Introduction
Vertically incomitant pattern strabismus is used to describe the type of strabismus wherein the amount of horizontal deviation changes during the excursion of the eye from upgaze to downgaze. It is a common association with many types of strabismus, especially infantile esotropia and intermittent exotropia. Several patterns have been described for the type of vertical incomitance observed (eg, “A” or “V” patterns), depending upon the relative increase or decrease in the horizontal deviation during the vertical eye movement. The pathophysiology of this phenomenon is multifactorial and has been attributed to factors including oblique muscle dysfunction, horizontal or vertical recti anomaly, displacement of muscle pulleys, and orbital anomalies. The identification of the pattern and its underlying mechanism is essential to plan a proper surgical management in strabismus. In this chapter, we will discuss in detail the various types of pattern strabismus, its mechanisms, and the appropriate surgical intervention for the same.
Types of Pattern Strabismus
Around 12%-50% cases of horizontal strabismus will manifest vertical incomitance or a pattern. Duane1 introduced the concept of pattern in strabismus in 1897 when he described “V” pattern in bilateral superior oblique palsy. Urrets-Zavalia2 first described the need to identify vertical incomitance in a comitant horizontal strabismus in 1948. Urist3 introduced the terms “A and V” pattern in strabismus. Although “A” or “V” patterns are the most common patterns observed (Figure 1), there are several other patterns that can be seen in a comitant strabismus.
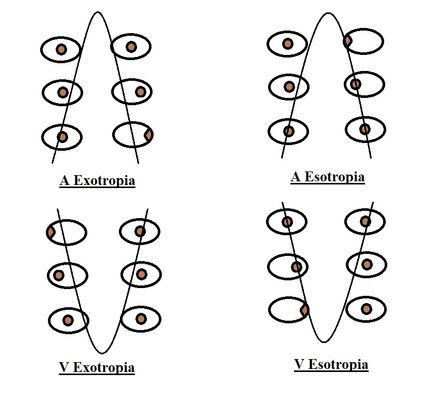
Figure 1. A and V patterns seen in exodeviation and esodeviation. (Courtesy of Vinay Gupta, BSc Optometry)
The types of patterns described are:
- A-pattern: When the eye converges as the eye moves from down to upgaze, it is termed as an A-pattern. Therefore in an A-pattern esotropia, the deviation is more in upgaze than in downgaze (Figure 2), and in an A-pattern exotropia the deviation is more in downgaze than in upgaze. The A-pattern is considered significant if the difference in horizontal deviation between the 2 gazes is ≥ 10 prism diopters.
- V-pattern: When the eye converges as the eye moves from up to downgaze, a V-pattern is present. In V-pattern esotropia, the deviation is more in downgaze than in upgaze, and in V-pattern exotropia the deviation is more in upgaze than in downgaze (Figure 3). This is the most common type of pattern in strabismus. The V-pattern is considered to be significant if the difference in horizontal deviation between the 2 gazes is ≥ 15 prism diopters.
- Y-pattern: This is considered to be a subtype of V-pattern, where the horizontal deviation remains stable from midline downgaze to primary position, and a relative divergence is seen on upgaze. It is seen in bilateral inferior oblique overaction, Brown syndrome, or Duane syndrome (DS).
Arrow pattern is another variant of Y-pattern, where a relative convergence is seen from midline primary position to downgaze. This may be seen in bilateral superior oblique palsy.
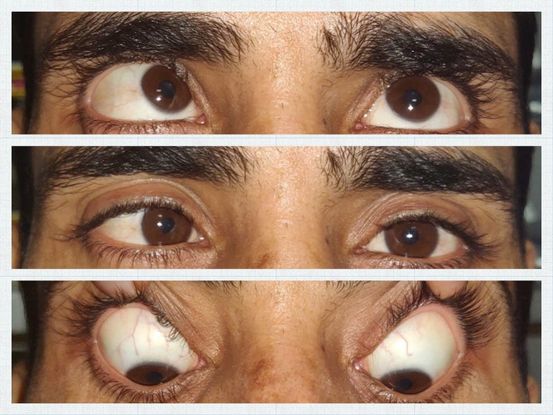
Figure 2. Clinical photograph of the patient showing A-pattern esotropia. (Courtesy of Vinay Gupta, BSc Optometry)

Figure 3. Clinical photograph of the patient showing V-pattern exotropia. (Courtesy of Vinay Gupta, BSc Optometry)
- λ-pattern (lambda): This is considered to be a subtype of A-pattern, where the horizontal deviation remains stable from midline upgaze to primary position and a relative divergence is seen on downgaze. This pattern may be seen with bilaterally underacting inferior recti or overacting superior obliques.
- X-pattern: As the name implies, here a relative divergence of the eyes is seen in both upgaze and downgaze (Figure 4). This is suggestive of a tight lateral rectus that may be seen in long-standing exodeviation or type 3 DS. Overaction of both superior and inferior obliques has also been implicated in some cases.
- <>-pattern (diamond): A relative convergence of the eyes is seen in both upgaze and downgaze in a diamond pattern that may be seen in cases of tight medial recti.

Figure 4. Clinical photograph of the patient showing X-pattern exotropia with divergence in upgaze and downgaze. (Courtesy of Vinay Gupta, BSc Optometry)
Pseudo patterns
Pseudo A or V patterns may be seen in certain forms of strabismus in the absence of a true pattern. Pseudo V-esotropia may be seen in accommodative esotropias with uncorrected hyperopic refractive error. The patient shows accommodative convergence in primary and downgaze as opposed to upgaze simulating a V-pattern. Likewise, pseudo V-exotropia may be seen in intermittent divergent strabismus, wherein the patient fuses for downgaze and breaks in upgaze, manifesting exodeviation. Pseudo patterns must be ruled out by measuring the deviations after prescribing appropriate refractive correction or observing the deviation under cover to prevent fusion.
Pathophysiology of Pattern Strabismus
Several theories have been put forth to explain the occurrence of pattern in horizontal strabismus. But there is no clear consensus on the exact pathophysiology of patterns in comitant horizontal strabismus. According to Kushner,4 the pattern is a result of complex interactions occurring amongst all the extraocular muscles. Broadly, it has been classified as peripheral (mechanical) or central (neural) (Figure 5).
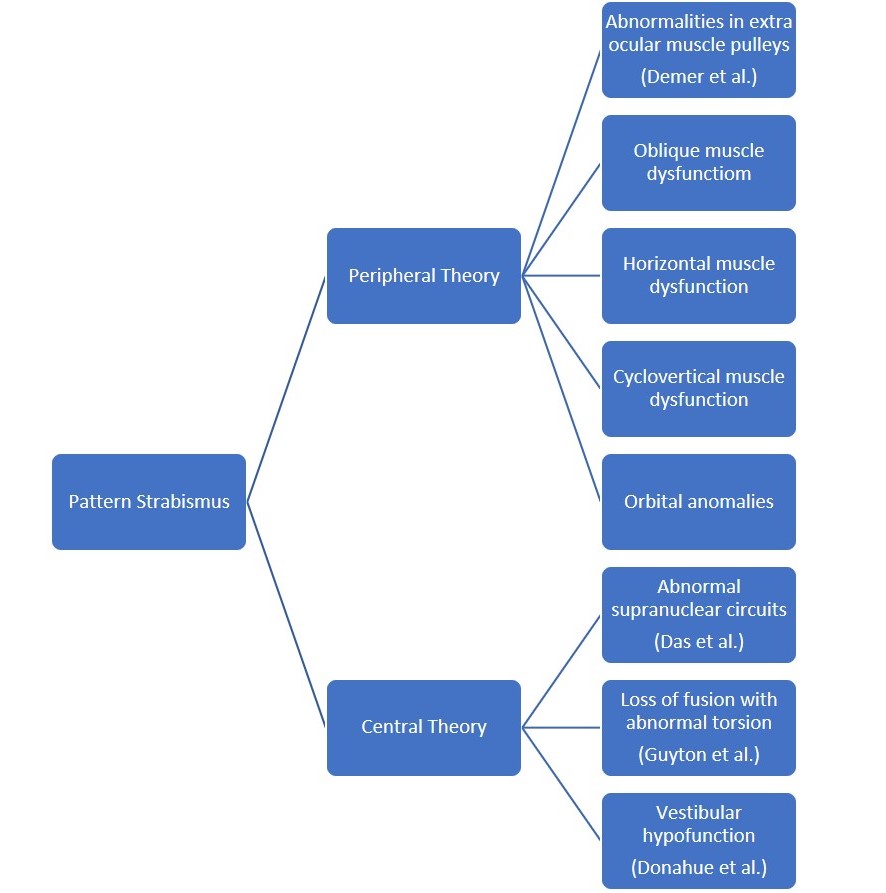
Figure 5. Flowchart showing various theories for pattern strabismus. (Courtesy of Vinay Gupta, BSc Optometry)
Peripheral (Mechanical) factors
- Oblique muscle dysfunction: In 1959, Knapp5 proposed the theory of oblique muscle dysfunction, which is the most accepted and commonly encountered mechanism in pattern strabismus. This theory is based on the fact that obliques are weak abductors. Therefore, when inferior oblique muscles overact and superior oblique muscles underact, it causes a relative divergence in upgaze compared to downgaze, resulting in a V-pattern (Figure 6). A new terminology devised by CEMAS (Classification of Eye Movement Abnormalities and Strabismus) for this phenomenon is overelevation in adduction.6 On the contrary, when superior obliques overact and inferior obliques underact, it causes relative divergence in downgaze, resulting in an A-pattern referred to as over-depression in adduction (Figure 7).
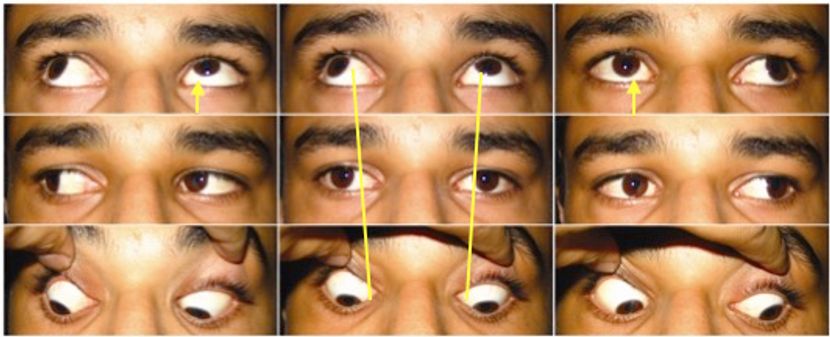
Figure 6. Clinical photograph of the patient showing V-pattern exotropia associated with bilateral inferior oblique overaction. (Courtesy of Vinay Gupta, BSc Optometry)
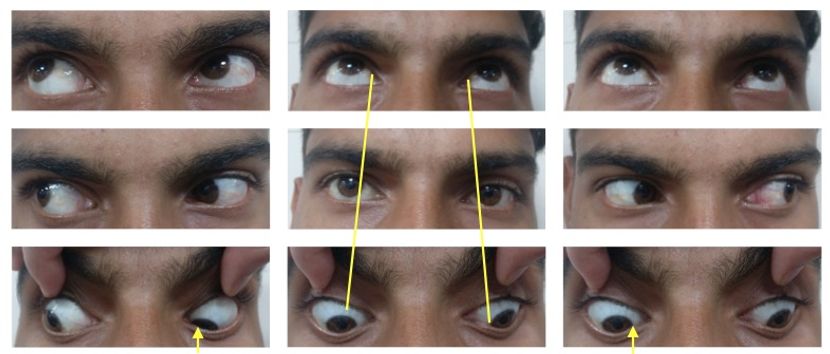
Figure 7. Clinical photograph of the patient showing A-pattern exotropia associated with bilateral superior oblique overaction. (Courtesy of Vinay Gupta, BSc Optometry)
- Horizontal muscle dysfunction: The imbalance of horizontal muscle forces as a cause of pattern strabismus was proposed by Urist.3 According to this theory, V-pattern is a result of overaction of medial rectus in downgaze and lateral rectus in upgaze, and A-pattern is due to medial rectus underaction in downgaze and lateral rectus underaction in upgaze. Electromyography studies, however, do not support the hypothesis.
- Cyclovertical muscle dysfunction: This is a less-accepted theory, wherein V-pattern is associated with underaction of superior rectus and overaction of its yoke muscle, that is, the inferior oblique. Similarly, A-pattern is associated with inferior rectus underaction and superior oblique overaction.
- Muscle pulley dysfunction: This interesting concept proposes the role of extraocular muscle pulley heterotopy in the causation of vertical incomitance. Muscle pulleys or sleeves are considered to be the functional origin of extraocular muscles. They comprise the posterior condensation of the Tenon capsule, along with components of elastin, collagen, and smooth muscles. The orbital layer of each extraocular muscle is inserted in their pulleys that stabilize the posterior muscle during contraction. Anomalies of muscle pulleys can result in slippage of the muscle during globe rotations. This theory has been supported by the magnetic resonance imaging (MRI) studies7, 8 that have revealed even small mislocations (< 2 mm) of muscle pulleys, especially perpendicular to the plane of muscle action (vertical displacement of horizontal rectus muscle pulleys and horizontal displacement of vertical rectus muscle pulleys) can cause vertical incomitance. An inferior mislocation of lateral rectus pulley can resemble an inferior oblique overaction and generate V-pattern. While a superior displacement can resemble a superior oblique overaction and manifest as A-pattern.
- Orbital anomalies: Orbital anomalies, as may be seen in craniofacial abnormalities, including palpebral fissure slant, hydrocephalus, plagiocephaly, Crouzon, Apert, etc. indirectly affect the oblique muscle function. The role of sagittalization (becoming more parallel to sagittal plane) and desagittalization (becoming more parallel to coronal plane) of oblique muscles leading to misdirected muscle forces have been proposed by Gobin.9 In plagiocephaly, the retroplacement of trochlea causes desagittalization and thus pseudo-paresis of superior oblique presenting as V-pattern (Figure 8). Conversely, in hydrocephalus with frontal bossing, there is frontal displacement of trochlea that causes sagittalization and overaction of superior oblique, presenting as A-pattern. In patients with primary orbital anomalies, such as Crouzon and Apert syndromes, extorsion of the rectus muscle pulleys primarily accounts for the pattern strabismus.10
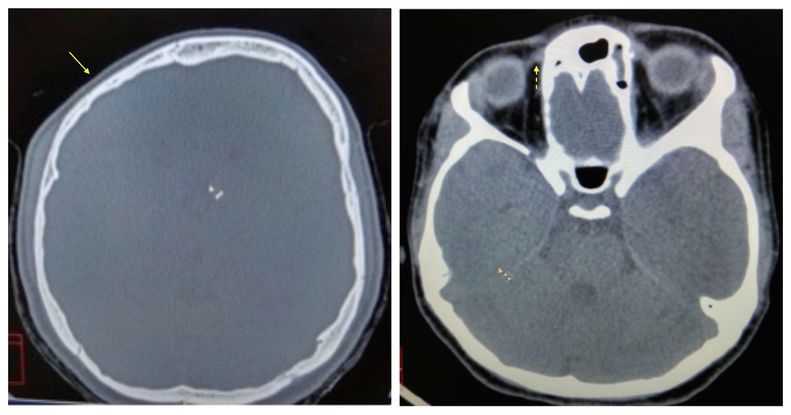
Figure 8. Computed Tomography (CT) brain showing right-sided plagiocephaly (yellow arrow) with thin superior oblique on the affected side (yellow dashed arrow). (Courtesy of Vinay Gupta, BSc Optometry)
Central factors
- Loss of fusion: Miller and Guyton11 have put forth the theory of loss of fusion as a predisposing factor for pattern strabismus. They followed up the patients with intermittent exotropia (without any pre-existing pattern) postoperatively and found that 43% of patients who developed consecutive esotropia manifested A or V patterns, versus only 5% of those who were aligned. They proposed that loss of fusion is instrumental in causing torsional drift, referred to as “sensory torsion,” which alters the action of the recti.
An excyclotorsion of both eyes makes superior recti partial abductors and inferior recti partial adductors. Consequently, the occurrence of divergence in upgaze and convergence in downgaze causes a V-pattern (Figure 9). Excyclotorsion also converts medial recti into partial elevators and lateral recti into partial depressors, which results in elevation in adduction, resembling inferior oblique overaction. Similarly, incyclotorsion of the eye alters the muscle force vectors of the recti to produce an A pattern.
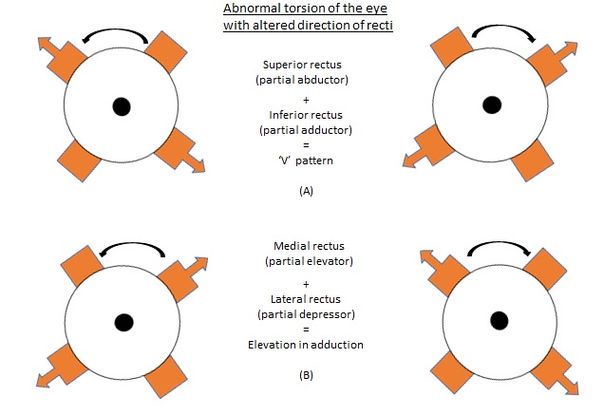
Figure 9. V-pattern due to excyclotorsion of the eyes. (Courtesy of Vinay Gupta, BSc Optometry)
- Supranuclear anomalies: Animal studies have raised the possibility of the role of abnormal supranuclear circuits in pattern strabismus. In these studies, the eye that was visually deprived during the critical period of visual development manifested pattern strabismus.12 The non-viewing eye has shown cross-coupled movements which could be due to cross-wiring between the vertical and horizontal eye movement areas.13
- Vestibular anomalies: In a study conducted on the patients with neurological deficits including neural tube anomalies, spina bifida, and hydrocephalus, an association between A-pattern strabismus and brainstem/cerebellar lesions was seen. The authors hypothesized that the pattern was due to imbalance between the anterior and posterior semicircular canals. Based on this, the authors have described A-pattern strabismus as a “special form of bilateral skew deviation”.14
Patient Work-up
It is paramount to rule out a vertical pattern in every case of comitant strabismus, as our management would be defined by the same. Apart from the basic strabismus work-up, the additional assessment needed in the presence of patterns is to look for:
- Abnormal head posture: Chin elevation may be seen in V-exotropia or A-esotropia; chin depression may be a feature in A-exotropia and V-esotropia.
- Measurement of deviation in primary position, 25 degrees upgaze and 35 degrees downgaze: A case of V-esotropia may be misdiagnosed as convergence excess type of esotropia. Similarly, V-exotropia may be confused with divergence excess type of exotropia. Measurement of deviation in the 3 sets of gaze will reveal the true pattern.
- Measurement of deviation in 9 gazes.
- Overelevation or overdepression in adduction (measuring oblique muscle overaction).
- Ocular torsion: Objective assessment of ocular torsion can be done on fundus examination based on the relative position of macula and optic nerve head. Normally, the fovea is located 0.3 disc diameters below the horizontal line, passing through the center of the disc. In excyclotorsion, the macula lies further below this line, and in incyclotorsion, the macula lies above it. As per Phillips and Hunter,15 ocular torsion is considered to be a more reliable predictor of oblique muscle overactions than versions.
- Orbital imaging may be considered in patients with craniofacial anomalies and in cases where the cause of the pattern cannot be identified.
Surgical Management
The management of pattern strabismus can be difficult. It requires not only the correction of the horizontal deviation, but also of the vertical pattern. The pattern needs to be corrected only if it is significant (as described above) or if the patient is symptomatic in the direction of largest deviation. The type of surgery is governed by the underlying pathophysiology of the pattern and directed towards the implicated extraocular muscle. The 2 most commonly performed surgeries for correction of vertical incomitance in a horizontal strabismus are:
- Oblique muscle surgery: V-pattern strabismus presenting with overelevation in adduction is mostly due to inferior oblique overaction. Likewise, an A-pattern strabismus with overdepression in adduction is due to superior oblique overaction. Oblique muscle weakening is the procedure of choice in such cases, along with horizontal recti surgery to correct the horizontal deviation. This will correct the pattern and the cosmetically unacceptable upshoot or downshoot in adduction and will decrease the torsion. Usually, symmetrical weakening of the obliques is done unless there is definite asymmetrical overaction or a vertical deviation in primary position. As the oblique muscle weakening does not significantly alter deviation in primary gaze, the amount of horizontal recti surgery is decided by the deviation in primary gaze.
Video 1: Inferior Oblique Recession Procedures
Various inferior oblique weakening procedures are:
- Fink’s recession: This technique recesses the inferior oblique along its natural course. The anterior point of new insertion is 6 mm below and posterior to the inferior end of lateral rectus insertion. This corresponds to 8 mm recession of inferior oblique.
- Park’s recession: In this technique, we reattach the anterior end of inferior oblique 2 mm lateral and 3 mm behind the lateral border of inferior rectus. This corresponds to 10 mm recession of inferior oblique, and causes a little antero-positioning in addition to recession of inferior oblique. For more pronounced effect, the anterior end of the inferior oblique can be placed near the vortex vein in such a fashion to straddle the vein, corresponding to a 14 mm recession of the inferior oblique.
Antero-positioning means that the inferior oblique is anteriorized with respect to its natural course. In contrast to pure recessions, antero-positioning alters the path of the muscle and thus brings about greater weakening of the muscle and changes it from an elevator to a weak depressor.
- Inferior oblique recession with antero-positioning (Elliot and Nankin recession16): Here both the muscle ends are bunched up and placed adjacent to the lateral end of inferior rectus insertion with the 2 scleral tunnels 1-2 mm apart horizontally. This causes recession along with antero-positioning of the inferior oblique and results in limited elevation of the eye. The postoperative limitation of elevation during abduction resulting in an apparent inferior oblique overaction in the contralateral eye, often accompanied with Y-pattern exodeviation, has been described by Kushner.17 This phenomenon has been termed as “antielevation syndrome” by Mims and Wood.18 The neurofibrovascular bundle of the inferior oblique that inserts in the posterior fibers prevents the eye from elevating, by acting as a tether.19 This has been described as the “J deformity anteriorization” by Kenneth Wright.
This antielevation effect can be useful in cases of dissociated vertical deviation (DVD) and unilateral superior oblique palsy (SOP) with hypertropia. But some patients may have diplopia in upgaze. The antielevation effect can be minimized by placing the inferior oblique 1-2 mm posterior to the lateral border of the insertion of the inferior rectus, or by placing the oblique at the equator of the globe, without sacrificing the primary action of eliminating oblique overaction and adding to inferior pull to help correct the DVD.20
- Inferior oblique recession with antero-positioning (Modified Elliot and Nankin recession): This is a modification of the existing Elliot and Nankin recession (unpublished), wherein the anterior end of inferior oblique is placed, as in the Elliot and Nankin technique, and the posterior end is inserted 5 mm posterior along the lateral border of the inferior rectus muscle. This produces slightly less antero-positioning effect than the Elliot and Nankin technique but avoids the “antielevation syndrome,” as the posterior fibers are not stretched. Therefore, this technique is preferred by the authors for the management of pattern strabismus with severe inferior oblique overaction.
Kenneth Wright has described the “graded anteriorization” procedure, wherein graded anterior placement of the inferior oblique is done depending on the severity of overaction.
- Graded 1+ and 2+ inferior oblique recession18 (Total antero-positioning): Here the muscle is inserted 1 mm and 2 mm anterior to the lateral border of inferior rectus, respectively. It has a greater antielevation effect compared to the Elliot and Nankin procedure.
- Anteronasal transposition (ANT): This is a relatively new technique, wherein the inferior oblique is inserted along the nasal border of the inferior rectus muscle. This totally abolishes its effect as an elevator and extorter and converts it into a depressor and intorter in adduction. This is a very strong weakening procedure that is not performed in comitant strabismus. It has been described for superior oblique palsies to obviate excyclotorsion.19 Adjustable ANT has also been described.23
- Myectomy and extirpation/denervation have been described but are not preferred procedures by the authors, as the results may be unpredictable, and anteriorization cannot be achieved by these procedures.
The most common complication of inferior oblique surgeries is residual overaction, which may be due to missed posterior fibers. Other complications include fat adherence syndrome, orbital hemorrhage, pupillary dilatation, injury to lateral rectus muscle or vortex vein, and rarely torsional diplopia.
Various superior oblique weakening procedures are:
- Posterior tenectomy of superior oblique (PTSO): This is commonly advocated for the correction of A-pattern. As the name suggests, the posterior fibers responsible for depressor action of the muscle are excised, and the anterior 2 mm responsible for incyclotorsion is spared.
Video 2: Posterior Tenectomy of Superior Oblique
- Full muscle recession: The superior oblique is disinserted and reattached to the sclera nasally. Translational recession has been described wherein superior oblique is sutured 6 mm nasal to the nasal border of the superior rectus and 12 mm posterior to limbus. This prevents the limitation of depression in abduction.
- Lengthening procedures including using silicone band expanders and loop tenotomy are other weakening procedures that may be indicated in severe A pattern.
- Split-tendon elongation is a procedure where the tendon is split, and the cut ends are tied together. It provides a graded effect without the need of placing any foreign object. The risk in this procedure is that the sutures may cut through the thin superior oblique tendon.
- Free tenotomy, tenectomy, Z-tenotomy and split-lengthening procedures have also been described.
The most common complication of superior oblique weakening procedure is residual overaction due to missed posterior fibers of the superior oblique. Another common occurrence is the superior oblique palsy, wherein the patients with good fusion can complain of torsional diplopia. Other complications include injury to the superior rectus or the vortex veins.
- Horizontal recti surgery with vertical displacement of insertions: Knapp24 advocated the vertical displacement of horizontal recti to correct for pattern strabismus. When there is a pattern in the absence of oblique muscle overaction, upshifts or downshifts of the horizontal recti can be used to collapse the pattern. The muscle insertion should be shifted in the direction where its effect has to be weakened. For example, in a V-pattern medial rectus insertion is shifted down, which enhances its effect in upgaze and decreases in downgaze. Likewise, for the correction of A-pattern, medial rectus insertion is shifted up. Lateral rectus insertion is shifted up in V-pattern and shifted down in A-pattern strabismus. Therefore, medial rectus is always shifted toward the apex, and lateral rectus is shifted toward the base of the A or V pattern (Figure 10), leading to the common mnemonic MALE: medials to the apex, laterals to the empty space of the pattern. The amount of shift depends on the severity of the pattern. Usually, a shift of half a muscle width (ie, 5 mm) is recommended, which can correct up to 15-20 PD of the pattern.
Recessions and resections of the horizontal recti are combined with upshifts and downshifts to manage the horizontal deviation, as well as the pattern. The amount of recession and resection is planned according to the horizontal deviation in primary gaze, and no correction is needed for the shift procedure. However, the shifts of the horizontal recti can induce torsion, particularly if the shifts are used in unilateral surgery.25
If the severity of the pattern is not explained entirely by any one mechanism, then we can consider combining the oblique muscle surgery with the shifts of the horizontal recti.
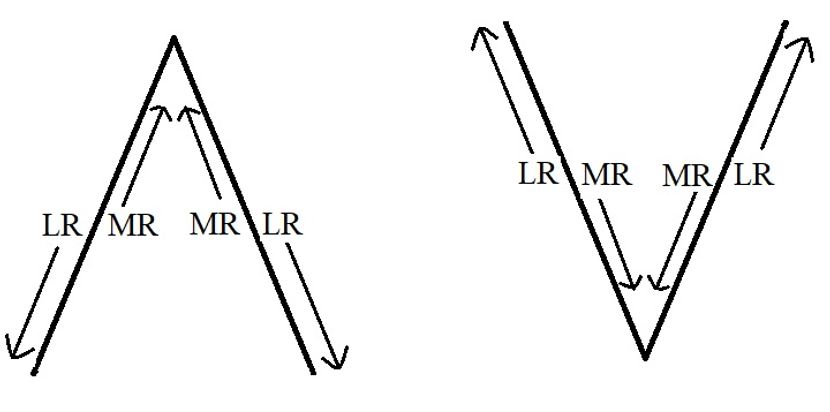
Figure 10. Direction of vertical displacement of horizontal recti in pattern strabismus- Medial rectus is shifted towards the apex and lateral rectus is shifted towards the base of A or V pattern. (Courtesy of Vinay Gupta, BSc Optometry)
Other less commonly performed procedures are:
- Slanting muscle insertion: In 1971, Boyd26 and colleagues described a new technique of slanting the insertions of medial and lateral rectus muscles for recessions or resections in A and V patterns without overaction of vertically acting muscles. This technique did not gain much popularity. For V-esotropia, slanting medial rectus recession is done with greater recession of the inferior muscle insertion. The slant is reversed for A-exotropia. V-exotropia requires more recession of the upper end, and A-exotropia requires more recession of lower end of recessed lateral recti.
- Vertical recti surgery with horizontal displacement of insertion: This technique was described by Miller.27 Similar to the muscle shifts described for horizontal recti, horizontal shifting of the vertical recti insertion can also be done, which affects the adducting force of the vertical recti. This is not commonly advocated.
Conclusion
Occurrence of a pattern in horizontal comitant strabismus is an interesting phenomenon. The pathophysiology is varied, with no clear consensus. The first challenge for the clinician is to diagnose the pattern and the second is to identify the cause. If the pattern is significant, or the patient is symptomatic, it necessitates intervention. Oblique muscle weakening is the preferred approach in the presence of oblique muscle overactions. In their absence, upshifts or downshifts of the horizontal recti insertion can be planned. Pattern strabismus associated with craniofacial anomalies is complex and often difficult to manage.
Acknowledgements
We would like to extend sincere thanks to Mr. Vinay Gupta, BSc Optometry, for the contribution of figures in this chapter.
References
- Duane A. Isolated paralysis of extraocular muscles. Arch Ophthalmol. 1897; 26: 317–334.
- Urrets-Zavalia A. Abduction en la elevacion. Arch Opfalmol. 1948; 23: 124–134.
- Urist MJ. The etiology of the so-called A and V syndromes. Am J Ophthalmol. 1958; 46: 835–844.
- Kushner BJ. The role of ocular torsion on the etiology of A and V patterns. J Pediatr Ophthalmol Strabismus. 1985; 17:222.
- Knapp P. Vertically incomitant horizontal strabismus, the so called “A” and “V” syndromes. Trans Am Ophthalmol Soc. 1959;57:666-699.
- Hertle RW. A next step in naming and classification of eye movement disorders and strabismus. J AAPOS. 2002; 6(4):201-202.
- Clark RA, Miller MJ, Rosenbaum AL, Demer JL. Heterotopic muscle pulleys or oblique muscle dysfunction? JAAPOS. 1998;2:17–25.
- Oh SY, Clark RA, Velez F, Rosenbaum AL, Demer JL. Incomitant strabismus associated with instability of rectus pulleys. Invest Ophthalmol Vis Sci. 2002;43:2169–2178.
- Gobin MH. Sagittalization of the oblique muscles as a possible cause for the “A”, “V”, and “X” phenomena. Br J Ophthalmol. 1968;52:13–18.
- Weiss AH, Phillips J, Kelly JP. Crouzon syndrome: relationship of rectus muscle pulley location to pattern strabismus. Invest Ophthalmol Vis Sci. 2014;55:310-317.
- Miller MM, Guyton DL. Loss of fusion and the development of A or V patterns. JPOS. 1994;31:220–224.
- Das VE, Fu LN, Mustari MJ, Tusa RJ. Incomitance in monkeys with strabismus. Strabismus. 2005;13:33–41.
- Ugolini G, Klam F, Dans MD. Horizontal eye movement networks in primates as revealed by retrograde transneuronal transfer of rabies virus: differences in monosynaptic input to “slow” and “fast” abducens motoneurons. J Comp Neurol. 2006;498:762–785.
- Donahue SP, Itharat P. A-pattern strabismus with overdepression in adduction: a special type of bilateral skew deviation? JAAPOS. 2010;14:42–46.
- Phillips PH, Hunter DG. Evaluation of ocular torsion and principles of management. In: Rosenbaum AL, Santiago AP(eds) Clinical Strabismus Management, Principles and Surgical Techniques. WB Saunders: Philadelphia, 1999:52–72.
- Elliott RL, Nankin SJ. Anterior transposition of the inferior oblique. J Pediatr Ophthalmol Strabismus. 1981;1835-1838.
- Kushner BJ. Restriction of elevation in abduction after inferior oblique anteriorization. JAAPOS. 1997;1:55-62.
- Mims JL 3rd, Wood RC. Antielevation syndrome after bilateral anterior transposition of the inferior oblique muscles: incidence and prevention. JAAPOS. 1999:333-336.
- Stidham DB, Stager DR, Kamm KE, Grange RW. Stiffness of the inferior oblique neurofibrovascular bundle. Invest Ophthalmol Vis Sci. 1997;38:1314-20.
- Yoo E-J, Kim S-H. Modified inferior oblique transposition considering the equator for primary inferior oblique overaction (IOOA) associated with dissociated vertical deviation (DVD). Strabismus. 2014;22:13-17
- Mims JL 3rd, Wood R. Bilateral anterior transposition of the inferior oblique. Arch Ophthalmol. 1989; 107:41-44.
- Stager DR Jr, Beauchamp GR, Wright WW, Felius J, Stager D Sr. Anterior and nasal transposition of the inferior oblique muscles. JAAPOS. 2003;7:167-173.
- Saxena R, Singh D, Chandra A, Sharma P. Adjustable anterior and nasal transposition of inferior oblique muscle in case of torsional diplopia in superior oblique palsy. Indian J Clin Exp Ophthalmol. 2015;1:104-106.
- Knapp P: Vertically incomitant horizontal strabismus, the so-called “A” and “V” syndromes. Trans Am Ophthalmol Soc. 57:666, 1959
- Sharma P, Halder M, Prakash P. Torsional changes in surgery for A-V phenomena. Indian J Ophthalmol. 1997; 45:31–35.
- Boyd TA, Leitch GT, Budd GE. A new treatment for ‘A’ and ‘V’ patterns in strabismus by slanting muscle insertions. A preliminary report. Can J Ophthalmol. 1971;6:170-177.
- Miller JE. Vertical recti transplantation in the A and V syndromes. Arch Ophthalmol. 1960;64:175-179.