Introduction
Treating adult patients with small-angle diplopia can be challenging. Since normal vertical and divergence amplitudes are low, acquired esotropia or any vertical deviation can cause diplopia. In many patients, especially those with a vertical component, there is some degree of incomitance. Therefore, the goal of therapy is not to "cure" diplopia entirely but rather to produce a large field of central, binocular vision to allow the patient the greatest visual function for daily tasks. The treatment for small-angle deviation in adults can be nonsurgical or surgical.
Patient management: treatment and follow-up
Nonsurgical treatment
a. Monocular occlusion
Although it successfully eliminates any binocular diplopia, monocular occlusion is almost never a good long-term treatment strategy. Otherwise poorly tolerated, it can be used as a temporizing measure as a patient anticipates spontaneous improvement or awaits surgical correction. Diplopia only while reading can be treated with occlusion of the bifocal segment of the nondominant eye.
b. Spectacles with prism
Prism correction is an acceptable solution for adult patients with small-angle strabismus causing diplopia. However, many adult patients find prism glasses unsatisfactory. For example, patients who are emmetropic, or who use contact lenses, or are status post successful refractive surgery will probably object to wearing prism glasses. Prism glasses can also cause image distortion. Moreover, a noncomitant ocular deviation renders prism correction ineffective in all but primary gaze, and the correction is therefore often not well tolerated.
Prisms can be ground into the lens or can be temporary in the form of a Fresnel prism. In general, use of prism correction is limited to adults with small-angle strabismus (traditionally less than 15∆) who already wear glasses to correct a refractive error. Fresnel press-on prisms, generally placed before the nondominant eye, can be used as a short-term treatment of diplopia, but occasionally can prove to be an effective long-term strategy. Prisms can also be used to correct residual small-angle deviation after strabismus surgery. The prisms can cover the entire lens or just the distal/near part of bifocal glasses (Figure 1). Ground-in prisms are generally used as a long-term strategy. Higher amounts of prism induce visual distortion and are heavy, which may limit use for some patients.

Figure 1. Bifocal glasses with prism correction using Fresnel press-on prisms for near work on the right (nondominant) eye. No correction is needed for distance.
c. Orthoptics
In general, orthoptic exercises are most appropriate for young adults with intermittent exotropia or convergence insufficiency. Consistent and frequent use of convergence exercises can significantly reduce symptoms of asthenopia and improve control of the deviation in many patients. High compliance is needed for clinical success. Some computer-based exercises require binocular vision and should not be given to patients without binocularity. Orthoptic eye exercises for any other clinical conditions remain unproven, although there are anecdotal and nonrandomized studies that report success with small angles of esotropia and vertical deviations.
d. Botulinum toxin
Most ophthalmologists prefer standard strabismus surgery to the use of botulinum toxin. The use of botulinum toxin for treating eye misalignments, first described by Alan Scott, has gained popularity in some forms of strabismus, with acute 6th nerve palsy being the most common indication.1 Botulinum toxin may also be particularly useful in situations where strabismus surgery is undesirable. This might be the case in patients unfit for general anesthesia, when the clinical condition is unstable or temporary, or if surgery is prone to fail or has already failed. Typical dosing of botulinum in the treatment of strabismus is 1.25-5 units into any one muscle. Higher dosages can be injected in a previously injected muscle or when the extraocular muscle is bigger, such as in thyroid eye disease. The frequent need for repeated treatment is a limiting factor in its acceptance.
Botulinum toxin can be injected under direct visualization during strabismus or decompression surgery, or in an office under topical anesthesia using electromyographic (EMG) guidance (Figure 2) to confirm correct placement of the injection into the muscle. The effect of the toxin will typically start to be seen within 2–4 days of the injection; it then causes an expected overcorrection for some weeks due to the contracture of the antagonist muscle. This will result in stretching of the injected paralyzed muscle. The toxin wears off after 6–8 weeks; in many cases, it leaves a permanent realignment. This "stretching" will cause a histologic change in the sarcomere density and the length-tension curves within the muscle. Therefore, as the effect of the toxin wears off, some of the changes persist, resulting in a permanent net change to the alignment.2
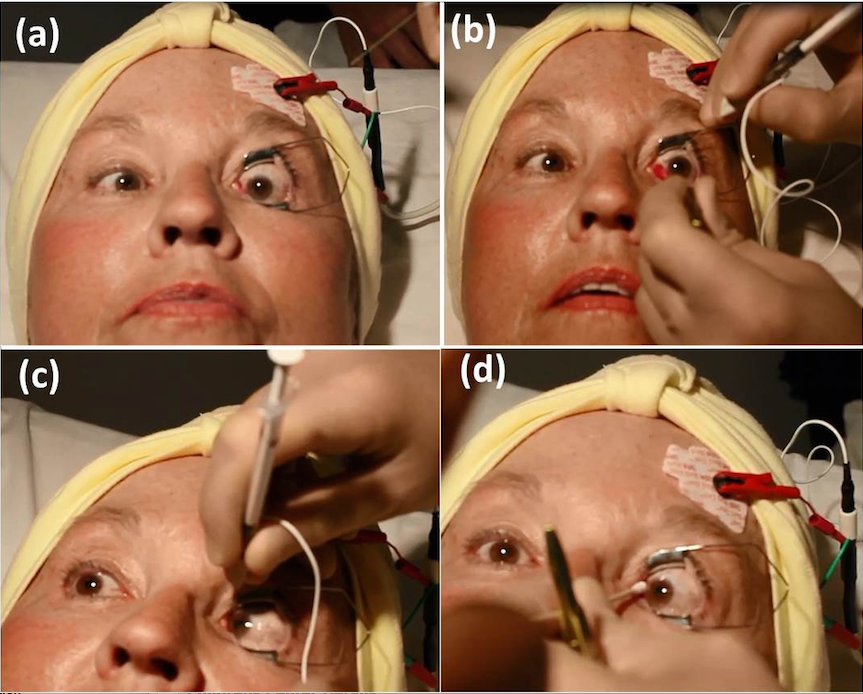
Figure 2. An example of electromyographic (EMG) guided botulinum toxin (BT) injection to the left medial rectus (LMR) under topical anesthesia.
(a) A lid speculum is placed. A metallic 27G needle is used, and an electrode is placed on the patient’s forehead, then attached to the electromyogram. (b) Patient is asked to look in the opposite direction to the action of the muscle being injected (In this case, it is left gaze. Forceps can be used). The needle is inserted through the conjunctiva, superficial to the sclera, and into the target muscle. (c) When the needle is in the muscle, the patient is asked to look in the direction of action of the muscle being injected (In this case, it is right lateral gaze. Note a restriction in the right eye). If the needle is correctly positioned, there will be an audible increase in signal output from the EMG. Then the toxin is slowly injected to the muscle. (d) The needle is carefully removed with the help of an applicator. The patient is immediately seated to avoid penetration of the toxin to the levator palpebrae muscle, which can cause ipsilateral ptosis.
Surgery
This section does not describe the conventional strabismus procedures, typically performed for deviations that are 15∆ or more; it focuses instead on techniques that were specifically designed to correct small-angle deviations.
a. Rectus muscle tenotomy
Rectus muscle tenotomy was described as far back as the 1800s.3 This surgical technique had been abandoned until Scott introduced the "graded muscle tenotomy" in 20004 and Wright modified it (the "central tenotomy") in 2009.5 In the former, the muscle is cut, leaving one portion of the tendon attached its original insertion and the other disinserted. The authors find this "slanted" tenotomy to be very useful in situations with incomitant strabismus. For example, a left hypertropia that is worse in right gaze but shows no evidence of left inferior oblique overaction can be treated with a right inferior oblique temporal side cut.
The central tenotomy involves cutting the central 3-4mm of the rectus tendon at the insertion (specifically the inferior or media rectus) (INSERT Movie). Care should be taken not to cut the ciliary arteries. Wright reported correcting an average of 2.3∆ of vertical deviation with an inferior rectus central tenotomy and 1.3∆ of esotropia with medial rectus central tenotomy. A bilateral central tenotomy can correct twice as much. The original article by Wright described performing it under local anesthesia in office through an intact conjunctiva with minimal complications. However, the surgery can be performed in the operating room using conventional techniques. For example, a patient who has a medium-to-large degree of esodeviation and small right hypertropia will notice vertical diplopia after the horizontal deviation has been corrected with prisms. A routine bimedial recession will be combined with left inferior rectus central tenotomy under direct visualization of the muscle and ciliary vessels, leading to resolution of both horizontal and vertical diplopia. If done in office, care should be taken to avoid scleral perforation (especially if not using blunt scissors), cutting a ciliary vessel, or cutting the entire rectus muscle from its insertion. Using this method under direct visualization, complications and overcorrections can be avoided. In the case of undercorrection, a standard strabismus surgery can be done to treat the consecutive deviation.
b. The inferior oblique "Z myotomy"
A "Z myotomy" of the inferior oblique can correct small symptomatic diplopia and asthenopia caused by mild inferior oblique muscle overaction (IOOA≤+2). This form of misalignment can result in patient frustration since its incomitant nature leads to differing degrees of deviation in different gaze positions. As discussed previously, prism correction is less than ideal in this situation because diplopia can be eliminated in only one gaze position. Classically, when IOOA is present, there is an ipsilateral hypertropia in primary gaze that worsens in contralateral gaze due to greater upward excursion of the adducted eye compared to the abducted eye. The most common surgical approaches to treat IOOA are inferior oblique recession or myectomy, and the choice is heavily influenced by individual surgeon experience and preference. These surgical options have the potential of overcorrecting small incomitant hypertropias or minimal IOOA (≤+2). The inferior oblique “Z-myotomy” lengthens the inferior oblique less so than conventional recession or myotomy and, although known for over 40 years, has not gained popularity and is not widely performed.
Figure 3 demonstrates the basic surgical steps of an inferior oblique (IO) Z-myotomy. The advantages of IO "Z-myotomy" include that it is easy to perform; quick (5-7 minutes per inferior oblique muscle in our experience); does not involve sutures; maintains the original muscle insertion, thereby decreasing risk to the nearby macula; can be "augmented" (with recession or myectomy) in the future if needed; appears to be self-setting to the amount of correction needed; and presents a very small risk for symptomatic overcorrection.
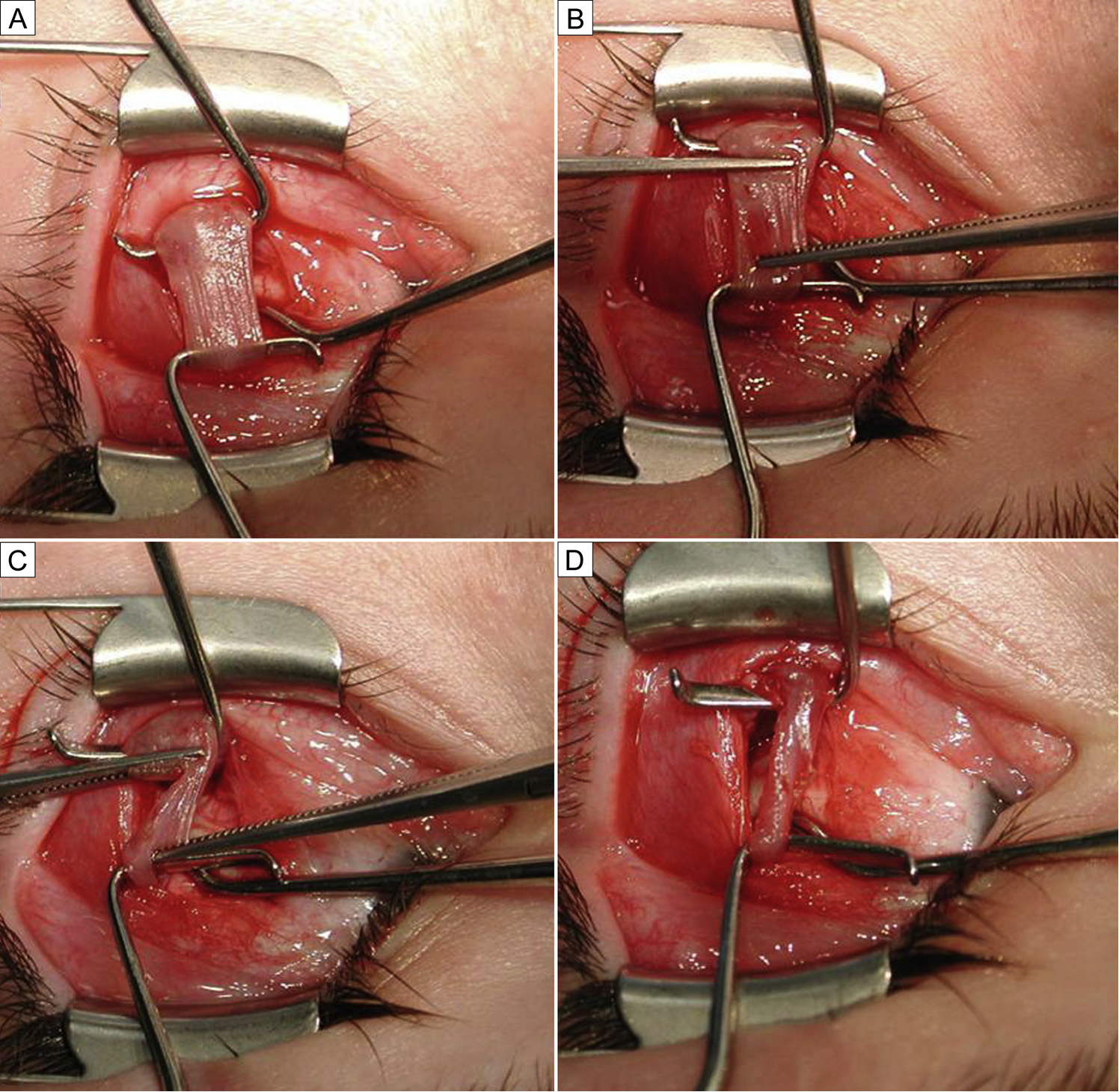
Figure 3. The "Z myotomy". (a) The inferior oblique is isolated and stretched between 2 Green hooks. (b) Two opposing straight Jake clamps (approximately 10 mm from each other) are placed, each encompassing approximately 75% of the muscle belly, isolating 50% of the muscle belly between the two muscle clamps. (c) Westcott scissors are used to cut the muscle across the Jake clamps distal to the direction of blood flow (closest to the insertion) to optimize hemostasis. The cut edges of the muscle are then cauterized using a low temperature heat cautery. (d) Inferior oblique appearance after a "Z myotomy."
Recently, several authors have reported their results in treating symptomatic vertical deviation due to mildly overacting inferior oblique, but one group reported the largest cohort, with 38 patients.6 According to that experience, a "Z myotomy" would be considered for correction of a vertical deviation of up to 6 prism diopters in primary gaze (although it can be used for larger deviations in patients with good fusion). When bilateral mild IOOA is present, bilateral "Z myotomy" can be considered. When IOOA is asymmetric, an inferior oblique recession can be performed on the side where IOOA is more pronounced and a "Z myotomy" on the less over acting inferior oblique. When the deviation in primary gaze is larger than a pure "Z myotomy" can fix (eg, larger than 6 prism diopters), a contralateral inferior rectus recession can be performed. Thus, the IO "Z myotomy" improves the incomitance and the inferior rectus recession improves the rest of the deviation.
c. Mini plication
When a tightening procedure is needed for small horizontal deviation, the "mini-plication" developed by Wright can be performed.7 This procedure can correct 5-10∆ of horizontal deviation and can be done in an office setting. Here, instead of plicating the entire muscle like traditional plication, only the central part of the muscle is being shortened using a Vicryl suture. This procedure is recommended for patients with small horizontal deviation, usually less than 15∆. The advantages of this procedure over a standard tightening procedure are that it does not require hooking and removing the muscle, and it preserves the integrity of the muscle insertion and presumably the anterior ciliary vessels. It can also be done with topical anesthesia and can be reversed.
d. Small angle surgery with adjustable suture
Small-angle strabismus can also be addressed with a standard eye muscle surgery on a single muscle using adjustable sutures. Basically, the deviation is doubled and the full dosage for a bilateral surgery is performed unilaterally. For example, a patient with 10∆ esotropia will undergo a unilateral medial rectus recession of 3.5 mm (the amount of bilateral medial rectus recession for esotropia of 20∆) or a unilateral lateral rectus resection of 4.5 mm (the amount of bilateral lateral rectus resection for esotropia of 20∆). In either case, an adjustable suture will be placed.
References
- Coats DK. Adult Strabismus. Focal Points. San Francisco: American Academy of Ophthalmology; 2009: 27 (12).
- Kowal L, Wong E, Yahalom C. Botulinum toxin in the treatment of strabismus. A review of its use and effects. Disabil Rehabil. 2007; 29:1823-1831.
- von Noorden GK. Strabismology from its beginnings to the middle of the 19th century. In: von Noorden GK, ed. The History of Strabismology. Oostende, Belgium: JP Wayenborgh; 2002:41-46.
- Scott AB. Graded rectus muscle tenotomy for small deviations. In: Proceedings of the Jampolsky Festschrift 2000; San Francisco: The Smith-Kettlewell Eye Research Institute:215-216.
- Wright KW. Mini-tenotomy procedure to correct diplopia associated with small-angle strabismus. Trans Am Ophthalmol Soc. 2009; 107:97-102.
- Cruz FC, Robbins SL, Kinori M, Acera EC, Granet DB. Z-myotomy of the inferior oblique for small incomitant hypertropias. J AAPOS. 2015; 19:130-134.
- Leenheer RS, Wright KW. Mini-plication to treat small-angle strabismus: A minimally invasive procedure. J AAPOS. 2012; 16:327-330.