Defending Ophthalmology Code Values and Improving Medicare Reimbursements to Ophthalmologists

What we told you early this year
Medicare payment rates for cataract procedures are expected to be revised in 2020. Significant changes for coding and payment for extended ophthalmoscopy are also expected for next year. Intravitreal injection is under scrutiny for 2021, because of its continued increase in utilization.
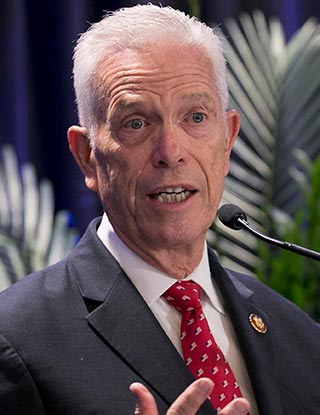
Rep. Bill Johnson, R-Ohio, is a member of the House Committee on Energy and Commerce, which wields Medicare oversight powers.
The Academy told you about our plan to gather the data that can help us present a strong case against cuts. We also pledge to work to protect ophthalmology from renewed efforts to adversely reform E/M-visit payments – a fight we’ve successfully waged in the past.
What’s happening today
We’re awaiting the next step in the annual process of code-value adjustments, when CMS unveils its proposed Medicare physician fee schedule for 2020. We partnered with the American Society of Cataract and Refractive Surgery in January to make a data-driven case for fair cataract reimbursements. The RUC then sends its recommendations to CMS for consideration of the 2020 fee schedule. We’ll know what CMS proposes for cataract reimbursements in July.
Last year, when the RUC challenged us to review the valuation for our cataract codes, we developed a robust set of data through a survey of Academy and ASCRS member ophthalmologists. The surveys also assess physicians’ work for two new combined cataract codes that were established to capture endoscopic cyclopohotocoagulation when performed with cataract surgery. Current cataract and complex cataract codes (66982 and 66984) were revised to describe a stand-alone performance before surveying for the value of the work performed by physicians.