Accessory lacrimal ducts are a congenital defect of the nasolacrimal system that typically presents later to the ophthalmologist than congenital nasolacrimal duct obstruction (CNLDO). Parents often note increased tearing on one side, especially with crying (Figure 1). Sometimes there is an associated dermatitis. Parents do not usually note any significant discharge unless it is associated with CNLDO. Accessory lacrimal ducts most frequently present in the medial lower lid and connect with the canaliculus or the nasolacrimal sac. They can be demonstrated by placing fluorescein-tinged balanced salt solution in the conjunctival fornix (Figure 2). If there is a connection with the nasolacrimal system, the fluorescein will drain through the accessory duct, nicely outlining the external location of the duct (Figure 3). The accessory ducts can be quite subtle in many cases.
The area of the duct is injected with xylocaine with epinephrine a few minutes prior to the excision (Figure 4). This helps with pain control postoperatively, decreases bleeding during the case, and minimizes the amount of general anesthesia required during the case. A circumlinear incision is made around the accessory lacrimal duct (Figure 5), usually with a blade, and then the accessory duct must be dissected back a minimum of a few millimeters, but preferably most of the way back toward the canaliculus or nasolacrimal sac (Figure 6). The dissection should include the entire tract of the accessory lacrimal duct. The location of the canaliculus or sac will be recognized if the probe has been left in place during the case. Care should be taken not to damage the canaliculus (Figure 7). Any bleeding can be controlled with bipolar cautery. The defect should then be closed with 1 or 2 interrupted absorbable sutures such as 6-0 mild chromic, or 7-0 vicryl (Figure 8). The advantages of this type of suture are that it can remain in place for 10-14 days before dissolving and that there is no need to remove it, making it preferable to nonabsorbable sutures for use in young children. If performed appropriately, the tract should not recur; however, if the dissection is not deep enough or if too much of the tract is left in place, recurrence is more likely.

Figure 1. Accessory lacrimal duct / fistula.

Figure 2. The Ritleng stent introducer is placed through the lower lid punctum and the Ritleng medium collarette stent woven through the introducer and retrieved from the nose.

Figure 3. Marking the accessory lacrimal duct.

Figure 4. Injection of 1% lidocaine with epinephrine around the duct mainly for hemostasis.

Figure 5. The accessory duct is probed with the “0” probe.
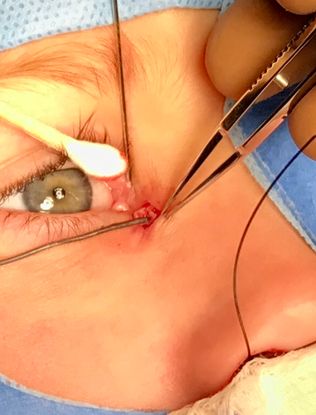
Figure 6. Dissecting the accessory duct down to the lacrimal sac.

Figure 7. Completion of dissection of the accessory duct.

Figure 8. Closure of the lacrimal sac opening, deep tissues, and skin in layered fashion.