The key to any examination is to be systematic and always perform each element.
1. Visual acuity
- In the clinic, visual acuity is typically measured at distance. Otherwise, in a consult setting outside of the clinic, it’s measured at near. Don’t forget to have a near card with you.
- Make sure the patient is wearing his or her correction. Always have a pair of +3.00 readers with you, as many people in the emergency room won’t have their glasses with them. A pinhole occluder will also reduce the impact of uncorrected refractive error.
- If the patient is unable to see the biggest optotype on the card, the progression (from better to worse) is counting fingers (CF), hand motions (HM), light perception (LP) with projection, LP without projection and no light perception (NLP).
- For children who are too young to use Allen pictures, employ the “central, steady, maintain (CSM)” approach. Central: Is the corneal light reflex in the center of the pupil? Steady: Can the patient continue fixating when the light is slowly moved around? Maintain: Can the patient maintain fixation with the viewing eye when the previously covered eye is uncovered?
2. Pupils
- Look for anisocoria. If present, carefully check the pupil size in both well-lit and dark conditions.
- Check the reactivity of each pupil with a penlight or Finoff transilluminator.
- Use the swinging flashlight test to look for a relative afferent pupillary defect.
Cartoon:
https://www.youtube.com/watch?v=HSYo7LhfV3A
Patient:
https://www.youtube.com/watch?v=A6My6rI0p-A
3. Extraocular motility and alignment
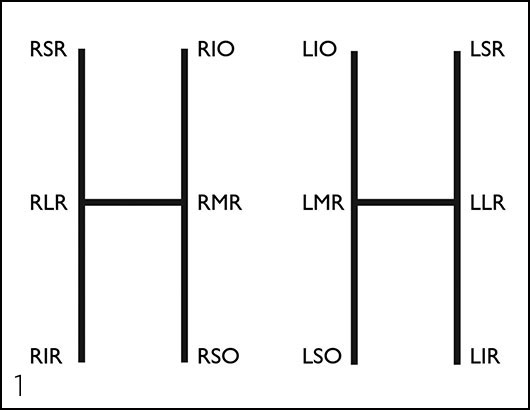
- Have the patient look in the six cardinal positions of gaze. Test with both eyes open to assess versions — repeat monocularly to test ductions. Figure 1 below shows which muscle is tested in each position.
- Use the cover/uncover test to assess for heterotropias.
- Use the alternate cover test to assess for the total amount of deviation. This amount minus any heterotropia is the amount of heterophoria.
4. Intraocular pressure
- Goldmann applanation tonometry is the gold standard and should be used in the clinic whenever possible.
- Outside of the clinic, Tono-Pen tonometry is much more practical.
- If you suspect a ruptured globe, skip this part of the exam.
5. Confrontation visual fields
- Assess each quadrant monocularly by having the patient count the number of fingers that you hold up. If acuity is particularly poor, have the patient note the presence of a light.
- Use the colored lid of an eyedrop bottle to define the position of a scotoma more accurately.
6. External examination
- Look for any ptosis by measuring the margin-to-reflex distance, which is the distance from the corneal light reflex to the margin of the upper lid.
- Look for lagophthalmos.
- Note any unusual growths or lesions that may require a biopsy.
- Palpate lymph nodes and the temporal artery if indicated by the history or exam.
- Measure proptosis or enophthalmos with an exophthalmometer.
- Perform a full cranial nerve exam for patients with diplopia or other neurologic symptoms.
7. Slit-lamp examination
- Lids/lashes/lacrimal system: Normal anatomy and contours? Any lesions?
- Conjunctiva/sclera: White and quiet? Injection? Lesions?
- Cornea: Clear? Epithelial disruptions? Stromal opacities? Endothelial lesions?
- Anterior chamber: Deep? Cell or flare?
- Iris: Round pupil? Transillumination defects? Nodules?
- Lens: Clear? Nuclear, cortical or subcapsular cataract?
- Anterior vitreous: Inflammation? Hemorrhage? Pigmented cells?
8. Fundoscopic examination
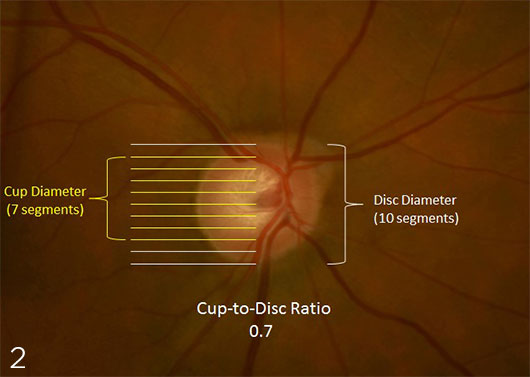
- Optic nerve: Cup-to-disc ratio (see Figure 2 below)? Focal thinning? Pallor? Symmetric?
- Macula: Foveal light reflex? Drusen, edema or exudates?
- Vessels: Contour and size? Intraretinal hemorrhage?
- Periphery: Tears or holes? Lesions? Pigmentary changes?
* * *
 About the author: Jason D. Rupp, MD, PhD, is a PGY-4 resident at Washington University/Barnes Jewish Hospital in St. Louis. He will be staying to complete a glaucoma and complex anterior segment surgery fellowship during the 2016–2017 academic year.
About the author: Jason D. Rupp, MD, PhD, is a PGY-4 resident at Washington University/Barnes Jewish Hospital in St. Louis. He will be staying to complete a glaucoma and complex anterior segment surgery fellowship during the 2016–2017 academic year.