Establishing the diagnosis
A five-year-old girl is referred by her pediatrician because her vision screen revealed decreased visual acuity in the left eye. The child's mother reports that the child is otherwise healthy, was born at full term, and has met all developmental milestones. However, the left eye occasionally appears to turn inward. The child seems to ignore people when they approach her on the left side, and she was previously more likely to cry when her car seat was positioned behind the driver. Further history indicates that, as a baby, she did not feed well when given a bottle, and that she occasionally snores.
On examination she has a slightly wide nasal bridge. Her visual acuity is 20/20 in the right eye and 20/800 in the left eye with LEA symbols. On cover testing she has poor fixation with the left eye but seems to demonstrate a 6 diopter left esotropia. There is a trace left afferent pupillary defect. Following cycloplegia with 2.5 % phenylephrine and 1% cyclopentolate eye drops, her retinoscopy is +0.50 in the right eye and -3.00 + 1.50 × 90 in the left eye. Examination of the fundus reveals a normal-appearing right optic nerve. The left optic nerve is slightly enlarged, with multiple anomalous vessels radiating circumferentially. A tuft of white material obscures the central cup. There is a wide area of peripapillary pigment abnormality, with zones of hyperpigmentation in clumps, and hypopigmentation. The nerve appears to undulate slightly in and out of focus. (Figure 1).
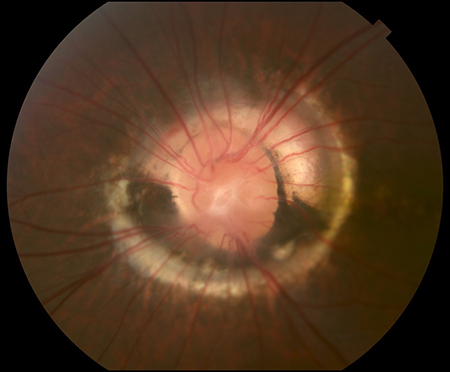
Figure 1. Wide area of peripapillary pigment abnormality, with zones of hyperpigmentation in clumps, and hypopigmentation. On examination, the nerve appears to undulate slightly in and out of focus.
The child is diagnosed with morning glory disc anomaly and her mouth is examined. There appears to be a slight separation of the soft palate, but no cystic mass lesion. The child is prescribed full-time glasses wear to correct the anisometropia and part-time patching of the right eye 2 hours per day. Discussion with her mother includes the diagnosis and the news that, despite the glasses and patching, the overall visual prognosis is poor. A magnetic resonance imaging (MRI) scan of the orbit/sinuses with gadolinium and a magnetic resonance angiogram (MRA) is ordered to exclude a transphenoidal encephalocele and intracranial carotid artery dysgenesis. Her neuroimaging results demonstrate a slight downward displacement of the chiasm into the suprasellar cistern but are otherwise unremarkable. The intracranial vascular system is normal. She is scheduled for a 3-month follow-up visit and is referred to a pediatric otolaryngologist for evaluation of the soft palate.
Morning glory disc anomaly: Clinical features
In 1970 Kindler described an unusual congenital disc anomaly as “morning glory syndrome” because of its resemblance to the morning glory flower.1 It is characterized by an enlarged, funnel-shaped excavation that incorporates the optic disc. The disc itself is enlarged, and orange or pink in color within a surrounding area of peripapillary chorioretinal pigmentary changes. The overall diameter of the disc depends on the size of the excavated posterior scleral opening. Occasionally the disc itself may appear elevated. Within the center of the disc is a white glial tuft. Similar to petals on a flower, the blood vessels are increased in number and curve as they emanate radially from the disc, rather than in the usual central branching pattern. They then straighten, and it is often difficult to distinguish the arteriolar from the venous circulation. There are also small peripapillary arteriovenous communications. Depending on the size of papillary chorioretinal involvement, the macula may be incorporated into the excavation, which is termed “macular capture.”2,3
Morning glory syndrome is typically unilateral with equal involvement of the right and left eyes. Bilaterality of this condition can occur.4 The visual prognosis is usually poor, in the 20/100 to 20/200 range. Serous retinal detachments can occur in 30% of individuals. Although not completely understood, it is postulated that there is a communication between the subarachnoid space within the posterior excavation and the subretinal space.5 Cerebrospinal fluid can then leak subretinally and can extend to a complete retinal detachment. Cases to support this hypothesis include resolution of the serous detachment following optic nerve sheath fenestration, and demonstration of a gas bubble in the subarachnoid space following vitrectomy with gas injection and optic nerve sheath fenestration. Contractile movements within the morning glory disc anomaly, leading to an opening and closing of the central cup that corresponds to pulse pressure, can also be seen.6
Etiology
Morning glory disc anomaly may be part of other systemic abnormalities and syndromes, although it does not appear to be a specific genetic disorder. Most established is the finding of a transphenoidal basal encephalocele and midfacial malformations.7 Transphenoidal encephalocele is an out-pouching of the meningeal sac through a defect in the sphenoid bone, and it often contains the optic chiasm and hypothalamus. Sometimes there is a midline cleft in the soft palate with visualization of intraoral extension of the encephalocele. Typically, individuals with these findings also have a wide head, depressed nasal bridge, and mid upper lip defect or cleft. When the meningocele protrudes into the nasopharynx, it can impair breathing, leading secondarily to nasal obstruction with subsequent mouth breathing and snoring. Rhinorrhea has also been described, as well as the dire consequences of surgical biopsy or removal of a presumed nasal polyp. Because the hypothalamus can be contained within the encephalocele, hypopituitarism can occur, affecting growth hormone and antidiuretic hormone production.8 Other midline intracranial anomalies have been reported, including agenesis of the corpus callosum, and absent optic chiasm, as well as an association with renal agenesis. Cerebrovascular anomalies have also been frequently demonstrated, most notably ipsilateral intracranial vascular dysgenesis.
If both intracranial carotid arteries are involved, then hypertrophy of collateral vessels at the base of the brain can occur, resembling a “puff of smoke” on arteriogram.9 This descriptively is called moyamoya syndrome.10 Finally, some girls with morning glory disc anomaly, infantile hemangiomas, and dysplasia of the carotid vasculature have PHACE syndrome, which includes posterior fossa malformations, facial hemangiomas, arterial anomalies, cardiac anomalies and aortic coarctation, and eye anomalies.
Differential diagnosis
The etiology of morning glory disc anomaly is poorly understood. There are some similarities to optic disc coloboma with interference in the closure of the posterior aspect of the fetal fissure. Thus the morning glory disc is sometimes misdiagnosed as an optic nerve coloboma. A coloboma is characterized by a larger bowl-shaped area of excavation decentered inferiorly in the relative position of the embryonic fissure. The inferior neuroretinal rim is thin, while the superior neuroretinal rim is spared, and the nerve tissue appears compressed. The excavation may extend to involve the adjacent choroid and retina. Microcornea, iris coloboma, and microphthalmia are frequently present. In coloboma there is also no central glial tuft and there is minimal peripapillary pigmentary disturbance. Optic disc coloboma is often familial, bilateral, and there is no sex predilection. Coloboma may occur as part of other systemic conditions, including CHARGE (colobomas and cranial nerves, heart problems, atresia of the choanae, retardation of growth/development, genital and urinary abnormalities, ear and hearing abnormalities) association, Walker-Warburg syndrome, Goltz focal dermal hypoplasia, Aicardi syndrome, Goldenhar sequence, and linear sebaceous nevus syndrome. Morning glory disc anomaly is distinguished from coloboma by the abnormal formation of the posterior sclera and lamina cribrosa. Herniation of intraocular contents through the defect develops, leading to a conical deformity, which then might interfere with fetal fissure closure. There is also interference with regression of the hyaloid vascular system, which can persist centrally within the dysplastic disc. Thus, morning glory disc anomaly may represent a spectrum of abnormal development that would include optic pits and peripapillary contractile staphyloma. The association with abnormal angiogenesis supports a hypothesis of abnormal mesenchymal differentiation; possibly due to a neuroectodermal induction abnormality. Histologically, findings of adipose tissue and smooth muscle have been found within the peripapillary sclera.
Treatment and follow-up
The visual prognosis in individuals with morning glory disc anomaly is poor. In addition to the abnormal disc itself and the predilection for serous retinal detachments, there is an added compounding variable of high refractive errors, amblyopia, and strabismus. Although ocular realignment surgery and treatment of anisometropic amblyopia is recommended and may result in some recuperation of vision, it is rare to see dramatic improvements. Treatment of the other associated abnormalities requires an interdisciplinary approach, often including neurosurgery, interventional neuroradiology, otolaryngology, and dentistry. All patients discovered on routine ophthalmic examination to have morning glory disc anomaly should have brain MRI, MRA, and timely referrals to the appropriate subspecialist.
References
- Kindler P. Morning glory syndrome: unusual congenital optic disk anomaly. Am J Ophthalmol. 1970; 69(3):376-384.
- Lee BJ, Traboulsi EI. Update on the morning glory disc anomaly. Ophthalmic Genet. 2008; 29(2):47-52.
- Steinkuller PG. The morning glory disk anomaly: case report and literature review. J Pediatr Ophthalmol Strabismus. 1980;17(2):81-87.
- Beyer WB, Quencer RM, Osher RH. Morning glory syndrome: A functional analysis including fluorescein angiography, ultrasonography, and computed tomography. 1982; 89:1362-1364
- Irvine AR, Crawford JB, Sullivan JH. The pathogenesis of retinal detachment with morning glory and optic pit. 1986; 6:146-150.
- Sawada Y, Fujiwara T, Yoshitomi T. Morning glory disc anomaly with contractile movements. Graefes Arch Clin Exp Ophthalmol. 2012; 250(11):1693-1695.
- Ellika S, Robson CD, Heidary G, Paldino MJ. Morning glory disc anomaly: characteristic MR imaging findings. AJNR Am J Neuroradiol. 2013; 34(10):2010-2014.
- Loddenkemper T, Friedman NR, Ruggieri PM, Marcotty A, Sears J, Traboulsi EI. Pituitary stalk duplication in association with moya disease and bilateral morning glory disc anomaly - broadening the clinical spectrum of midline defects. J Neurol. 2008; 255(6):885-890.
- Quah BL, Hamilton J, Blaser S, Héon E, Tehrani NN. Morning glory disc anomaly, midline cranial defects and abnormal carotid circulation: an association worth looking for. Pediatr Radiol. 2005; 35(5):525-528.
- Komiyama M, Yasui T, Sakamoto H, Fujita K, Sato T, Ota M, Sugita M. Basal meningoencephalocele, anomaly of optic disc and panhypopituitarism in association with moyamoya disease. Pediatr Neurosurg. 2000; 33(2):100-104.