The links to each individual chapter of the Color Atlas of Gonioscopy are available at the Chapters link, below.
Viewing the anterior chamber of a normal eye directly (3‑1) is not possible. Light from the junction of the iris and cornea strikes the tear–air interface at a shallow angle, and it is totally reflected back into the eye (3‑2). This is the principle of total internal reflection. If light from the interior of the eye strikes the cornea at an angle steeper than 46° (the critical angle), the light will exit the eye and the trabecular meshwork will be visible (Shields, 1992). Rarely, this may occur in eyes with keratoconus, keratoglobus, or severe myopia (3‑3). The angle of approach to the trabecular meshwork can be altered if the limbus is indented, as shown by Trantas in his initial description of gonioscopy (3‑4) (Trantas, 1907).
In modern gonioscopy, contact lenses are used to overcome the problem of total internal reflection. Two basic types of lens are used: the direct lens and the indirect lens.
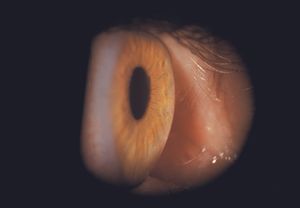
3-1 Slit-lamp view attempting to visualize the angle in a normal eye. No angle structures are visible because of total internal reflection
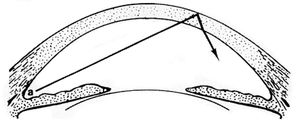
3-2 Light from the anterior chamber angle (a) undergoes total internal reflection at the tear–air interface and is not visible to the examiner.
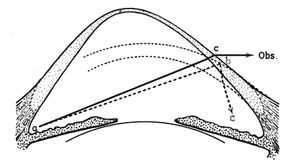
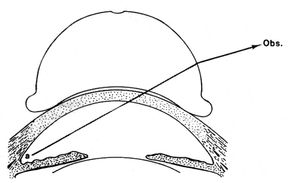
3-3 In an eye with keratoconus light from the trabecular meshwork (a) strikes the cornea at a steep enough angle to permit direct visualization of the trabecular meshwork by the observer (Obs.). This is an uncommon situation.
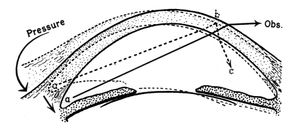
3-4 Indentation of the limbus brings angle structures (a) into direct view without a lens. It is very difficult to obtain an undistorted view in this manner.
Direct Gonioscopy
Direct gonioscopy is performed with a steeply convex lens, which permits light from the angle to exit the eye closer to the perpendicular at the interface between the lens and the air (3‑5). The Koeppe lens (3‑6), which is a 50-diopter lens, is placed on the eye of a recumbent patient using saline to bridge the gap between lens and cornea (3‑7). The examiner views the angle through a hand-held binocular microscope, which is counterbalanced to permit ease of handling. Illumination is provided by a light source that is held in the other hand (3‑8). The Koeppe lens magnifies ×1.5. This, in combination with the ×16 magnification of the oculars, yields a total magnification of ×24. There are Koeppe lenses in several sizes to suit infants to adults.
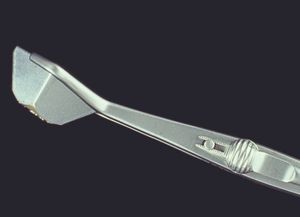
Direct lenses are used for surgical procedures such as goniotomy and goniosynechialysis. The Hoskins-Barkan (3‑9 to 3‑11) and Swan-Jacobs (3‑12) lenses are most commonly used. These lenses can also be used to examine sedated infants with an operating microscope or a portable slit lamp (3‑13 and 3‑14).
3-5 Direct gonioscopic lenses change the angle of the interface with the air so that the light from the trabecular meshwork (a) exits more perpendicularly.

3-6 The Koeppe lens for direct gonioscopy is available in several sizes. (Courtesy of Ocular Instruments.)
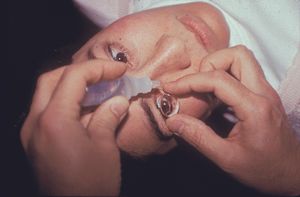
3-7 Saline is used to bridge the gap between the Koeppe lens and the cornea in a supine patient. (Courtesy of Paul R. Lichter, MD, University of Michigan, and A. Tim Johnson, MD, PhD, Department of Ophthalmology & Visual Sciences, University of Iowa.)

3-8 Examination of supine patient with Koeppe lens using counterbalanced biomicroscope and Barkan illuminator. (Courtesy of Paul R. Lichter, MD, University of Michigan, and A. Tim Johnson, MD, PhD, Department of Ophthalmology & Visual Sciences, University of Iowa.)



3‑9, 3‑10, 3‑11 Hoskins-Barkan surgical contact lenses in three sizes (for infant, premature infant, or adult). This direct lens is used with loupes or an operating microscope for goniotomy and other angle surgery. (Courtesy of Ocular Instruments.)

3‑12 Swan-Jacobs surgical contact lens. This direct lens is used with loupes or an operating microscope for goniotomy and other angle surgery. (Courtesy of Ocular Instruments.)

3-13 Gonioscopy can be performed on sedated infants with a direct contact lens and an operating microscope or a portable slit lamp. Here a Swan-Jacobs lens is used with a portable slit lamp to examine the eye of a sedated child with primary infantile glaucoma.

3-14 View through a Swan-Jacobs lens into the angle of a child with primary infantile glaucoma.
Indirect Gonioscopy
The lenses used in indirect gonioscopy use mirrors to overcome total internal reflection. The mirror redirects light from the angle so that it exits the eye perpendicularly to the lens-air interface (3‑15). The examination is performed at the slit lamp and takes advantage of the latter’s flexible illumination and magnification system.
The Goldmann three-mirror lens (3‑16 and 3‑17) has one mirror dedicated to viewing the angle. There are two additional mirrors for examination of the peripheral retina. The Goldmann lens is coupled to the cornea by means of a viscous methylcellulose fluid. The lens has a broad (12 mm) area of contact with the globe and, under the application of pressure, can artificially close the angle or reflux blood into Schlemm’s canal. The single-mirror Goldmann lens has only the gonioscopic mirror (3‑18). The Ritch trabeculoplasty laser lens (3‑19) is similar to the Goldmann lens except that all four of its mirrors are directed at the angle; two mirrors face the angle at 59° and the other pair approaches it at 64°. In front of one of the 59° mirrors and one of the 64° mirrors are convex buttons that increase magnification ×1.4 and concentrate laser energy (Ritch, 1985). The Magna View lens (3‑20 and 3‑21) is a single-mirror lens that is similar to the Goldmann one-mirror lens except that it has a wider field and provides ×1.3 magnification. It was designed for the delivery of laser energy to the angle and photography.
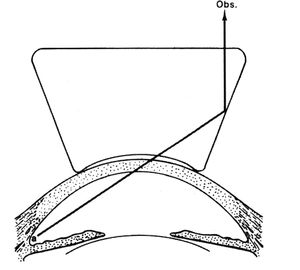
3-15 Indirect gonioscopic lenses use mirrors or prisms to it has no handle to reflect the light from the irido-corneal angle (a) so that it leaves the eye perpendicular to the face of the contact lens.


3‑16, 3‑17 Goldmann three-mirror lens. The shortest mirror is for examining the angle. The other two mirrors are for examining the peripheral retina. Like all indirect lenses, the central area can be used to examine the fundus. (Courtesy of Haag-Streit.)

3-18 Goldmann style one-mirror lens. (Courtesy of Ocular Instruments.)

3-19 Ritch trabeculoplasty laser lens. Two 59° mirrors are designed to view the inferior angle and two 64° mirrors are designed to view the superior angle. A convex button in front of one 59° mirror and one 64° mirror provides extra magnification for examination and laser treatment. (Courtesy of Ocular Instruments.)


3‑20, 3‑21 The Magna View lens is a Goldmann-like one-mirror lens. It has a broader viewing area than the Goldmann single-mirror lens and a convex anterior face that provides slight magnification. This lens was designed for the delivery of laser energy to the angle. (Courtesy of Ocular Instruments.)
The Posner lens (3‑22) has four identical mirrors that permit examination of four quadrants with no rotation of the lens (3‑23). By turning the lens through only 11°, the small areas between the mirrors can be brought into view. Because the lens has a small (9 mm) area of contact with the cornea, the angle can be deepened by pushing on the lens (indentation gonioscopy). The small gap between lens and cornea is filled with tears or topical anesthetic. This keeps the cornea free of viscous fluids and permits clear examination and photography of the optic nerve head following gonioscopy. The Zeiss lens (3‑24 and 3‑25) is similar to the Posner lens but is made of glass instead of plastic. It is no longer commercially available. The Sussman lens (3‑26 and 3‑27) is also similar to the Posner lens, except that it has no handle.
Special mention should be made of the Allen-Thorpe gonioprism (3‑28 and 3‑29), which was used in preparing all of the paintings reproduced in this Atlas (Allen et al, 1954). Rather than mirrors, this lens has four prisms. It has a flange that holds it in place (3‑30) and requires methylcellulose to couple it to the cornea. The lens is no longer commercially available.

3-22 Array of Posner four-mirror lenses with fixed handle and plastic lens. This lens has four identical mirrors for rapid gonioscopy. No methylcellulose coupling solution is required. The small area of contact allows for indentation gonioscopy. This lens is very similar to the Zeiss four-mirror lens, which is no longer commercially available. (Courtesy of Ocular Instruments.)
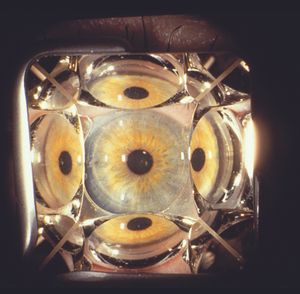
3-23 Four quadrants visible through Zeiss four-mirror lens.

3‑24, 3‑25 Zeiss four-mirror lens on Unger fork (Carl Zeiss).

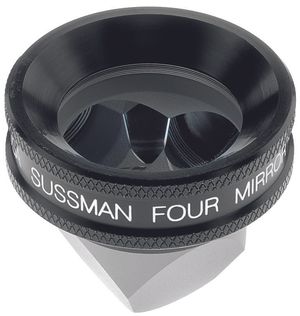
3‑26, 3‑27 The Sussman four-mirror lens is like the Zeiss or Posner lens but without a handle. Some examiners prefer to hold the lens directly. (Courtesy of Ocular Instruments.)
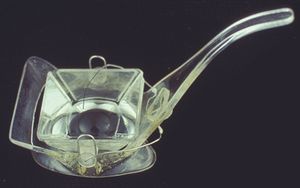
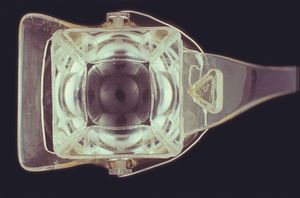
3‑28, 3‑29 Allen-Thorpe gonioprism. Four prisms permit all four quadrants to be examined. The lens is suspended in a frame by means of a fine spring that holds the prism against the cornea. The frame holds the lens between the lids. (Courtesy of Bausch & Lomb.)

3-30 The Allen-Thorpe gonioprism is held in place by its frame. Both hands are free to manipulate the slit lamp.
Comparison of Direct and Indirect Gonioscopy
Both direct and indirect gonioscopy have advantages and disadvantages.
Although direct gonioscopy is no longer widely practiced outside of the operating room, it does have certain advantages over indirect gonioscopy. Direct gonioscopy, as the term suggests, provides a straight-on view of the angle rather than the mirror image given by the indirect lenses. Direct gonioscopy permits the examiner to vary the angle of visualization more readily—to enable one to look over the curvature of iris bombé, for example. The view with direct gonioscopy is more panoramic than with indirect gonioscopy. Two Koeppe lenses may be used to compare the angles of the two eyes in order to determine whether one eye has suffered a traumatic recession.
The major disadvantage of direct gonioscopy is its inconvenience. The patient has to lie down, usually in a special room with special equipment. The inconvenience of direct gonioscopy led to the development of the van Herick system of estimating the depth of the anterior chamber based on examination by slit lamp. Van Herick stated that “In the routine examination of nonglaucomatous patients, it is impractical to perform gonioscopy” (van Herick et al, 1969). Fortunately, the convenience of indirect gonioscopy allows one to perform it quickly as part of a routine evaluation of glaucoma patients.
Indirect lenses have several advantages that have made them the preferred lenses for most ophthalmologists. The first advantage, specific to the four-mirror lenses, is that they do not require viscous coupling agents. This is particularly important if a patient is to have fundus photography at the same visit. Gonioscopy can be performed quickly with the same anesthetic as that used for tonometry. Additionally, no special equipment is required when performing indirect gonioscopy with any lens. The slit lamp serves as a source of variable magnification and illumination. The slit beam can create a corneal wedge to help to define the structures of the angle (Chapter 4 ). Indentation gonioscopy can be performed with the Posner or Sussmann lens to distinguish appositional from synechial angle closure (Chapter 4 ). Additionally, gonioscopic photography and videography can be performed in combination with indirect gonioscopy.
Indirect lenses have the disadvantage of giving a mirror-image view of the angle, which can be somewhat confusing. It is also easy to open or close the angle inadvertently by applying excessive pressure to the indirect lenses. These lenses may exaggerate the degree of angle narrowing and are less able to provide a view into the depths of a narrow angle (Shaffer, 1962). The four-mirror lens is somewhat more difficult to learn to use than the other lenses but, once mastered, is extremely convenient.
Because direct gonioscopy is rarely used in routine clinical practice, this Atlas concentrates on slit-lamp (indirect) gonioscopy. For further information on direct gonioscopy, refer to the works of Troncoso (1947), Shaffer (1962), Becker (1972), and Kimura (1974). Although these texts are no longer in print, they are available in many medical libraries.