Managing diabetic retinopathy (DR) is all about the labeling. If you learn the basic classification system early, it makes this multifaceted disease easier to manage — and helps your diabetic patients preserve their vision.
The landmark Early Treatment for Diabetic Retinopathy Study (ETDRS) in the 1980s established a series of disease stages that have structured subsequent studies. Learning these stages will inform every diabetic patient encounter that you’ll have.
It’s initially helpful to consider diabetic macular edema (DME) and DR as distinct, parallel disease processes. Both result from microvascular damage, but you treat them differently.
Diabetic Macular Edema
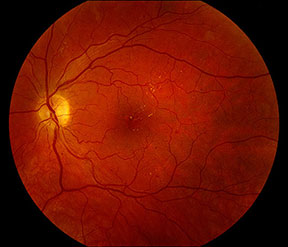
Mild NPDR with microaneurysms and exudate. Image courtesy of D. Wilkin Parke III, MD.
DME commonly involves microaneurysms, exudate and cystic intraretinal fluid. Based on its distribution in the macula, you can describe DME as focal or diffuse. As defined by the ETDRS, clinically significant macular edema involves either:
- Retinal thickening within 500 microns of the foveal center;
- Exudates within 500 microns of the foveal center and with adjacent retinal thickening or
- Retinal thickening at least one disc diameter in size and within one disc diameter of the foveal center.
You usually treat visually significant DME with intravitreal pharmacotherapy or macular laser and monitor the patient every three to four months.
Diabetic Retinopathy
DR is classified two ways, depending on symptoms. If the patient has dot-blot hemorrhages, cotton-wool spots, venous beading or intraretinal microvascular anomalies (IRMAs) in the absence of neovascularization, classify the DR as nonproliferative. Define the severity based on the symptoms:
- A few microaneurysms: The eye has mild nonproliferative diabetic retinopathy (NPDR).
- Findings like cotton-wool spots and dot hemorrhages (i.e., beyond microaneuryms): moderate NPDR.
- An eye with four quadrants with intraretinal hemorrhaging, two with venous beading or one with IRMAs: severe NPDR.
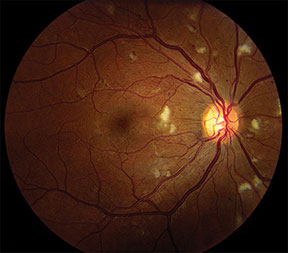
Severe NPDR with cotton-wool spots, intraretinal hemorrhage and IRMAs. Image courtesy of D. Wilkin Parke III, MD.
You can usually follow NPDR every three to six months, based on severity. Occasionally you may treat severe NPDR with a panretinal photocoagulation laser.
Proliferative diabetic retinopathy (PDR) is defined by the presence of neovascularization of the disc (NVD) or elsewhere (NVE) or vitreous hemorrhage. Although you use further criteria to identify a subcategory called high-risk PDR, you should initially deem any eye with PDR at high risk of progressing to a vision-threatening event like a tractional retinal detachment or dense vitreous hemorrhage.
PDR is classically treated with panretinal photocoagulation. With tractional detachments and persistent vitreous hemorrhage, you may need to perform vitrectomy. For all diabetic eyes, and especially those with PDR, remember to look for neovascularization of the iris (rubeosis iridae) and the angle. If the IOP is elevated as a consequence, the eye also has neovascular glaucoma.
Beyond the Retina
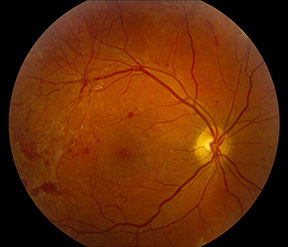
PDR with NVE and vitreous hemorrhage. Image courtesy of D. Wilkin Parke III, MD.
Diabetic eye disease often extends beyond the retina:
- Diabetic papillitis is comparable to a nonarteritic anterior ischemic optic neuropathy and usually involves unilateral optic disc edema in the setting of DR.
- Diabetes is also associated with dry eye disease, neurotrophic keratopathy, posterior subcapsular cataract and strabismus from microvascular ischemic cranial nerve palsies.
As you can see, a thorough diabetic evaluation touches on multiple aspects of the standard eye exam. Don’t rush to the retina and forget to look for motility deficits, anterior segment changes and optic nerve edema. Know how to stage DR precisely and it will guide your management and follow-up. The classification system is onerous at first, but learn it early and you’ll find that the disease becomes a lot simpler to handle.
* * *
 About the author: Wilkin Parke III, MD, is a vitreoretinal specialist with Vitreo Retinal Surgery, PA in Minneapolis and has been a member of YO Info’s editorial board since 2015.
About the author: Wilkin Parke III, MD, is a vitreoretinal specialist with Vitreo Retinal Surgery, PA in Minneapolis and has been a member of YO Info’s editorial board since 2015.