should be performed to assess aortic dilation. Oral beta-blockers and Losartan reduce the incidence of aortic rupture. Aortic replacement may be necessary when aortic root measurements reach 50 to 55 mm in the adult. The average age of death has been delayed from the 40s to the 60s or later.
- Careful refractions at regular intervals are necessary to achieve best possible vision. The issue of the necessity of lensectomy in patients with significant subluxation and astigmatism continues to be debated. With the advent of vitrectomy instrumentation, small-incision lensectomy has become safer. Before lens extraction is contemplated, patients should have a prolonged trial of aphakic or phakic correction, as well as patching if amblyopia is suspected.
- The prognosis for vision is good if the diagnosis is made early, errors of refraction are corrected, and amblyopia is managed properly.
References
- Abboud EB: Retinal detachment surgery in Marfan's syndrome. Retina.1998;18:405-409.
- Izquierdo NJ, Traboulsi EI, Enger C, et al: Glaucoma in the Marfan syndrome. Trans Am Ophthalmol Soc. 1992; 90:111-117; discussion 118-122.
- Izquierdo NJ, Traboulsi EI, Enger C, et al: Strabismus in the Marfan syndrome. Am J Ophthalmol. 1994; 117:632-635.
- Loewenstein A, Barequet IS, De Juan E, et al: Retinal detachment in Marfan syndrome. Retina. 2000; 20:358-363.
- Maumenee IH: The eye in the Marfan syndrome. J Am Ophthalmol Soc. 1981; 79:684-733.
- Mir S, Wheatley HM, Hussels IE, et al: A comparative histologic study of the fibrillin microfibrillar system in the lens capsule of normal subjects and subjects with Marfan syndrome. Invest Ophthalmol Vis Sci. 1998; 39:84-93.
- Traboulsi EI, Whittum-Hudson JA, Mir SH, et al: Microfibril abnormalities of the lens capsule in patients with Marfan syndrome and ectopia lentis. Ophthalmic Genet. 2000; 21:9-15.
- Miraldi Utz, V, Coussa RG, Traboulsi EI. Surgical Management of Lens Subluxation in Marfan Syndrome: Application of a Simplified Technique and a Review of the Literature. JAAPOS. 2014; 18: 140-146.
- Wheatley HM, Traboulsi EI, Flowers BE, et al: Immunohistochemical localization of fibrillin in human ocular tissues: relevance to the Marfan syndrome. Arch Ophthalmol. 1995;113:103-109.
Resources
Traboulsi EI. Compendium of Inherited Disorders and the Eye. New York: Oxford University Press; 2005. Adapted with permission.