Author: Daniel Palanker, PhD
The relaxed eye has an approximate optical power of 60 diopters (D) (ie, its focal length is 16.7 mm in air), with the corneal power being about 40 D, or two thirds of the total power. Due to orderly arrangement of collagen fibrils in the cornea, it is highly transparent with transmission above 95% in the spectral range of 400-900 nm. The refractive index of the cornea is n≈1.3765±0.0005. The amount of light reaching the retina is regulated by the pupil size, which can vary between 1.5 mm and 8 mm. The anterior chamber of the eye, which is located between the cornea and lens capsule, is filled with a clear liquid––the aqueous humor having a refractive index n≈1.3335. The crystalline lens of the eye, located behind the iris, is composed of specialized crystallin proteins with refractive index of n=1.40-1.42. The lens is about 4 mm in thickness and 10 mm in diameter and is enclosed in a tough, thin (5-15 mm), transparent collagenous capsule. In the relaxed eye, the lens has a power of about 20 D, while in the fully accommodated state, it can temporarily increase to 33 D. The vitreous humor––a transparent jelly-like substance filling the large cavity posterior to the lens and anterior to the retina––has a refractive index n≈1.335.
Aberrations
With focusing optics that are not perfect, the focal spot size of the laser beam is limited by diffraction and aberrations. Measurements of optical aberrations in the human eye demonstrate that for pupillary dilation of up to 3 mm in diameter, an average emmetropic human eye is optically well corrected, and the focal spot is close to the diffraction limit. For pupils greater than 3 mm in diameter, however, the central aberrations increase, resulting in increases in the focal spot size. Peripheral field aberrations lead to rapidly increasing blur of the image with angle of visual field, strongly limiting the focusing capability of laser in the periphery of the retina. In retinal photocoagulation, a flat contact lens is typically used to reduce the optical power of the front surface of the cornea. If the lens is used properly, it greatly aids in controlling peripheral aberrations during photocoagulation. Other methods include using an aspheric lens to control optical aberrations in the periphery during photocoagulation. The use of such lenses has many advantages, in particular by providing wide-field viewing, although aberrations are difficult to correct over the totality of fields of interest and additional reflections may be introduced by the lens surface.
Contact Lenses
Currently, retinal laser photocoagulation relies heavily on the use of contact lenses. A number of contact lenses have been developed for this purpose, and the most common types are listed in Table 1. The universal (Goldmann) three-mirror contact lens provides a flat front surface that nearly cancels the positive refractive power of the front surface of the cornea. Mirrors at 59 degrees, 67 degrees, and 73 degrees aid in visualization and photocoagulation of the periphery and anterior segment. To obtain the most reproducible results in photocoagulation, the operator should hold the contact lens so that the flat surface is within ±5 degrees of perpendicular to the laser beam. The use of mirrors in contact lenses helps the operator keep the laser beam properly aligned to the lens while photocoagulating over a large field.
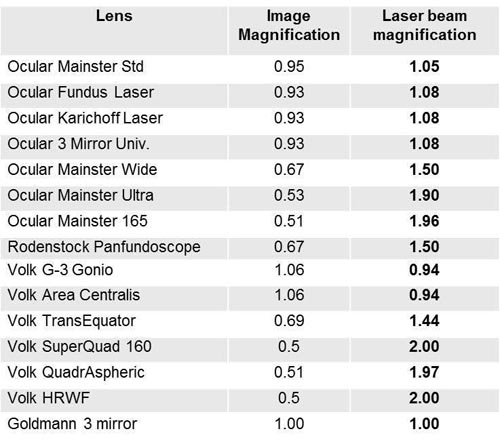
Table 1. Common contact lenses.
Another useful photocoagulation lens is the inverted image lens system, typified by the Rodenstock, Quadraspheric, and Mainster photocoagulation lenses. These lenses contain a lens element in contact with the corneal surface and another positive lens element at a fixed distance from the cornea. These systems magnify the spot size on the retina, while increasing the field of view, requiring the operator to adjust the power accordingly. Magnification factors of the most common contact lenses are listed in Table 2. It is important to keep in mind that magnification of the retinal image de-magnifies the beam size on the retina by the same amount, ie, the higher magnification of the retina, the smaller the laser spot is on the retina.
Suggested Reading
- Smith G, Atchinson DA. The eye. In: Smith G, Atchinson DA, eds. The Eye and Visual Optical Instruments. Cambridge, UK: Cambridge University Press; 1997:291-316.
- Thompson KP, Ren QS, Parel JM. Therapeutic and diagnostic application of lasers in ophthalmology. In: Waynant RW, ed. Lasers in Medicine. Boca Raton, FL: CRC Press. 2002:211-246.
- Pomerantzeff O, Pankratov M, Wang GJ, Dufault P. Wide-angle optical model of the eye. Am J Optom Physiol Opt. 1984;61(3):166-176.
- Walsh G, Charman WN, Howland HC. Objective technique for the determination of monochromatic aberrations of the human eye. J Opt Soc Am A. 1984;1(9):987-992.