Authors: Darius Moshfeghi, MD; Mark S. Blumenkranz, MD
Laser Photocoagulation and Photodynamic Therapy for Von Hippel-Lindau Retinal Capillary Hemangiomas
Retinal capillary hemangiomas (RCHs), also known as retinal hemangioblastomas, occur most frequently in conjunction with von Hippel-Lindau (VHL) syndrome. These lesions are characterized by plump, but otherwise normal, retinal capillary endothelial cells with normal pericytes and basement membrane. Astrocytes with lipid vacuoles are found in the tumor interstitia. Isolated RCH outside of VHL do occur, although they are more likely to be single, unilateral, and present later. While the overall visual prognosis for VHL-associated RCH is good, a recent report demonstrated that with mean follow-up of 8.2±4.2 years that on average patients lost of 5.1±0.6 letters.
Von Hippel-Lindau syndrome has an autosomal dominant inheritance pattern, with an incidence of 1 in 36,000 live births. These lesions can occur either singly, or more often, multiply and bilaterally, with a greater than 80% predilection for peripheral location. Vision loss can occur from exudation, strabismus, hemorrhage, and retinal detachment, as well secondary causes such as macular edema, lipid maculopathy, and epiretinal membrane. Early lesions often present as indistinct areas of redness in the retina, which appear to be retinal hemorrhages. Patients may be relatively asymptomatic until the lesions achieve larger size, and it is imperative to perform life-long surveillance of even asymptomatic individuals with VHL because smaller lesions are more easily eradicated than larger lesions. In VHL patients, RCH is diagnosed at a mean of 25 years.
Treatment of RCH includes diathermy, cryotherapy, laser photocoagulation, photodynamic therapy, and plaque brachytherapy.
Laser Photocoagulation of RCH
Thermal destruction of retinal capillary hemangiomas, beginning with diathermy, has been practiced for over 7 decades. Other variations included cryotherapy and photocoagulation. Presently, argon laser photocoagulation is a mainstay of therapy for early and small lesions, particularly peripheral lesions. Based on histopathology of enucleated specimens treated with multiple modalities, including diathermy, cryotherapy, and argon laser photocoagulation, it has be posited that RCH less than 3 disc diameters in size are amenable to argon laser photocoagulation therapy. These same specimens demonstrate regression of the RHC following thermal therapy with areas of adjacent retinal neovascularization. In advanced cases, rubeosis iridis, subretinal fluid with xanthochromic particles, and total retinal detachment have been noted following argon laser photocoagulation. Early experience with laser photocoagulation supported treatment of lesions <1 disc diameter in size.
The technique of laser photocoagulation of RCH is dependent on the location of the tumor. Peripheral tumors can be treated in a two-fold technique:
- Initial treatment of the feeder vessels; and
- Subsequent treatment of the tumor itself.
Juxtapapillary tumors are directly treated with laser photocoagulation. Shields has advocated that laser photocoagulation be reserved for RCH lesion <4.5 mm in diameter located posterior the equator. For larger and anterior lesions, he recommends cryotherapy.
Peripheral RCH Laser Photocoagulation Technique
For smaller peripheral RCH lesions, the arteriole feeding the tumor should be treated first. The draining vein should be treated in a separate session, followed by treatment of the tumor itself, beginning with the tumor margins. In a large series of patients with VHL, laser photocoagulation demonstrated excellent results at tumor control. Of interest, 82% of RCH that were initially observed remained stable over a median 84-month follow-up. Poor visual acuity outcome (≤20/400) was significantly correlated with poor initial visual acuity and presence of vitreous hemorrhage (Figure 1).
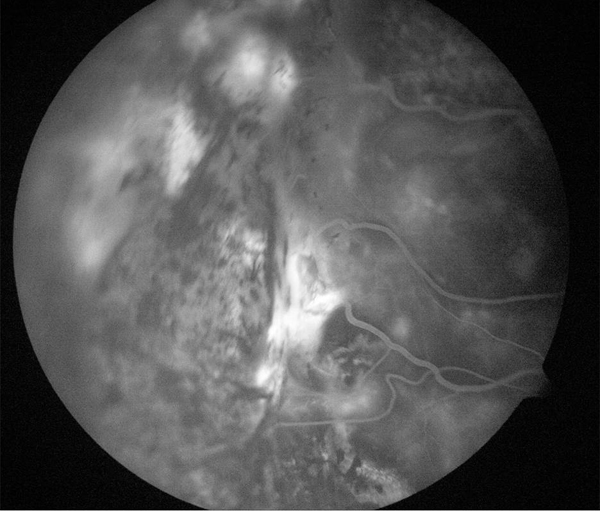

Figure 1. Treatment of leaking angioma from VHL treated with laser.
Juxtapapillary Retinal Capillary Hemangiomas
Juxtapapillary RCHs are more difficult to treat due to their location over the optic nerve and lack of clearly defined afferent and efferent feeding vessels. This treatment quandary may explain why juxtapapillary RCH are more likely to be associated with retinal detachment, exudate, and poor visual acuity outcomes. The juxtapapillary RCH also present at younger ages, with a predilection for the temporal aspect of the optic nerve. Laser photocoagulation is directed onto the tumor surface and may be supplemented with barricade and/or grid laser temporally to prevent exudate into the macula. Low-energy, long duration laser treatments in multiple sessions over several months are preferred, as originally advocated by Gass.
Summary
Retinal capillary hemangiomas associated with VHL occur earlier, more frequently, and bilaterally compared to sporadic RCHs. Argon laser photocoagulation is a good therapeutic option, particularly for peripheral lesions with small diameter and lesser thickness. Visual acuity results tend to be good for the peripheral lesions following laser photocoagulation, and more guarded for juxtapapillary RCHs. The poorer results for juxtapapillary lesions are likely related to inability to treat the feeder vessels adequately due to anatomic considerations as well as their location temporally and tendency to produce exudate into the macula.
Suggested Reading
- Chew EY, Schachat AP. Capillary hemangioblastom of the retina and von Hippel-Lindau disease. In: Ryan SJ, ed. Retina. Vol III. 5 ed. London: Saunders Elsevier; 2013:2156-2163.
- Nicholson DH, Green WR, Kenyon KR. Light and electron microscopic study of early lesions in angiomatosis retinae. Am J Ophthalmol. 1976;82(2):193-204.
- Singh AD, Nouri M, Shields CL, Shields JA, Smith AF. Retinal capillary hemangioma: a comparison of sporadic cases and cases associated with von Hippel-Lindau disease. Ophthalmology. 2001;108(10):1907-1911.
- Toy BC, Agron E, Nigam D, Chew EY, Wong WT. Longitudinal analysis of retinal hemangioblastomatosis and visual function in ocular von Hippel-Lindau disease. Ophthalmology. 2012;119(12):2622-2630.
- Lonser RR, Glenn GM, Walther M, et al. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059-2067.
- Singh AD, Shields CL, Shields JA. von Hippel-Lindau disease. Surv Ophthalmol. 2001;46(2):117-142.
- Weve HJ. Angiomatosis retina, cured by diathermocoagulation. Ophthalmologica. 1949;117(6):371.
- Cardoso RD, Brockhurst RJ. Perforating diathermy coagulation for retinal angiomas. Arch Ophthalmol. 1976;94(10):1702-1715.
- Welch RB. Von Hippel-Lindau disease: the recognition and treatment of early angiomatosis retinae and the use of cryosurgery as an adjunct to therapy. Trans Am Ophthalmol Soc. 1970;68:367-424.
- Meyer-Schwickerath G. The preservation of vision by treatment of intraocular tumors with light coagulation. Arch Ophthalmol. 1961;66:458-466.
- Rosa RH, Jr., Goldberg MF, Green WR. Clinicopathologic correlation of argon laser photocoagulation of retinal angiomas in a patient with von Hippel-Lindau disease followed for more than 20 years. Retina. 1996;16(2):145-156.
- Malecha MA, Haik BG, Morris WR. Capillary hemangioma of the optic nerve head and juxtapapillary retina. Arch Ophthalmol. 2000;118(2):289-291.
- Gass JD. Treatment of retinal vascular anomalies. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83(3 Pt 1):OP432-442.
- Shields JA. The expanding role of laser photocoagulation for intraocular tumors. The 1993 H. Christian Zweng Memorial Lecture. Retina. 1994;14(4):310-322.
- Singh AD, Nouri M, Shields CL, Shields JA, Perez N. Treatment of retinal capillary hemangioma. Ophthalmology. 2002;109(10):1799-1806.
- McCabe CM, Flynn HW, Jr., Shields CL, et al. Juxtapapillary capillary hemangiomas. Clinical features and visual acuity outcomes. Ophthalmology. 2000;107(12):2240-2248.
- Johnston PB, Lotery AJ, Logan WC. Treatment and long-term follow up of a capillary angioma of the optic disc. Int Ophthalmol. 1995;19(2):129-132.
- McDonald HR. Diagnostic and therapeutic challenges. Juxtapapillary retina capillary hemangioma. Retina. 2003;23(1):86-91.
- Gass JD, Braunstein R. Sessile and exophytic capillary angiomas of the juxtapapillary retina and optic nerve head. Arch Ophthalmol. 1980;98(10):1790-1797.