The links to each individual chapter of the Color Atlas of Gonioscopy are available at the Chapters link, below.
Both laser and incisional surgery are performed with the aid of gonioscopic visualization of the angle. Incisional surgery includes goniotomy, goniosynechialysis, internally created filtration procedures, and internal revisions of filtration fistulas. Such procedures are performed by only a small proportion of ophthalmologists and generally fall outside the scope of this atlas. Goniotomy is briefly discussed in Chapter 7. Gonioscopic lenses are used more often for laser surgery than for incisional surgery. The most common gonioscopic laser procedures are trabeculoplasty and iridoplasty. These procedures will be discussed in some detail. Transpupillary cyclophotocoagulation of the ciliary body is also performed gonioscopically, but it has limited effectiveness and is rarely used. Various forms of ab interno laser fistulas and laser lysis of synechiae have been described as well as new devices for ab interno incisional surgery are being evaluated for their utility in treating various forms of glaucoma. These procedures have not reached general use and are not discussed.
Argon and Selective Laser Trabeculoplasty
Argon and selective laser trabeculoplasty are the most frequently performed procedures for glaucoma.
Argon laser trabeculoplasty
Argon laser trabeculoplasty (ALT) successfully lowers intraocular pressure in about 80% of patients with primary open-angle glaucoma (Thomas et al, 1982). The effect on intraocular pressure is proportional to that before treatment (Thomas et al, 1982; Wise and Witter, 1979). ALT is efficacious in treating primary open-angle glaucoma and some secondary open-angle glaucomas, such as those associated with pseudoexfoliation and the pigment dispersion syndrome. It is less successful in patients with infantile glaucoma, angle recession, inflammatory glaucoma, and aphakia and in young patients (Thomas et al, 1982; Wise and Witter, 1979).
A Goldmann three-mirror lens is usually used for ALT. The lens should have an antireflective coating to allow maximum delivery of the laser energy to the angle. Some ophthalmologists prefer to use the Ritch lens, which has magnifying “buttons” to focus the laser energy on to a smaller area. The Ritch lens (see 3-19) also has mirrors that are designed specifically for the superior and inferior angles (Ritch, 1985).
An understanding of the anatomy of the angle is a critical requirement for performing ALT. The burns are applied at the junction of the pigmented and nonpigmented trabecular meshwork (10‑1). Delivery of laser energy too far posteriorly results in increased inflammation and an increased number of peripheral anterior synechiae (Rouhiainen et al, 1988) (see 8‑52 and 8‑53). Laser energy delivered too far anteriorly may result in overgrowth of the trabecular meshwork by corneal endothelium (Rodrigues et al, 1982). The techniques described in Chapter 4 can be used to help define the anatomy. If the angle is confusing, one should look inferiorly at the deepest and most pigmented portion of the angle to become oriented to the patient’s anatomy. The corneal wedge can be invaluable in determining the location of Schwalbe’s line. In patients on cholinergics with steep approaches to the angle, dilation can be used to improve the visibility of the angle. In patients with a poor view of the angle secondary to pupillary block, one may need to perform a peripheral iridotomy with a laser. In eyes with plateau iris configuration and in other cases where the angle is crowded, it may be helpful to perform iridoplasty before carrying out trabeculoplasty.
It can be difficult to maintain one’s bearings while performing ALT because of the mirrored view of the angle. If a long series of laser spots is delivered and the lens is then rotated for a second series of spots, it is easy to become lost unless there are visible angle landmarks such as iris processes, nevi, or distinct laser burns. One can hold the Goldmann lens with three fingers (see 4‑8) and rotate the lens slightly after every few applications, keeping the area undergoing treatment near the center of the mirror.
A 50-μm spot of argon—green light is normally used. The duration of delivery is 0.1 s. The power required varies from 200 to 1200 mW and is adjusted until an adequate uptake of energy is noted. In an angle with average pigmentation one should generally start with approximately 700 mW. In a darkly pigmented angle, as found in cases of pseudoexfoliation and pigmentary glaucoma, one should start at a lower energy, approximately 300 mW. In extremely lightly pigmented angles, no visible uptake of laser energy may be apparent despite a power level of 1200 mW. An adequate response to treatment is signified by blanching or the formation of small bubbles in the trabecular meshwork (10‑1). If a crater, a large bubble, or a shower of bubbles forms, the intensity is too high. The use of power levels greater than 1000 to 1200 mW is not recommended. A therapeutic effect may result from treatment at this power level, even if no visible angle changes occur.

10-1 Burns induced by argon-laser trabeculoplasty. The burns are placed at the junction of the pigmented and nonpigmented portions of the trabecular meshwork. The end-point is a blanching of the meshwork (left) or a small bubble (second from left). A large bubble (second from right) or a shower of bubbles (right) indicates that excessive laser energy is being applied. A similar small shower of bubbles may appear during selective laser trabeculoplasty, but without blanching of the meshwork.
It is important to have the burn strike the trabecular meshwork perpendicularly. When properly aligned, a crisp round spot will be formed by the aiming beam. This is easiest to judge if the aiming beam is kept fairly dim. If the spot is distorted or oblong, the Goldmann lens is probably being held at an unusual angle. It is often helpful to look around the slit-lamp oculars and adjust the lens so that the front surface is parallel to the plane of the patient’s face. This should help to give a distinct, round spot. In the case of patients with steep approaches to the trabecular meshwork, who are looking into the mirror in order to allow the physician to treat the meshwork, there will be some distortion of the beam because of the angle of approach. A flatter approach, parallel to the iris, is preferred. Some authors suggest that the patient should be asked to look slightly away from the mirror so that a flat approach into the meshwork can be obtained (Palmberg, 1989). With most patients, however, satisfactory results are obtained if they look straight ahead through the entire procedure. ALT can be performed for any portion of the angle but is typically performed over 180° or 360°. Typically, 40 to 50 laser applications are applied over each 180°.
The most common complication from ALT is postoperative elevation of the intraocular pressure. Apraclonidine has been shown to decrease the number and intensity of pressure spikes markedly after laser trabeculoplasty and is generally administered at the time of the procedure (Robin et al, 1987). Brimonidine is now used routinely in the same way. There should be postoperative monitoring for intraocular pressure spikes at 1 hour after the procedure.
Re-treatment of a previously treated angle has met with varying success. Although some authors have found re-treatment to be safe and efficacious in selected patients (Jorizzo et al, 1988), others have reported an unacceptable number of pressure spikes and a low success rate (Brown et al, 1985).
Selective laser trabeculoplasty
Selective laser trabeculoplasty (SLT) represents a relatively new addition to the treatment options for open-angle glaucoma. Many similarities exist between argon and selective laser trabeculoplasty, including technique, efficacy, and role in the glaucoma treatment algorithm. Nevertheless, numerous differences also exist.
SLT uses a Q-switched, double-frequency, neodymium:yttrium-aluminum-garnet (Nd:YAG) laser (532 nm). This is intended to target pigmented trabecular meshwork while concurrently avoiding thermal injury to the trabecular beams (Latina et al, 1998). SLT does not require that the spot size (400 μm) or duration (3 ns) of the application be adjusted. Unlike ALT, the laser energy does not need to be precisely applied over the trabecular meshwork alone, as long as the trabecular meshwork is covered by the laser application. In angles with confusing anatomy or limited pigmentation, this can be a useful advantage over ALT. These advantages of SLT over ALT are countered by the current requirement that a separate laser unit must be employed to treat with SLT, and many practitioners find this to be cost- or space-prohibitive.
The energy used for SLT is typically between 0.5 to 1.5 mJ per application. It is usually titrated up while watching for a few small bubbles to arise from the trabecular meshwork after each shot (see 10‑1). If a large shower of bubbles occurs, or if pigment is dispersed with the laser application, it should be titrated down. The energy required to see the small bubbles appears to be related to angle pigmentation. SLT can be effective even if no bubbles are seen during the procedure. As with ALT, SLT is performed using a mirrored lens. The Goldmann three-mirror lens works well, as does the Latina SLT lens, which has one mirror. The lens should be rotated frequently enough to keep the view clear and avoid tangential application of the laser to the angle structures. Forty-five applications per 180° is a reasonable number, and both 180° and 360° treatments are routinely performed.
Both prospective and retrospective trials suggest that SLT compares favorably to ALT, although there is not yet data to identify long-term risks or benefits of the procedure (Damji et al, 2006, and Juzych et al, 2004). As with any relatively new procedure, it is important to discuss the lack of long-term follow-up with patients during the consent process. Patients should be treated prophylactically with brimonidine before and after the procedure to avoid a pressure spike. Monitoring of the pressure 1 hour after the procedure is appropriate to identify the small number of patients that do have a pressure elevation after SLT despite pretreatment with brimonidine. Recent evidence suggests that highly pigmented angles may be particularly susceptible to these pressure spikes (Harasymowycz et al, 2005). Other complications are exceedingly rare, including the formation of peripheral anterior synechiae.
Re-treatment with SLT after prior ALT is controversial, although potentially effective (Latina et al, 1998, and Damji et al, 2006). We generally do not recommend repeating the procedure after a history of failed ALT procedures, although the limited side effects make it a safe alternative in patients for whom the remaining options involved incisional surgery. There is not enough evidence to date to discuss the efficacy of re-treatment with SLT after previously successful SLT, although many practitioners currently do this.
Laser Iridoplasty
Laser iridoplasty is used to pull the iris away from the angle. This is done in eyes with plateau iris configuration, when laser trabeculoplasty is difficult due to a crowded angle, and, rarely, in eyes with acute angle closure in which laser iridotomy cannot be performed. Laser iridoplasty can be performed either through a Goldmann three-mirror lens or directly through the cornea without the use of a lens, aiming at the most peripheral iris (10‑2). In either case, iridoplasty is done with large, slowly applied spots of low power. This power is chosen to shrink, not perforate, the iris. Spots of 200 to 500 μm with durations of 0.2 to 0.5 s are used. The power is adjusted until visible shrinkage is noted; this usually requires power settings of 150 to 300 mW.
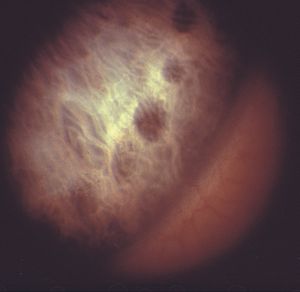
10-2 Scars from argon-laser iridoplasty. The energy was administered through the cornea without a gonioscopic lens in this patient with plateau iris syndrome.