By Anna M. Horwood, PhD, DBOT
These pages outline the clinical assessment of ocular alignment and binocular vision, as well as the factors that might influence them, in typical and atypical infants. Visual acuity testing and fundus and media examination are not covered in these pages.
A companion chapter, Typical and Atypical Development of Ocular Alignment and Binocular Vision in Infants – The Background, covers the research evidence on typical and atypical development upon which these clinical methods are based.
Case History
A parental history of an infant's early-onset strabismus must be taken carefully. If the infant subsequently appears straight and binocular on examination, the child could have recently grown out of neonatal misalignments, so what the parents describe may have been genuine, but is no longer there (Figure 1).

Figure 1. Neonatal misalignments in a 4-week-old infant that resolved completely by 3 months of age. In this case misalignment was noted approximately 20% of waking hours.
For the infant with an obvious strabismus, the important question is not just when the deviation started, but when was it constant or intermittent at the start, and was the deviation the same size as it is now? Genuine infantile esotropia may have been much smaller or intermittent in the first weeks of life.
Any history of clear and constant eso- or exotropia from early infancy should be taken more seriously, as it could indicate poor vision or a cranial nerve palsy. Birch and colleagues1 reported that large-angle constant esotropias noted at 2 to 4 months of age did not spontaneously resolve, but a few infants with small- or variable-angle esotropia did regain normal alignment.
Essential infantile esotropia is not now thought to start from birth, and may have a more intermittent onset, or be of smaller angle. The esotropia seems to be a consequence of maldevelopment of normal binocular vision, rather than the primary cause. A few infants observed by their orthoptist mothers who did develop genuine infantile esotropia, as opposed to neonatal misalignments, were indistinguishable in the first month from the typical infants who grew out of the deviation. Their deviations were becoming more frequent in the second month, but only became constant and with increasingly large angles after 4 months of age (Figure 2).2
Parents of such children rightly say the strabismus started at birth, but if questioned closely will report that it was not initially constant or so large.

Figure 2. Progressive increase in infantile esotropia angle in a case tested in the author’s laboratory.
The onset of intermittent exotropia is often difficult to pinpoint because although there are published reports that the onset is often at birth,3 the large angle kappa of infancy may make an infant's eyes look divergent when they are not. In a large series of infants observed from their first weeks, the author has also seen a few children as neonates with what appeared to be genuine very large-angle exotropia, which subsequently disappeared in later months, only to re-emerge as intermittent exotropia in later childhood (unpublished data).
Early-onset accommodative esotropia is known to occur occasionally in hyperopic infants4 and may relate to concentration on smaller objects but is probably impossible to distinguish from neonatal misalignments in infants of less than 4 months of age, as mild hyperopia can also resolve with emmetropization.
Family photographs are invaluable. They may enable the ophthalmologist to reassure parents about a pseudostrabismus due to epicanthus, or alert the ophthalmologist to a deviation that has since disappeared or cannot be elicited in the examination room.
A history of prematurity indicates higher risk of strabismus and refractive error (aside from any retinopathy of prematurity [ROP]-related strabismus). Clinical findings and milestones, such as expectations of finding stereopsis or appropriate accommodation, should be related to corrected (gestational) age in premature infants.
Observations
Epicanthus can cause a very strong illusion of strabismus and is a common reason that infants are referred for assessment. Non-family members may be more concerned about a possible strabismus than the child’s own family, who may be accustomed to most infants in their family looking similarly pseudostrabismic.
Parents often bring photographs of a “strabismus” in a child with pseudostrabismus due to epicanthus. This is particularly noticeable when the infant is looking slightly to one side as the nasal sclera is covered by the epicanthus. Using the photograph to explain the effect to parents and point out symmetrical corneal reflections can be very helpful (Figure 3).

Figure 3. Pseudostrabismus due to epicanthus.
All pediatric ophthalmologists are taught to use the corneal reflections of a spotlight to assess the angle of deviation, and quickly become familiar with the “normal ranges” in older children. For professionals seeing fewer neonates, the neonatal corneal reflections can look excessively nasal due to the much larger angle kappa, so can suggest an exotropia.
It is particularly easy to feel there is an exotropia if the infant is looking just past the examiner’s head to look at a window or bright light behind them, which they often like to do. The slight lateral gaze makes the corneal reflection of one eye move temporally, so it looks “normal,” while the other has moved more nasally, giving the appearance of an exotropia in that eye, when in fact both eyes are straight, but just not fixating the examiner (Figure 4 and Video 1). As long as the tester is sure the child is fixating, the symmetry of the corneal reflections is more important than their absolute position, because angle kappa can vary widely. Professionals examining the ocular alignment of neonates need to be aware of this possible bias, and it sometimes helps to not concentrate on the corneal reflections but on the overall impression of alignment.
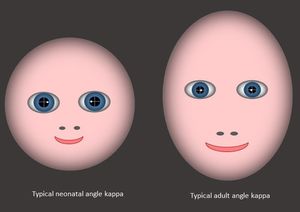
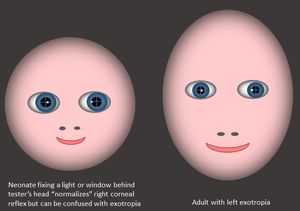
Figure 4. Infant angle kappa as compared to adult angle kappa
Video 1. Infant angle kappa as compared to adult angle kappa
A useful technique for clinicians is to make observations of alignment while standing behind the caregiver’s back (preferably the primary caregiver) while they hold the baby up in front of them and engage the infant’s attention. An infant may look at a window or light in preference to an unfamiliar professional’s face, but will usually fixate their caregiver intently. The caregiver can also slowly rotate the baby horizontally and vertically while maintaining fixation, while the ophthalmologist looks on, as a useful way to assess motility or smooth pursuit movements if conventional testing fails.
Fixation and following in very young infants is less easy to elicit in busy visual environments, such as a “child friendly” room with multiple pictures and toys. A single illuminated target in a dimly lit room may elicit normal fixation, motility or fusional responses that are not possible otherwise.
It is important that the target is silent if fixation and following are also being used as a marker for visual acuity.
The Brückner Test
The Brückner test screens for strabismus, anisometropia, media opacities, abnormal pupil reactions, and fundus anomalies near the visual axis. It takes seconds, is nonthreatening, and it does not require close proximity to the infant, so it can be done with minimal cooperation. It is therefore a good way to start a retinoscopy or ophthalmoscopy. The infant gets used to the instrument light and some initial assessment can be made before getting closer. An ophthalmoscope beam set at zero is used to straddle both eyes from a distance of > 0.6 m. Any asymmetry or abnormality of the brightness or color of the red reflex is suspicious. In strabismus, off-axis fixation in one eye causes a brighter reflex in that eye (Figure 5). Reflective crescents toward the top or bottom of the pupil indicate refractive error. (Although this image is of an older child, other Brückner test images of children of various ages can be found at the Alaska Blind Child Discovery website and the Oman Journal of Ophthalmology website).

Figure 5. Brückner (red) reflex in left eye (American Academy of Ophthalmology 2014)
Retinoscopy
Assessment of refractive error is integral to assessment of strabismus. Cycloplegic retinoscopy remains the gold standard test of refractive error, but Mohindra (near) retinoscopy can be a useful noncycloplegic technique to identify or monitor infant refractive error without dilation. Experience and a calm examination technique can reveal errors only slightly less hyperopic than those found on cycloplegic refraction.5 For infants, the test is carried out in the dark and the infant can fix the retinoscope streak. An “against” movement is often found at first, but with time the accommodation relaxes and a “with” movement can gradually emerge and build as the child relaxes. A soothing, calm technique and time may help an infant to relax. The Mohindra technique is particularly useful for monitoring emmetropization in an otherwise healthy infant with an initially significant refractive error (eg, neonatal astigmatism) that is being monitored as it reduces over time, and where there is no other indication for repeated cycloplegia.
Photoscreeners
Commercial photoscreeners such as the Suresight or Plusoptix can be useful to screen for risk factors similar to those detectable by a Brückner test. However, most photoscreeners require a period of steady and central fixation, which can be difficult to achieve in very young infants.
Ocular Motility
Any engaging target can be used to assess ocular motility in an infant. It is useful to have a selection of bright, noisy toys that can be introduced in turn to provide novelty. A brightly illuminated target will allow concurrent assessment of corneal reflections. Neonates may exhibit “sticky fixation,” so saccades to a new target may be slow to initiate, especially if they have just been fixating a human face, which is a highly salient target. Smooth pursuit (as opposed to the vestibulo-ocular reflex below) is often best elicited by engaging fixation on the examiner then by either the examiner moving, or by holding the infant’s head and slowly rotating it sideways or vertically while engaging their fixation on the examiner’s face.
The Vestibulo-Ocular Reflex (VOR) (The “Swinging / Spinning Baby Test”)
Observing the vestibulo-ocular reflex is another useful way of assessing both gross visual acuity and ocular motility. By rapidly rotating an infant held facing and tilted slightly towards the examiner5 (Figure 6), a reflex bilateral eye movement in the opposite direction to the rotation will be elicited. More prolonged rotation will induce vestibular nystagmus that is still visible when the rotation stops. Sighted infants will normally suppress this nystagmus within a few beats. More prolonged nystagmus indicates poor vision. The same technique is useful for checking for full adduction or abduction, for example in an infantile esotropia with cross fixation or Duane syndrome, where poor cooperation or attention limits conventional ocular motility testing in a child with an apparent restriction on conventional motility testing.

Figure 6. The vestibulo-ocular reflex test
Cover Testing
A conventional cover test, occluding each eye in turn to observe a fixation movement of a deviating eye, and recovery of a heterophoria, may be possible. Many infants, however, object or become fussy when either eye is occluded, so it can be unreliable. Refixation movements are typically slow, and by the time they occur, the infant may have become distracted by the occluder. If the child will tolerate occlusion, comparison of the response to occlusion of either eye can be very valuable. Occlusion of the better-seeing eye will elicit a stronger reaction than occlusion of an eye with poor vision. Attentional limitations mean the most infants will not reliably fixate targets in the distance, so intermittent exotropia may be impossible to elicit at first.
Induced Tropia Test
Fixation can be assessed by placing a base down prism over one eye while the infant is fixating on a near accommodative target. An upward deviation indicates that the eye is fixating without suppression, and alternation of the eyes up and down indicates switching of fixation between the eyes and suggests that both eyes have good vision (although this test does not detect mild amblyopia reliably). If the eye does not shift upward after several seconds with the prism placed base down in front of it, it is likely the eye is being suppressed or has significant amblyopia.
Motion Detection
Monocular optokinetic nystagmus (OKN) can be elicited by repeated refixations on the vertical black/white gratings of an OKN drum or tape moving horizontally. Typical infants will follow the stripes monocularly temporally to nasally, but not nasally to temporally. Development of symmetrical monocular OKN is associated with developing binocularity but remains somewhat asymmetrical throughout the first year of life. Persistent asymmetry is associated with infantile esotropia.
Strabismus Angle Assessment
Alternate prism cover testing is rarely possible with young infants, so clinical assessment of the angle of deviation often relies on objective assessment of the symmetry of the corneal reflections in relation to the pupil center (usually equally nasal—with a small positive angle kappa) when fixating a light either with (the Krimsky Test) or without (the Hirschberg Test) a correcting prism.
Corneal reflections can be abnormally displaced or asymmetrical in cases of dragged fovea in retinopathy of prematurity because of an increased angle between the visual and optic axes. This can lead to large pseudostrabismus despite bifoveal fixation.
Although angle kappa reduces dramatically in the first 9 months of life as the posterior chamber develops, the Hirschberg ratio (the angular change associated with 1-mm lateral displacment of the corneal reflection) does not, and it remains relatively stable from birth at approximately 21∆/mm7 (larger than the widely quoted 7°/15∆/mm). So although neonatal corneal reflections may appear abnormally nasal in comparison to older children and adults, an asymmetry of 2 mm will mean approximately 40∆ at any age.
Tests of Sensory Binocularity
Laboratory studies generally agree that stereoacuity is rarely found before 12 to 16 weeks, but even after that, infants in a clinical situation may not be interested in clinical stereotests in a typical office environment (as opposed to the laboratory techniques used to research development). By 4 to 5 months, some may eye-point to a stereoscopic preferential looking task or random dot tests as the Lang, Randot, Frisby, or TNO tests, but many sociable infants will prefer to fixate the tester if they can. By 6 months, a few infants will try to touch a random dot figure.
Tests of Motor Fusion
Although it is not clear whether at first “convergence” is true motor fusion or just 2 independent adduction/fixation movements, most infants will converge slowly to a bright unambiguous target such as a light-up jelly monster on a penlight from around 2 to 3 months. A 20D base-out prism can also elicit fusional convergence of the eye behind the prism. At first the response can be very slow to occur, so allow plenty of time. Responses can be elicited in younger infants by dimming ambient lighting to remove any visual distractions.

Figure 7. Illuminated target useful for testing in the dark. Sufficient light is provided by the target to allow assessment of fusion or motility without any other visual distractions.
Before 4 months of age infants may “get stuck” in convergence for a few seconds before recovery after such a convergence task, because the divergence phase as the prism is removed is usually more delayed and slower than the initial convergence phase. This is particularly easy to elicit in very young infants if testing is done in the dark when the only light is that provided is from the target (Figure 7). This response may coincide with time that parents report neonatal misalignments.2 This “getting stuck” behavior is not a sign of abnormality unless it persists beyond 4 months of age. Parents who say their infant is strabismic at home, but the infant appears straight on the examination day, can find it very reassuring when the examiner can elicit this response when other testing has failed to demonstrate a strabismus, as it can prevent them feeling that they have not been believed.
Accommodation
Mohindra (near or dark) retinoscopy is a very good way to assess refraction and accommodation. Hyperopia that builds slowly shows that the infant must have been accommodating to overcome the hyperopia at least some of the time.
Hypermetropic infants may accommodate to overcome their refractive error, but many systematically underaccommodate in relation to their refractive error, despite making appropriate near-distance changes.8 They therefore appear to accommodate to maintain a stable level of blur, but never fully clear the image for naturalistic fixation tasks. The same study showed that infants destined to emmetropize accommodated slightly more for near than distance, while those who did not emmetropize underaccommodated more for near. Differences were small, however, so they would probably not have been detectable clinically.
Dynamic retinoscopy to an engaging target such as an illuminated toy or a smartphone image can be surprisingly easy in small infants to see if they are overcoming any significant hypermetropia.
|
Table 1. Typical Visual Behavior in Infants <4months of age
|
|
Gross alignment
|
|
Preference for faces (especially the main caregiver), windows and bright lights
|
|
Large angle kappa so may look exotropic
|
|
Occasional large angle esodeviation possible up to 15% of waking hours—often seen after attempting near fixation
|
|
“Sticky fixation:” slow to refixate a new target
|
|
Poor acuity and contrast sensitivity, but adequate for social interactions
|
|
Slow convergence to near targets or prisms, slower relaxation sometimes preceded by inappropriate over-convergence
|
|
Wide range of refractive errors under cycloplegia, but myopic focus when undilated
|
|
Accommodation relatively unresponsive and poor to relax. “All or nothing” responses common.
|
|
Asymmetrical monocular optokinetic nystagmus (OKN)
|
|
Unreliable link between convergence and accommodation
|
|
Table 2. Warning signs for geniune strabismus in an infant in the first 6 months of life
|
|
Parents see a constant deviation at any age
|
|
New misalignment after 3 months of age
|
|
Parents say an intermittent deviaton noticed from birth is worsening from 2 months of age, or not fully resolved by 4 months
|
- Birch E, Stager D, Wright K, Beck R. The natural history of infantile esotropia during the first six months of life. Pediatric Eye Disease Investigator Group. J AAPOS.1998;2:325-328; discussion 329.
- Horwood AM, Riddell PM. Can misalignments in typical infants be used as a model for infantile esotropia? Invest Ophthalmol Vis Sci. 2004:45, 714-720.
- Costenbader F. The physiology and management of divergent strabismus. In: Allen JH, Strabismic Ophthalmic Symposium I, 1950 St. Louis,. Mosby-Year Book, Inc.
- Havertape SA, Whitfill CR, Cruz OA. Early-onset accommodative esotropia. J Pediatr Ophthalmol Strabismus. 1999:36, 69-73.
- Thorn F, Gwiaxda J, Held R. Using near retinoscopy to refract infants. In: Vital-Durand F, Atkinson J, Braddick O. (eds.) Infant Vision. Oxford: Oxford University Press.
- Hoyt C, Taylor D. Pediatric Ophthalmology and Strabismus, Edinburgh, Elsevier Saunders.
- Riddell P, Hainline L, Abrahamov I. Calibration of the Hirschberg test in human infants. Ophthalmol Vis Sci. 1994:35, 538-543.
- Horwood A, Riddell P. Hypo-accommodation responses in hypermetropic infants and children. Br J Ophthalmol 2011:95, 231-237.