Introduction
Surgical correction for adult strabismus is occurring at an increased rate, as noted in a study comparing surgical rates between 2000 and 2014.1 Understanding the impact that strabismus has on patient function, independence, safety, and sense of well-being is as integral to care as understanding the evaluation and solutions that benefit their lives.
Preoperative Considerations
Adults usually arrive in our examination rooms because they have compelling reasons to proceed with action: diplopia, blurred vision, asthenopia, effect on driving or work performance, social anxiety, and more. Diplopia may be caused by several different medical entities, which can be evaluated with laboratory and neuroimaging studies (Table 1). Adults with strabismus face many types of losses to recognize. They may have diplopia that is limiting their activities of daily living such as driving, with a resultant loss of independence if they remain housebound. Some may drive while closing 1 eye, which is challenging. Others require increasing prism use to control symptoms, which can lead to heavy, uncomfortable glasses and visual distortions in the glasses. Diplopia can present an occupational hazard for workers who rely on single vision to safely complete their work using heavy machinery, power tools, driving, or moving up and down ladders.
Table 1. Laboratory and neuroimaging studies for diplopia
|
Risk Factors for Diplopia
|
Tests to Perform
|
|
Hypertension
|
Blood pressure check
|
|
Diabetes mellitus
|
Fasting glucose, hemoglobin A1C
|
|
Thyroid myopathy
|
Thyroid function
|
|
Trauma
|
MRI or CT scan
|
|
Tumor
|
MRI scan
|
|
Neurodegenerative
|
Examination by PCP for Parkinson disease
|
|
Lax orbital pulleys
|
MRI scan
|
CT = computed tomography; MRI = magnetic resonance imaging; PCP = primary care physician
Diplopia presents a safety risk while walking, particularly in older patients, as diplopia can represent a fall risk.2 When there is dependence on glasses for single vision, not wearing glasses for even a short time can have serious consequences. Alternatively, patients may have a significant large-angle strabismus that they find difficult to live with at work and in social situations. The psychosocial impact and loss of self-esteem is evident in conversation with affected patients (Table 2). Many studies over decades of time have repeatedly shown the negative psychological effects strabismus has on employment, self-image, and social interaction.3-19
Table 2. Psychosocial impact in adult strabismus
|
Patient Considerations
|
Psychological Effects
|
|
Loss of independence
|
Fear of motor vehicle accidents (MVA), fall risk, fewer activities, social isolation
|
|
Loss of self-esteem
|
Social interaction discomfort
|
|
Loss of wages
|
Employer discrimination
|
For these reasons, adults tend to be motivated by and receptive to interventions such as prisms in glasses or surgery. A full examination of the ocular motility and fusion status needs to be performed before a plan for treatment can be formulated. Checking the ductions and versions can uncover weaknesses, palsies, or restrictions. Evaluating the fusional status by using stereoacuity tests such as the Randot or Titmus fly can be useful, and if there is no stereopsis, the Worth 4-dot test can demonstrate some peripheral binocularity (Table 3).
Table 3. Tests of ocular motility and fusion
|
Test
|
Purpose
|
|
Best corrected visual acuity
|
Refraction
|
|
Cover/uncover testing
|
Tests tropia vs phoria
|
|
Alternate prism cover testing
|
Measures tropia and phoria
|
|
Prism/cove test
|
Measures tropia
|
|
Worth 4-dot test
|
Measures sensory fusion
|
|
Stereoacuity Test
|
Measures level of binocularity
|
Approaching any discussion of surgery needs to be done with a clear explanation of the rehabilitative nature of strabismus surgery. Educating patients regarding the intended benefits of improved or maintained stereoacuity, as well as improving the ocular alignment, must be done. The successful maintenance of postoperative alignment is influenced by the level of vision and fusion, and this must be discussed as well. Internet posts on social media sites and optometric websites spreading disinformation, or anecdotal experiences stating that patients do not benefit from surgery introduce a bias, and must be addressed.20 With a better understanding of the reasons for surgery, and with appropriate expectations, the patient will be better equipped to make an informed decision.
Discussing appropriate expectations is key with patients who have diplopia. It is important to explain the goal of increasing the field of single binocular vision, as opposed to completely eliminating diplopia. If the angle of strabismus is small, comitant, and amenable to prismatic correction, or if there is reluctance for surgery, prisms may be an effective solution. In situations with incomitance, prisms will bring single binocular vision in some but not all fields of gaze, and this limitation needs to be discussed. Patients need to understand that they will still have diplopia in side gaze with prisms. Surgery can address surgical misalignment with incomitance to improve the ocular alignment in different gaze positions to expand the range of single binocular vision. In addition, it is important to discuss that there may be a change in the extraocular muscle function over time after the intervention, which could require an update of the level of prism in glasses, or a second surgery.
Surgical Planning
There are a few principles to consider when planning strabismus surgery. For underfunctioning muscles, repair the limitation if possible. For example, if a patient had a surgery in childhood for esotropia and subsequently develops a consecutive exotropia, and the previously recessed medial rectus is underacting on examination, strengthening the medial rectus can result in a better range of motion and field of single binocular vision than weakening the lateral rectus. If there is no underaction present, then weakening the muscle in the field of overaction, in this case with a lateral rectus recession, is indicated.
Another principle is to match deficits. An example of this is in incomitant situations such as a sixth nerve palsy. If after an inferior and superior rectus transposition to the lateral rectus (Knapp procedure) there is residual diplopia in the temporal field of the affected eye due to persistent underaction of the lateral rectus, then weakening the yoke muscle with a posterior fixation suture of the opposite medial rectus can help increase the area of single binocular vision in the affected field.
A third principle is to limit the creation of additional misalignments.21 This comes with planning the various outcomes of the initial surgery, then anticipating and limiting the secondary changes in alignment that may result. An example of this is in an adult with thyroid myopathy causing diplopia due to motility deficits (Figure 1). The MRI scan shows enlarged right inferior rectus and left superior rectus on coronal view (Figure 2). These muscles were also confirmed to be tight on forced duction testing. Conventional eye muscle surgery on 1 muscle will likely result in good alignment in primary gaze, but it will induce a deficit in the field of action of the operated muscle, leading to diplopia in that gaze. Planning the surgery using adjustable sutures on the tight right inferior and left superior rectus muscles can make the alignment more precise in primary gaze. By adding a posterior fixation suture to the corresponding right superior and left inferior rectus muscles, one can prevent a secondary deviation in the vertical field of gaze affected by the recessed muscles.
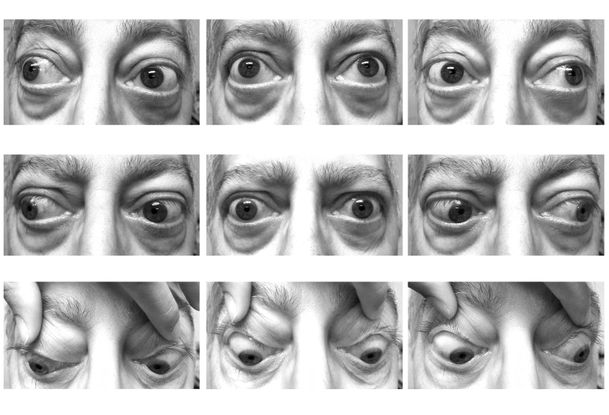
Figure 1. Thyroid myopathy causing diplopia due to motility deficits in an adult.

Figure 2. MRI scan showing enlarged right inferior rectus and left superior rectus on coronal view.
Prism adaptation
Prism adaptation is helpful to prevent surgical undercorrections. For an adult with longstanding exotropia, the patient may have diplopia with less than the total measured prismatic correction. In order to prism adapt a patient, a temporary Fresnel prism is placed on a patient’s glasses for the maximum amount of prism tolerated by the patient. On the return visit, the strabismus is again measured, and if a larger deviation is tolerated, the Fresnel prism is increased to the larger angle. This is repeated until the largest prism tolerated is determined. In this way, the maximum amount of surgery tolerated without diplopia can be quantified, and surgery for this angle used to correct the full deviation and prevent postoperative undercorrection.
Adjustable sutures
Once strabismus surgery has been chosen, and repeat measurements of the ocular alignment are noted to be stable, surgical dose tables are consulted to determine the amount each muscle will be recessed, resected, or plicated. The amount of surgery performed is also influenced by many factors including axial length, previous muscle surgery, scarring, and muscle or orbital restrictions or limitations to movement. For example, a larger eye will respond less than a smaller eye to the same amount of surgery. In addition, a neonatal eye is smaller and the insertions are closer to the equator than in an older child, so less surgery will be more effective. One other example is that advancing a previously recessed muscle will be more powerful than a resection of the same number of millimeters. With all of these examples, the table numbers will need to be adjusted to prevent under- or overcorrection. After reviewing all of the factors that play a role, the amount of surgery to perform on each muscle is determined by the surgeon.
Adjustable sutures offer the ability to evaluate the result of the strabismus surgery, then make a change that could improve the postoperative result. Adjustments can be made immediately following surgery, or after a delay of several hours to a few days, according to the surgeon’s preference and training. Many studies of the adjustable suture technique have been performed. Most are retrospective and few directly compared adjustable techniques to nonadjustable techniques. To date, there are no randomized, prospective, controlled clinical trials addressing this topic.22,23
Candidates for an adjustable suture include most adult patients who can tolerate the adjustment, so patient selection is important. Some pediatric ophthalmologists reserve the adjustable suture for adult patients with paralytic or restrictive strabismus. General indications for the use of adjustable suture techniques are restrictive strabismus, previous trauma or surgery, slipped or lost muscle, incomitant deviations, combined vertical, horizontal, and torsional deviations, and longstanding complex strabismus. Patients with type I Duane syndrome or a complete abducens nerve palsy may benefit from various procedures. One involves 1 or 2 horizontal rectus muscle recessions: the recession of a medial rectus of the affected eye and the contralateral medial rectus. Another technique is a transposition of both vertical rectus muscles to the affected lateral rectus muscle insertion, with or without posterior fixation sutures. A third procedure that has been suggested to lessen the risk of anterior segment ischemia is a superior rectus transposition to the lateral rectus. An adjustable suture may be helpful to manage any potential vertical misalignments that can occur in this setting.24,25
Overcorrection of a hypertropia after surgery on vertical muscles in thyroid surgeries has been reported. This has resulted in the recommendation to leave the muscle in an undercorrected position after an adjustable suture is used in this entity, in order to improve the ultimate result and limit reoperations.26,27
Same-day adjustments can be performed after strabismus surgery that was performed with retrobulbar anesthesia using lidocaine,28 once the lidocaine has lost efficacy, or after recovery from general anesthesia. Some surgeons are using topical anesthesia for straightforward cases, and adjustable sutures can be done in the operating room. Others prefer a brief general anesthesia using propofol or sevoflurane, with wake-up and adjustment in the operating room under topical anesthesia. Many surgeons prefer to adjust the next day, or anytime within the week of surgery, in the office under a local anesthetic.
When performing an adjustment in the office after surgery, several components will be necessary to have on hand in preparation: 1) a sterile tray of instruments including a lid speculum, forceps, needle holder, saline cannula, Westcott scissors, cotton tips, and sterile gauze pads; 2) a strong light, either of operating room strength in a procedure room, or a similar light source on a stand; 3) a near card and visual acuity wall chart; 4) prisms and an occluder; 4) patient’s glasses without prism. The patch is removed, and topical anesthesia is placed on the surgical eye for comfort. After the vision is obtained, measurements are made while looking at a distant Snellen chart and a near card. If an adjustment is needed, the patient is placed in a supine position, topical anesthesia is applied, then an adjustment is made. The alignment is measured again. When the alignment is satisfactory, the knot is tied down and trimmed, and the ends are tucked under the conjunctiva.
Botulinum toxin A
Treatment of adult strabismus is often managed with incisional surgery; however, botulinum toxin A can be a valuable addition.
Botulinum toxin A has been used in several entities, with variable success, when evaluating the ultimate alignment. In patients with acute sixth nerve palsy, botulinum toxin has a role in promoting realignment in a timely manner that may help recover binocularity.29 However, there is evidence that there may not be a difference in the ultimate alignment between patients who received the treatment and those who did not receive the treatment.30 Early botulinum toxin injection in this setting is useful for patients who are diplopic and debilitated from the diplopia, and who are not tolerating prisms, cannot afford the prism, or have no need for glasses otherwise.
Similarly, in patients with either a complete or incomplete abducens nerve palsy, botulinum toxin A has been used to relax the tight medial rectus in place of a medial rectus recession, and augment the transposition of both vertical muscles to the lateral rectus. When used as an adjunct in this way, it reduces the concern for anterior segment ischemia by reducing the surgery on rectus muscles. A multi-center study comparing the use of vertical rectus muscle transposition and botulinum toxin A to the medial rectus muscle versus surgery alone showed that botulinum toxin A enhanced the surgical outcome; however, second surgeries and prism are often needed to improve the overall success rate.31
The results of injecting botulinum toxin A to the recessed lateral rectus, in addition to resection of the medial rectus, in patients with large-angle sensory exotropia has shown good results with improved alignment and cosmesis. This has the added benefit of limiting the procedure to the eye with poor vision.32,33
Intraoperative Considerations
Surgical preparation
Preventing postoperative infection is important, because visual loss can result if an infection develops. The rate of infection after strabismus surgery has been described as low, varying with the site of infection. For conjunctivitis, the rate has been reported as about 3% of cases,34 while for orbital cellulitis the rate is from 1 in 100034 to 1 in 1900.35 Applying povidone-iodine to the conjunctival sac before surgery has been shown to reduce ocular surface bacteria when used before surgery.36 Despite various preparation and draping precautions, a high rate of contamination of suture material and needles in strabismus cases has been described, with a rate of 29.2% to 34.6%.37 Another study evaluated the rate of suture contamination with either no pre-treatment or pre-treatment with either antibiotic/steroid or antiseptic and antibiotic/steroid. They reported a rate of suture contamination that was 28% in controls that reduced to 9% with a combination of antiseptic and antibiotic/steroid pre-treatment. The authors attributed the infections to contamination from lashes and skin.38 Additional infection preventative strategies include applying a second instillation of povidone-iodine, followed by a pause of 2 minutes before making the conjunctival incision, which decreased the rate of contamination of the surgical site and sutures from 25% to 10% in another study.39
Oculocardiac reflex40
The oculocardiac reflex is defined as a 20% reduction in the heart rate, asystole, or a new arrhythmia occurring after traction on an extraocular muscle. It is transmitted through the trigeminal and vagus nerves and can also occur after pressure on the orbit or globe. Surgery on the medial rectus muscle is the most likely to induce the oculocardiac reflex, and it is more common in children than adults. It is imperative for the surgeon to immediately release any tension on the extraocular muscle, which can dampen the response. If the oculocardiac reflex persists or recurs, the anesthesiologist can treat with an anticholinergic such as atropine or glycopyrrolate, which will blunt the response so the case can safely proceed. The reflex does extinguish over time, so the surgeon may choose to wait, retesting every 30-60 seconds until the reflex does not recur, if the patient is not able to tolerate the cardiac side effects of either atropine or glycopyrrolate.40
Thin sclera
When a patient is highly myopic, the sclera can be quite thin, and the thinnest sclera is located posterior to the rectus muscle insertions.41 Scleral perforations present an overall low risk of strabismus surgery, occurring at a rate of about 1% in adults. For enhanced safety during recessions, hang-back recessions are one option to reduce risk. Hang-back recessions involve placing the scleral passes through thicker sclera at the original insertion instead of through thinner sclera at a recessed location.42 This may lead to a less desirable outcome, with both overcorrections and undercorrections, however. One study identified greater success with a conventional recession compared to a hang-back technique in treating exotropia, as they reported late overcorrections from the hang-back technique.43-46
Although a few studies have shown similar efficacy between a hang-back technique and conventional recession for treating exotropia in the short run, when looking at longer-term outcomes, the conventional recession appears to be more successful.44-47 Consequences of a scleral perforation include vitreous hemorrhage, retinal detachment, and endophthalmitis, which can have a devastating visual result, including NLP final vision.45 The best visual outcomes occur when the infection is identified early after surgery with immediate vitreous tap for gram stain and culture, followed by the injection of antibiotics. Early diagnosis can be difficult in children, who cannot always communicate their symptoms, compared to adults. Therefore, it is best to instruct parents to be vigilant in recognizing the signs of endophthalmitis in the postoperative period, especially during the first 2 weeks, and to communicate to the surgeon any signs that occur.48,49
Conjunctival Considerations
One aspect to consider when approaching a patient undergoing complex strabismus surgery is the level of tissue fibrosis in place before the surgery begins. The conjunctiva and Tenon capsule may be scarred due to prior strabismus surgery, from a scleral buckle, or a glaucoma valve, or an oculoplastic procedure, with inadvertent fibrosis.
Additionally, the conjunctiva in adults is considerably more friable than that in children, and it needs to be handled with care during the incision and throughout the case to ensure that it can be properly closed at the end of the case. Judicious use of cautery is needed to prevent extensive subconjunctival hemorrhage postoperatively, which can lead to other complications such as a dellen (see below). However, cautery that is too aggressive can tear or contract the conjunctiva, either of which can complicate closure at the end of the case.
There is a potential role for an amniotic membrane graft to act as a protective layer separating the muscle from possible subconjunctival, Tenon capsule, or scleral fibrosis. Another use of an amniotic membrane graft is to cover defects due to a retracted or otherwise inadequate conjunctival layer. After completion of the muscle surgery, the sclera may be exposed and the conjunctiva may not cover the defect adequately. An amniotic membrane graft can be used to cover the defect. The graft can be glued or sutured into place with the edges under adjacent conjunctiva, serving as a scaffold over which epithelial cells spread. There is a risk of developing a secondary restrictive strabismus if the amniotic membrane contracts. When the surgical plan includes an amniotic graft, the authors have found greater success in the outcome.50
If an amniotic graft is not available, a conjunctival autograft can be taken from the superior conjunctiva of the fellow eye and used to bridge the gap. This consideration needs to be discussed in at-risk cases preoperatively to avoid postoperative surprises when the patient has only 1 eye to be operated on. Finally, leaving the conjunctiva to heal by secondary intent is an option if other options are not available. In this case, the conjunctiva is closed only where it does not exert traction on the eye when ducted away from the incision. Forced ductions are key in all adult surgery to ensure that a restriction will not be induced by conjunctival closure postoperatively. Topical steroids should be used postoperatively in these cases to delay wound healing, which prevents aggressive healing that can cause a symblepharon.
Corneal Considerations
In adults undergoing strabismus surgery with an adjustable suture, the postoperative vision in the operated eye is very important to complete the adjustment. Intraoperative corneal drying can be prevented by placing gelfoam soaked in balanced salt solution or by using a viscoelastic on the cornea during the case. Similarly, using topical drops at the conclusion of the case without ointment will maintain the patient’s visual clarity. If an adjustable suture is planned, using a sterile patch at the conclusion of the case protects the corneal surface and keeps the suture ends contained until the adjustment is performed. If a sliding noose technique is used, the suture ends are tucked under the conjunctiva until the adjustment is performed.
Lost or Slipped Muscle51,52
A lost muscle is identified when the action of an operated muscle has lost the ability to move past midline in the direction of action of the muscle. It is characterized by a complete loss of contact between the muscle and its capsule to the sclera. At times the muscle can be located by dissecting along adjacent connective tissue attachments. Once a muscle is lost, significant effort is needed to try to recover the muscle and reattach it to the eye in a location that will result in acceptable postoperative alignment. If it is not possible to recover the lost muscle, correction of alignment will need to include a transposition procedure. If a total transposition is planned, this would usually be at a later date to reduce the risk of anterior segment ischemia, although a ciliary artery-sparing procedure such as a Hummelheim or Jensen could be done on the same day.
A slipped muscle is caused by the attachment of the capsule around the muscle to sclera with retraction of the muscle posteriorly. Slipped muscles can often be found by dissecting posteriorly along the capsule. It is important to identify muscle tissue and to get solid, locked passes through this muscle to prevent a recurrence of the slippage.
Pulled-in-Two Syndrome (PITS)52
The pulled-in-two syndrome is a complication of strabismus surgery in which there is a rupture of an extraocular muscle. It can result in a lost muscle if not grasped quickly. The most commonly affected muscles are the medial rectus and the inferior rectus. Predisposing factors include age over 50, previous ocular surgery of any type, thyroid disease, and ocular trauma. When this occurs, early recognition of the tear in the muscle is necessary to take the needed steps to prevent the muscle from being lost. Releasing tension on the muscle is essential, followed by the use of locking forceps or a clamp to hold onto as much of the muscle belly as possible. A double-armed suture is then placed through a thicker, more posterior portion of the muscle belly with release of the clamp or forceps. It is important to account for the resection effect of this posterior placement in the final placement of the muscle on the globe. For instance, if the posterior placement is estimated to be 3 mm posterior to the original insertion, the surgeon must increase the recession of that muscle by 3 mm or decrease the resection by 3 mm. If the muscle is lost, a transposition surgery may be performed at a later date to decrease the risk of anterior segment ischemia.53
Postoperative Considerations
Early
Antibiotics
There is debate regarding the benefit to patients from postoperative topical antibiotic and steroid drops. Topical antibiotics containing neomycin are associated with a high rate of allergic sensitivity and are best avoided or used for short duration. Two studies did not show any benefit to treatment beyond a single dose of antibiotic steroid ointment or povidone-iodine immediately after the surgery for uncomplicated fornix based strabismus surgery.54,55 After reoperations or limbus-based surgery, however, a higher incidence of infections was found, therefore postoperative antibiotic-steroid drops were recommended.
Pain
Immediately after strabismus surgery, patients are at risk for ocular pain that should respond to acetaminophen but may require stronger medication.54,55
After reviewing medication allergies, acetaminophen with codeine or hydrocodone, or oxycodone with or without acetaminophen may be helpful for the day of surgery and possibly for sleeping the next evening, especially if the procedure was long or complicated, or if orbital fat had to be resected or cauterized. Inferior oblique surgery tends to be more uncomfortable (and often induces more postoperative nausea—see below). A perioperative bundle of acetaminophen, corticosteroid, ketorolac, a long-acting opioid, and ondansetron has been shown to decrease moderate to severe postoperative pain by 50%. Furthermore, sub-Tenon injection of bupivacaine during strabismus surgery has also been shown to reduce postoperative pain.56
For greater comfort following strabismus surgery, burying the knots of conjunctival sutures will prevent irritation from the loose ends of the suture or the knot itself. The surgeon should start the suture pass on the inside of the proximal half of the incision, then pass through the outside of the distal half of the incision. Next, the surgeoun should tie a surgeon’s knot. This knot will be buried under the conjunctiva. Leaving the suture ends a bit longer is also helpful, so if it is not possible to bury the suture ends, they will lay flat instead of poking directly outward into the eyelids, which can be a painful nuisance for the patient. Some surgeons avoid knots altogether by leaving the incision open or by using cautery to seal the conjunctival edges together.
A preoperative discussion of the patient’s pain tolerance and potential need for a stronger medication can relieve anxiety and postoperative pain. Each patient has a unique pain tolerance, so the surgeon should be flexible and err on the side of keeping postoperative patients comfortable. If they are unable to tolerate narcotics, then an alternative anti-inflammatory medication such as ibuprofen can be offered. Most children do not require narcotics following strabismus surgery, but older children, teens, and adults may benefit from a limited prescription for use as needed following strabismus surgery.
Postoperative nausea and vomiting57
Postoperative nausea and vomiting was reported to occur at a low rate for adults who had general anesthesia. When present, there was a delay to discharge from the postoperative recovery room. The rate of nausea and vomiting was somewhat higher for longer surgical cases, however. Early postoperative nausea and vomiting can be prevented by pre-treating during surgery with perioperative administration of acetaminophen, ketorolac, intravenous corticosteroid, and ondansetron.58
Additional use of ondansetron in the postoperative course can be helpful. Patients undergoing inferior oblique surgery are at a higher risk of postoperative nausea and vomiting and should be pre-treated every time. Subtenon injection of bupivacaine at the end of the case has been shown to decrease postoperative pain, which may also be helpful in reducing the incidence of postoperative nausea, and can decrease the need for short-acting narcotics in the recovery room, which are known to cause nausea and vomiting in some patients.59
Corneal abrasion and dellen
Despite all attempts to protect the cornea from drying during a surgery, if a corneal abrasion occurs from exposure, this can be treated with antibiotic drops and monitoring until it has healed.
Dellen are a focal thinning of the limbal cornea due to a tear film that incompletely coats the cornea surface, with secondary drying of the cornea. There is a risk of the thinning progressing to corneal rupture. In a study using limbus-based incisions, the risk of dellen formation was greater after a reoperated medial rectus muscle or a transposed medial rectus muscle.60 In all cases in this study, the dellen resolved with a pressure patch. A topical antibiotic-steroid combination may alternatively be used to reduce inflammation and prevent infection, with close follow-up to evaluate for thinning of the cornea.
Infection
The symptoms of infection are eye pain, discharge, edema, and decreased vision, and the patients usually present between 1 and 7 days after surgery.61 Initial management with oral broad-spectrum antibiotics such as amoxicillin/clavulanate or cephalexin is recommended if the infection is thought to be preseptal. If pain with ocular motility occurs in conjunction with eyelid edema, an immediate CT or MRI scan of the orbits is indicated to evaluate for orbital cellulitis or an abscess. For orbital involvement, admission for IV antibiotics is important. For an abscess, immediate incision and drainage may be warranted. Possible predisposing factors include age under 18 years, developmental delay, eye rubbing, sinus infection, and poor hygiene.62,63 Endophthalmitis is very unusual, reported to occur in 1 in 30,00 cases,35,64 with potentially devastating consequences, necessitating immediate treatment by a retina surgeon.
Diplopia65,66
Postoperative diplopia is very common in the first week following strabismus surgery, and fortunately resolves for most patients as edema reduces and the brain adapts to the new alignment. Diplopia may be prolonged in the setting of over- or undercorrections. Should the diplopia persist, it can be managed with occlusion, prisms, binocular/dichoptic therapy, amblyoposcope, synoptophore, dichoptic video games, or monocular fixation in the binocular field (MFBF) therapy. Ultimately, another strabismus surgery may be needed to manage this diplopia.
It can also occur in the setting of anomalous binocular function, as seen in anomalous retinal correspondence (ARC), horror fusionalis and central fusion disruption, in which the diplopia is intractable. ARC is caused by the development of a crude binocularity that develops in long-standing and usually large-angle strabismus. When the alignment is corrected, diplopia results. Another form of anomalous binocularity occurs in horror fusionalis, which can develop in patients with congenital strabismus, and in patients with central fusion disruption that is acquired from closed-head trauma and brainstem hemorrhage. Pre-testing with Bagolini lenses and prisms to determine the angle of ARC can help the surgeon plan for proper surgical amount to avoid this very unpleasant complication.
The preoperative assessment is essential and certain characteristics are predictors of postoperative diplopia including monovision, prolonged uncorrected aphakia, aniseikonia, brainstem injury, and retinal distortion. If a patient is unable to fuse with prisms preoperatively, there is an increased risk of postoperative diplopia. Preoperative assessment should involve tests for ARC including after-image testing, Bagolini lens tests, and synoptophore testing. If a patient has intractable postoperative diplopia they may get relief with optical blur, but may also need a black patch or dark contact lens to completely occlude the second image. On the other hand, if the patient has single binocular vision with prismatic correction preoperatively, there is a good chance they will not have postoperative diplopia.
Delayed
Anterior segment ischemia
Anterior segment ischemia is a risk factor for strabismus surgery performed in patients with vascular disease (Table 4) or on multiple rectus muscles. It is caused by interruption of the anterior ciliary vessels that travel though the rectus muscles to supply blood to the anterior segment structures, such as the episcleral limbus, the ciliary body, and the iris. One anterior ciliary artery supplies the lateral rectus and 2 supply each of the other extraocular muscles.67 The clinical signs of ischemia range from pupillary irregularity, to uveitis and corneal haze, to hypotony, to striate keratopathy, to cataract, and even to phthisis bulbi if untreated.68 Clinically the signs are more likely to occur after surgery on 3 or more rectus muscles.69 In addition, surgery on vertical rectus muscles presents a higher risk of developing anterior segment ischemia.70
Table 4. Vascular risk factors for anterior segment ischemia
|
Carotid-cavernous fistula
|
|
Carotid artery obstruction
|
|
Ophthalmic artery obstruction
|
|
Leukemia
|
|
Sickle cell disease
|
Studies looking at iris fluorescein angiography in patients with light-colored irides have identified decreased iris perfusion after strabismus surgery.69 Similarly, the resultant decrease of perfusion has been identified by ICG angiography of the iris in patients with brown irides.70 More recently, OCT-A has been used to evaluate iris vessel perfusion pre- and postoperatively, with similar findings.71 Plications can reduce the effect on iris vessel filling postoperatively when compared to resections, and may allow surgery on a third rectus muscle with less risk of developing anterior segment ischemia. Alternatively, botulinum toxin A on a third rectus muscle is another option to add to the planning of strabismus cases and decrease the chance of inducing anterior segment ischemia. Another alternative is to use a ciliary vessel-sparing technique,71,72 or to use fornix-based incisions to preserve perilimbal episcleral vessels.73
Suture granulomas present as a solid erythematous mass lesion in the area of previous strabismus surgery, adjacent to the suture holding the muscle. They are not painful, and they may or may not be cosmetically disfiguring. Non-absorbable sutures are typically used in reports of granulomas occurring after strabismus surgery.74,75 Not all respond well to steroid medications and may need to be resected.
Refractive changes
There may be a transient refractive shift after strabismus surgery on 2 horizontal rectus muscles, either bilateral or unilateral. In addition to myopia, astigmatic changes have been observed. These changes tend to resolve after several weeks to the preoperative refraction. Permanent changes to refraction may also occur and can be addressed with a change to glasses and/or contact lenses once the patient has healed. It is important to have a discussion with the patient or parent preoperatively, particularly if the patient does not require refractive correction, about the potential change in vision postoperatively.
Conjunctival inclusion cyst
A conjunctival inclusion cyst arises from inadvertent suturing of the conjunctival epithelium into the incision site. The cysts tend to develop several days to weeks after surgery and appear as a clear cystic structure. In-office puncture with massage can resolve these, although it is common to need to repeat the procedure multiple times until the cyst walls seal together. Patients in whom the puncture does not resolve, as well as children who are not able to safely tolerate the needle puncture in office, will benefit from surgical excision. Cyst excision in the operating room is best accomplished by injecting trypan blue into the cyst with a 30 or higher gauge needle to stain the cyst wall. Using this technique, the entire wall of the cyst can be removed with Westcott scissors and .12 or similar forceps to eliminate recurrence, a possible consequence if the surgeon does not remove all the conjunctival epithelium making up the cyst wall.76
Long-Term
Conjunctival or suture granuloma
A granuloma is a lobular capillary hemangioma that develops at the site of the conjunctival closure or where the muscle is sutured to the globe. Granulomas are distinguished from conjunctival cysts by their red-yellow, fleshy appearance, and rapid growth. The granuloma may respond to topical steroid drops with a reduction in growth and size, but it is rare for the steroid to fully resolve the lesion. Some may resolve over a prolonged period of time (many months to years). For those where the growth does not resolve, surgical excision can be considered. The granuloma is often fused with the overlying conjunctiva, particularly if the lesion is many months old or older. An attempt to dissect the conjunctiva off the lesion prior to removal should be made to preserve conjunctiva and prevent symblepharon formation (see below). If this is not possible, it may be necessary to excise the conjunctiva and employ one of the closure methods discussed in the next section on conjunctival scarring, below.77
Conjunctival scarring/symblepharon78,79
Strabismus can result from previous ocular surgeries from which there was scarring of the conjunctiva and consequent limitation of motility. Simply removing the scar tissue is not always effective, because the scar tissue tends to recur. Particularly in adults, whose conjunctiva is no longer elastic, it is important to pay attention to the conjunctival closure to make sure that the sutured conjunctiva is not inducing a restriction to gaze. If forced duction results in gaping or tension on the suture sites, the wound is too tight. Options at this point include leaving the conjunctiva open to heal by secondary intent, amniotic membrane graft, and conjunctival autograft. Healing by secondary intent is acceptable unless the muscle insertion and suture will be exposed. This increases the risk of infection, conjunctival cyst formation, and granuloma around the suture.
An alternative is to use an amniotic membrane to cover the gap in conjunctiva and the surface of the muscle to act as a scaffolding for the conjunctiva to heal over. It has been used to reconstruct a scarred conjunctival fornix as well as to treat symblepharon. These membranes are commonly available at most hospitals, but it is best to ascertain their availability in anticipation of the need (eg, complex adult cases, primary symblepharon repair, multiple reoperations, etc.).
Should amniotic membrane not be available, another alternative is to use a conjunctival autograft from the superior conjunctiva of the same or fellow eye. The superior conjunctiva of most patients has significant laxity and redundancy that a segment of tissue large enough to bridge the gap in the conjunctiva can be carefully excised, leaving the Tenon capsule intact, and placed over the gap. To affix the graft to the adjacent conjunctiva, 9-0 vicryl suture or Tisseal tissue glue can be used. In some cases, the conjunctiva will revascularize, in others it is merely acting as a scaffolding for conjunctival healing.
It is important to discuss these methods with any patient at risk of needing these procedures ahead of time, or immediately after surgery if it was not anticipated, as all 3 methods require a prolonged healing process postoperatively, and the eye will not return to normal appearance for several months following surgery.
Fat adherence syndrome
Marshall Parks first described fat adherence syndrome as occurring after inferior oblique surgery during which the posterior Tenon capsule is violated.80 This is due to the anatomic proximity of the inferior oblique and the Tenon capsule. This condition has also been described following retinal procedures.81 The prolapsing orbital fat scars to muscle or sclera and contracts, leading to a restrictive strabismus. It can be very hard to eliminate. One solution has been to place amniotic membrane grafts to separate the fat tissue from the muscle, and it is also placed on bare sclera to provide a barrier to exposed sclera. This complication is less likely to occur in surgery in which the inferior oblique is isolated under direct visualization, and where care is taken to not perforate the orbital septum during the procedure.
Dealing with fat adherence syndrome during subsequent strabismus surgery requires patience and meticulous attention to detail. The fibrofatty scar needs to be dissected off the muscle belly carefully, as there is almost always fibrofatty infiltration of the muscle belly itself by the process. Then, orbital fat and the fibrofatty scar need to be excised, and cauterized. Orbital fat is highly vascular and leads to postoperative bleeding (ecchymosis) and inflammation. Amniotic membrane and/or local corticosteroid (eg, triamcinolone) can be used to help prevent recurrence. The surgeon should attempt to limit any possible contact with intact yellow fat by the muscle or the globe prior to closing the conjunctiva. Orbital fat is an essential component of ocular protection in our orbit, and also can affect the cosmetic appearance of the skin postoperatively, so only as much fat as necessary should be removed or cauterized. Attention to postoperative pain management is critical, as these cases are often quite painful (see discussion above).82,83
Eyelid position change
Managing the palpebral fissure height is important to maintain cosmesis while performing strabismus surgery. Surgical recession of the inferior rectus for restrictive myopathy such as can occur in thyroid myopathy, orbital fibrosis, and after an inferior orbital wall fracture, can result in eyelid retraction. Any surgery on the superior or inferior rectus is at risk for an eyelid position change, although this complication is more common with surgery on the inferior rectus. It is important to separate the eyelid retractors from the eyelid during the surgical procedure to avoid this complication.84
Summary
Overall, strabismus surgery in adults can provide the benefits of improved function with an expanded field of single binocular vision. The enhanced binocular function can aid in balance, safety of mobility, and independence in daily life by restoring the freedom to drive. Resolution of strabismus can improve the patient’s sense of well-being and decrease social stress by enhancing self-esteem. Improving alignment can allow patients to return to gainful employment in a safer and more productive manner.
This must be balanced by the number of reoperations that are seen in adults, making those more complicated surgeries on the whole, with an increased likelihood of scarring encountered during surgeries and with more friable tissue compared to the healthy tissue encountered in children. As long as the preoperative assessment is thorough, and the risks and benefits are clearly outlined to manage expectations, there can be a successful outcome in many patients.
References
- Astle AT, Foulsham T, Foss AJ, McGraw PV. Is the frequency of adult strabismus surgery increasing? Ophthalmic Physiol Opti. 2016 (36):487-493.
- Pineles SL, Repka MX, Yu F, Lum F, Coleman AL. Risk of musculoskeletal injuries, fractures, and falls in Medicare beneficiaries with disorders of binocular vision. JAMA Ophthalmol. 2015 Jan;133(1):60-65.
- Baker, John D. The value of adult strabismus correction to the patient. J AAPOS. 2002; 6 (3):136-140.
- Beauchamp GR, Black BC, Coats DK, et al. The management of strabismus in adults- I. clinical characteristics and treatment. J AAPOS; 7 (4):233-240.
- Beauchamp GR, Black BC, Coats DK, et al. The management of strabismus in adults-II. Patient and provider perspectives on the severity of adult strabismus and outcome contributors. J AAPOS. 2005; 9 (2):141-147.
- Beauchamp GR; Black BC; Coats DK, et al. The management of strabismus in adults—III. The effects on disability. J AAPOS. 2005 Oct; 9 (5):455-459.
- Black BC, Felius J Beauchamp GR. Intensity and complexity index of disease for strabismus surgery. J AAPOS. 2003; 7 (1):60-65.
- Burden Jr AL. The stigma of strabismus: An ophthalmologist’s perspective. Arch 1994; 112:302.
- Burke JP, Leach CM, Davis H. Psychosocial implications of strabismus surgery in J Pediatr Ophthalmol Strabismus. 1997; 34:159-164.
- Coats DK, Paysee EA, Towler AJ, Dipboye RL. Impact of large angle horizontal strabismus on ability to obtain employment. Ophthalmology. 2000; 107:402-405.
- Helveston EM. The value of strabismus surgery. Ophthalmic Surg. 1990; 21:311-317.
- Jackson S, Harrad RA, Morris M, Rumsey N. The psychosocial benefits of corrective surgery for adults with strabismus. Br J Ophthalmol. 2006; 90:883-888.
- Keltner JL. Strabismus surgery in adults: functional and psychosocial implications. Arch Ophthalmol. 1993; 112:599-600.
- Kraft, SP. Adult strabismus surgery: more than just cosmetic/La chirurgie du strabisme adulte: bien au-dela’ de l’ Can J Ophthalmol. 2008; Feb; 43(1):9-12.
- Menon V, Saha J, Tandon R, Mehta M, Khokhar S. Study of the psychosocial aspects of J Pediatr Ophthalmol Strabismus. 2002;39:203-208.
- Metz HS. Strabismus surgery is reconstructive surgery. J Ped Ophthalmol 1988; 25:263.
- Mojon-Azzi SM, Mojon DS. Opinion of headhunters about the ability of strabismic subjects to obtain employment. Ophthalmologica. 2007; 221 (6):430-433.
- Olitsky, SE, Sudesh S, Graziano A, Hamblen J, Brooks SE, Shaha SH. The negative psychosocial impact of strabismus in adults. J AAPOS. 1999; 3:209-211.
- Rosenbaum AL. The goal of strabismus surgery is not cosmetic. Arch Ophthalmol. 1999; 117:250.
- Young BK, Verter E, Howard MA. 2019 AAPOS Annual Meeting: Quality Analysis of Publicly Available Videos for Pediatric Strabismus Surgery, poster
- Edward G. Buckley. General Principles in the Surgical Treatment of Paralytic Strabismus. In Pediatric Ophthalmology, Current Thought and a Practical Guide, Wilson, ME, Saunders RA, Trivedi RH Editors, Springer. 2009.
- Grace SF, Cavuoto KM, Shi W, Capo H. Surgical Treatment of Adult-Onset Esotropia: Characteristics and Outcomes. J Pediatr Ophthalmol Strabismus. 2017 Mar 1;54(2):104-111.
- Nihalani BR, Hunter DG. Adjustable suture strabismus surgery.Eye (Lond). 2011 Oct;25(10):1262-76. doi: 10.1038/eye.2011.167. Epub 2011 Jul 15. PMID: 21760626; PMCID: PMC3194320.
- Molarte AB, Rosenbaum AL. Vertical rectus muscle transposition surgery for Duane syndrome. J Pediatr Ophthalmol Strabismus. 1990; 27:171-177.
- Velez FG, Pineles SL. Adjustable posterior fixation suture technique in adjustable superior rectus transposition. J Binocul Vis Ocul Motil. 2018 Oct-Dec;68(4):154-155.
- Baker L, Mackenzie K, Adams GG, Hancox J. Long-term surgical outcomes for vertical deviations in thyroid eye disease. Strabismus. 2017 Jun;25(2):67-72.
- Peragallo JH, Velez FG, Demer JL, Pineles SL. Postoperative drift in patients with thyroid ophthalmopathy undergoing unilateral inferior rectus muscle recession. Strabismus. 2013 Mar;21(1):23-28.
- Modabber M, Dan AF, Coussa RG, Flanders M. Retrobulbar anaesthesia for adjustable strabismus surgery in adults: a prospective observational study. Can J Ophthalmol. 2018 Dec;53(6):621-626.
- Scott AB, Kraft SP. Botulinum toxin injection in the management of lateral rectus paresis. Ophthalmology. 1985 May;92(5):676-683.
- Holmes JM, Beck RW, Kip KE, Droste PJ, Leske DA. Botulinum toxin treatment versus conservative management in acute traumatic sixth nerve palsy or paresis. J AAPOS. 2000 June; 4(3):145-149.
- Holmes JM, Leske DA. Long-term outcomes after surgical management of chronic sixth nerve palsy. J AAPOS. 2002;6(5):283–288.
- Owens PL, Strominger MB, Rubin PA, Veronneau-Troutman S. Large-angle exotropia corrected by intraoperative botulinum toxin A and monocular recession resection surgery. J AAPOS. 1998; 2(3)144-146.
- Tuğcu B, Sönmezay E, Nuhoğlu F, Özdemir H,,,Özkan . Botulinum toxin as an adjunct to monocular recession-resection surgery for large-angle sensory strabismus. J AAPOS. 2017; 21(2)117-120.
- Koederitz NM, Neely DE, Plager DA et al. Postoperative povidone-iodine prophylaxis in strabismus surgery. J AAPOS. 2008; 12(4):396-400.
- Ing MR, Shortell J, Golez, J. Extraocular and intraocular infections following strabismus surgery: A review. J Pediatr Ophthalmol Strabismus. 2019; 56(4):214-221.
- Kivlin JD, Wilson Jr ME. Periocular Infection Study Group. Periocular infection after strabismus surgery. J Pediatr Ophthalmol Strabismus. 1995; 32:42-49.
- Rogers DL, Chheda L, Ford C, et al. The effect of surgical preparation technique on the bacterial load of surgical needles and suture material used during strabismus surgery. J AAPOS. 2011;15:230-233.
- Eustis HS, Rhodes A. Suture contamination in strabismus surgery. J Pediatr Ophthalmol Strabismus. 2012 Jul-Aug;49(4):206-209. doi: 10.3928/01913913-20110920-01.
- Benson CE, Rogers KL, Suh DW. Dual application versus single application of povidone-iodine in reducing surgical site contamination during strabismus surgery. J AAPOS. 2014; 18:347-350.
- Waldschmidt B, Gordon N. Anesthesia for pediatric ophthalmologic surgery. J AAPOS. 2019 Jun;23(3):127-131. doi: 10.1016/j.jaapos.2018.10.017. Epub 2019 Apr 14.
- Simon JW, Lininger LL, Scheraga JL. Recognized scleral perforation during eye muscle surgery: Incidence and sequelae. J Pediatr Ophthalmol Strabismus. 1992; 29: 273-275.
- Capo H, Repka MX, Guyton DL Hang-back lateral rectus recessions for exotropia.J Pediatr Ophthalmol Strabismus. 1989; 26:31-34.
- Rodrigues AC, Nelson LB. Long-term results of hang-back lateral rectus recession. J Pediatr Ophthalmol Strabismus. 2006 May-Jun;43(3):161-164. doi: 10.3928/01913913-20060301-04.
- Schönfeld S, Heede S, Salchow DJ. Ophthalmologe. [Comparison of hang-back recession and conventional recession for correction of exotropia] [Article in German]. 2016 May;113(5):402-408. doi: 10.1007/s00347-015-0154-z.
- Orlin A, Mills M, Ying G-S, Liu C. A comparison of hang-back with conventional recession surgery for exotropia. J AAPOS. 2007; 11:597-600.
- Rajavi Z, Ghadim HM, Nikkhoo M, Dehsarvi B. Comparison of hang-back and conventional recession surgery for horizontal strabismus. J Pediatr Ophthalmol Strabismus, 2001; 38:273-277.
- Mills PV, Hyper TJ, Duff GR. Loop recession of the recti muscles. Eye (Lond). 1987; 1:593-596.
- Schnall BM. Feingold AB. Infection following strabismus surgery. Curr Opin Ophthalmol. 2018; 29(5):407-411. doi: 10.1097/ICU.0000000000000507)
- Walton RC, Cohen AS. Staphylococcus epidermidis endophthalmitis following strabismus surgery. J AAPOS 2004; 8 (6):592-593.
- Benson CE, Rogers KL, Suh DW. Dual application versus single application of povidone-iodine in reducing surgical site contamination during strabismus surgery. J AAPOS. 2014; 18:347-350.
- Wan MJ, Hunter DG. Complications of Strabismus Surgery: Incidence and Risk Factors. Semin Ophthalmol. 2014; 29 *:421-428.
- Bradbury JA, Taylor RH. Severe complications of strabismus surgery. J AAPOS. 2013;17(1):59–63.
- Ellis EM, Kinori M, Robbins SL, Granet DB. Pulled-in-two syndrome: a multicenter survey of risk factors, management and outcomes. J AAPOS. 2016 Oct;20(5):387-391. doi: 10.1016/j.jaapos.2016.06.004. Epub 2016 Sep 16.
- Elkamshoushy AA, Soni A, Alsanousy A. A randomized controlled trial comparing the efficacy of topical antibiotic steroid combination versus no treatment after fornix-incision strabismus surgery. J AAPOS. 2018; 22 (5):344-347.
- Koederitz NM, Neely DE, Plager DA. Postoperative povidone-iodine prophylaxis in strabismus surgery. J AAPOS. 2008; 12(4):396-400.
- Enyedi LB, Wallace DK, Dear GdeL. A double-masked randomized trial of postoperative local anesthetic for pain control in pediatric strabismus surgery. J AAPOS. 2017 Apr;21(2):107-111. doi: 10.1016/j.jaapos.2017.03.005. Epub 2017 Mar 10.
- Kratt KM, Bothun ED, Kruthiventi SC, Portner ER, Sprung J, Weingarten TN. Postoperative nausea and vomiting and phase I post-anesthesia recovery after strabismus operations. J Pediatr Ophthalmol Strabismus. 2019; May 22;56(3):151-156. doi: 10.3928/01913913-20190208-03.
- Ali U, Tsang M, Igbeyi B, et al.A 4year quality improvement initiative reducing post-operative nausea and vomiting in children undergoing strabismus surgery at a quaternary paediatric hospital. Paediatr Anaesth. 2019 Jul;29(7):690-697. doi: 10.1111/pan.13664. Epub 2019 Jun 2.
- Raffa RB, Colucci R, Pergolizzi JV. The effects of food on opioid-induced nausea and vomiting and pharmacological parameters: a systematic review. Postgrad Med. 2017 Sep;129(7):698-708. doi: 10.1080/00325481.2017.1345282. Epub 2017 Jul 14.
- Frangouli O, Adams GG The use of amniotic membrane for the management of fibrosis in complex strabismus surgery. Strabismus. 2013 Mar;21(1):13-22.
- Mills MD, Coats DK, Donahue SP, Wheeler DT. Strabismus surgery for adults: a report by the American Academy of Ophthalmology. Ophthalmology. 2004; 111:1255-1262.
- Koederitz NM, Neely DF, Plager DA, et al. Postoperative povidone-iodine prophylaxis in strabismus surgery. J AAPOS 2008; 12:396-400.
- Zloto O, Mezer E, Ospina L, Stankovic B, Wygnanski-Jaffe T. Endophthalmitis following strabismus surgery: IPOSC global study. Curr Eye Res. 2017 Dec;42(12):1719-1724.
- Ing MR. Infection following strabismus surgery. Ophthalmic Surg. 1991; 22:41-43.
- Sharma M, Hunter DG. Diplopia after strabismus surgery. Semin Ophthalmol. 2018; 33:102-107.
- Reddy SK, Salgado CM, Hunter DG. Central fusion disruption following irradiation of neoplasm in pineal gland. Arch Ophthalmol. 2009;127(3):337–338.
- Basic and Clinical Science Course, Section 6, Pediatric Ophthalmology and Strabismus, 2014-2015:24.
- Saunders RA, Bluestein EC, Wilson ME, Berland JE. Anterior segment ischemia after strabismus surgery. Surv Ophthalmol. 1994; 38(5): 456–466.
- Olver JM, Lee JP. The effects of strabismus surgery on anterior segment circulation. Eye (Lond). 1989; 318–326.
- Chan TK, Rosenbaum AL, Rao R, Schwartz SD, Santiago P, Thayer D. Indocyanine green angiography of the anterior segment in patients undergoing strabismus surgery. Br J Ophthalmol. 2001; 85(2): 214–218.
- Pineles SL, Chang MY, Oltra EL, Pihlblad MS, Davila-Gonzalez JP, Sauer TC, Velez FG. Eye (Lond). 2018 Feb;32(2):173-178.
- McKeown CA. Anterior ciliary vessel sparing procedure In: Rosenbaum AL, Santiago P, eds. Clinical Strabismus Management. Philadelphia: W.B. Saunders Company, 1999: 516–526.
- Mojon DS. Comparison of a new, minimally invasive strabismus surgery technique with the usual limbal approach for rectus muscle recession and plication. Br J Ophthalmol. 2007 Jan; 91(1):76-82.
- Somsen D, Heidary G. Rapid onset of orbital cellulitis after uncomplicated strabismus surgery, J AAPOS. 2019; 23(5):290-291.
- House RJ Rotruck JC, Enyedi LB, Wallace DK, Saleh E, Freedman SF. Postoperative infection following strabismus surgery: case series and increased incidence in a single referral center. J AAPOS. 2019; 23(1):26.e1-26.e7.
- El-Abedin Rajaba GZ, Demer JL. Long-term results of surgical excision of conjunctival retention cyst using trypan blue with methylcellulose. Am J Ophthalmol Case Rep. 2019 Jun; 14: 28–31. Published online 2019 Feb 6. doi:1016/j.ajoc.2019.01.010 PMCID: PMC6377388 PMID: 30815620.
- Olitsky SE, Coats DK. Complications of Strabismus Surgery. Middle East Afr J Ophthalmol. 2015 Jul-Sep; 22(3): 271–278. doi:4103/0974-9233.159692 PMCID: PMC4502168 PMID: 26180463.
- Strube YNJ, Conte F, Faria C, Yiu S, Wright KW. Amniotic Membrane Transplantation for Restrictive Strabismus. Ophthalmology. 2011; 118:1175–1179.
- Parks, MM. Causes of the adhesive syndrome. Symposium on Strabismus. Trans New Orleans Acad Ophthalmol. Mosby, St. Louis, MO. 1978; 26:269-279.
- Parks MM. Inferior oblique weakening procedures. Int Ophthalmol Clin. 1985; 25: 107-117.
- Wright KW. The fat adherence syndrome and strabismus after retina surgery. 1986; 93(3):411-415.
- Özkan SB. Restrictive problems related to strabismus surgery. Taiwan J Ophthalmol. 2016 Jul-Sep; 6(3):102–107. Published online 2016 Jun 20. doi:1016/j.tjo.2016.05.001 PMCID: PMC5525619. PMID: 29018723.
- Kerr Fat adherence syndrome: An animal model. J AAPOS. 2004; 8(4):349-356. DOI:https://doi.org/10.1016/j.jaapos.2004.04.005.
- Fresina M, Campos EC. Corneal ‘dellen’ as a complication of strabismus surgery. Eye (Lond). 2009; 23:161-163.