This chapter was revised by the author on July 22, 2020.
Introduction
Duane retraction syndrome (DRS) is a unique restrictive variety of strabismus that is present from birth. It is characterized by co-contraction of the medial and lateral rectus muscles due to anomalous innervation of the lateral rectus muscle during embryogenesis.
It was first described by Heuck in 18791 and subsequently by several other authors, including Stilling in 1887,2 Sinclair in 1895,3 Mac Lebose in 1895,4 and Türk in 1899.5 The condition is named Stilling-Türk-Duane syndrome but is most commonly known as Duane retraction syndrome. In 1905, Duane published a landmark paper describing 54 cases in detail (of which 16 were his own), including the unique features of the syndrome, of which the most prominent was the retraction of the globe in adduction.6
This syndrome is characterized by variable limitation or absence of abduction, variable restriction of adduction, and retraction of the globe with narrowing of the palpebral fissure on adduction (Figure 1). These manifestations are frequently associated with abrupt elevation or depression of the eye in adduction, commonly known as upshoot and downshoot (Figure 2, Videos 1 and 2).
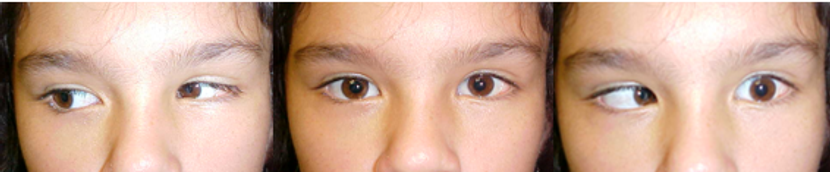
Figure 1. Patient with DRS on her left eye, limitation of abduction and narrowing of the palpebral fissure in adduction.

Figure 2. Same patient as in figure 1, showing upshoot and downshoot.
Video 1. Upshoot and downshoot
Video 2. Upshoot and downshoot
Epidemiology
Duane retraction syndrome (DRS) is one of the most common types of specialized strabismus; the overall prevalence of DRS in strabismic patients has been estimated between 1% and 4%.7,8,9
Most of the studies published on this condition point to a 60% female preponderance in patients with unilateral disease.10 This female preponderance seems not to be present in bilateral cases.11 The left eye is affected in two-thirds of unilateral cases.12
The female preponderance is explained by Parsa and Robert in the hypothesis that during embryogenesis, higher estrogen levels, along with a greater risk of inflammation, predispose the female fetus to venous thromboembolic events. These phenomena (in addition to right-to-left shunting creating more embolic events affecting the left carotid artery) result in dysregulated apoptosis, followed by misinnervation and ocular malformations.13
Bilateral cases represent 15% to 20% of all cases with DRS. The eyes can be asymmetrically affected in these cases (Figure 3).11,12

Figure 3. Bilateral DRS patient, adduction more affected on the left eye.
Considerations on the etiology of Duane Syndrome
Duane retraction syndrome is most likely a spectrum of mechanical, anatomical, genetic, and innervational disorders of the extraocular muscles.
Mechanical disturbances can occur as a result of the presence of fascial bands, which are occasionally found in cases of DRS (Figure 4).14 These bands act as a leash and cause limitation of the eye movement. Contracture or shortening of the muscles has also been documented.
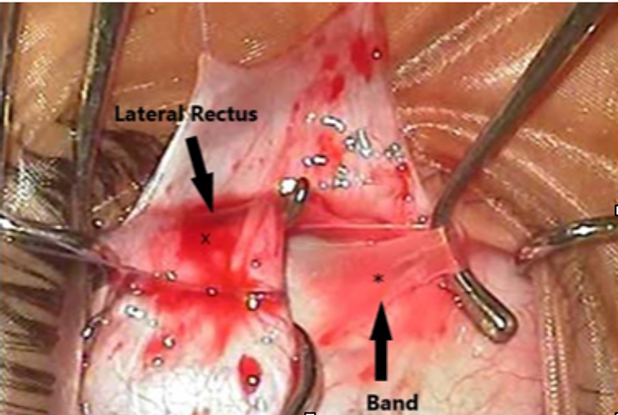
Figure 4. Fascial band observed underneath the lateral rectus in a DRS patient. (Courtesy Dr. Suma Ganesh, Shroff’s Charity Hospital, New Delhi)
Anatomical changes are also commonly seen in DRS cases, including fibrotic changes in the lateral or medial rectus muscles and anomalous insertions.15 Bifid lateral rectus muscles and hypoplastic changes in the muscle have also been described.16 Some of the anatomical anomalies could also occur as a result of a primary innervational anomaly.
Hereditary factors have been postulated as early as 1879 by Heuck.1 Family cases of the syndrome have been reported by many authors in the past, but in most of these reports the incidence represents about 10% of all cases.17,18
Several gene loci related to DRS have been mapped. In cases of DRS without systemic involvement, the DURS1 locus on chromosome 2q31 has been identified.19 An autosomal dominant variant of DRS has been associated with mutations of the CHN1 gene. Mutations in the DURS2 gene appear to affect primary development of the abducens and, to a lesser degree, the oculomotor nerve.20
Studies of sporadic forms of DRS showed a 10–20 times greater risk for having other congenital malformations divided in mainly 4 categories: skeletal, auricular, ocular, and neural.21
A gene responsible for DRS and a dominant form of hydrocephalus has been identified and is located close to a gene causing the branchio-oto-renal syndrome.22 It has been postulated that the gene responsible for the disease is incompletely penetrant, with variable expressivity.23 Another syndrome associated with the DRS is the Duane radial ray syndrome also known as Okihiro Syndrome. The eye movement abnormalities are associated with abnormalities of the bones in the arms and hands. It is caused by several mutations in the transcription factor of SALL4.24,25
The most important determining factor for the clinical features noted in DRS is produced by the innervational anomalies seen in this disease. Duane retraction syndrome is currently categorized among the congenital cranial dysinnervation disorders.26
The frequent association with other congenital anomalies, suggests a teratogenic event (genetical or environmental) occurring between the fourth and eighth weeks of gestation as a possible etiology for this syndrome. This teratogenic event affects the normal development of the VI nerve. It is still not clear as to whether this anomaly has a nuclear or supranuclear origin.
High resolution magnetic resonance imaging (MRI) scans in these patients have demonstrated that the abducens nerve can be absent; the abducens, oculomotor, and optic nerves can all be hypoplastic. Matteuci was the first to report hypoplastic abducens nucleus with absent sixth nerve on the affected side in 1 DRS type I patient.27 In 1998 Parsa and colleagues demonstrated the absence of left sixth nerve in a case of unilateral DRS, using high-resolution T1-weighted images on magnetic resonance imaging.28
As seen in other congenital cranial dysinnervation disorders, the deficient innervation of the lateral rectus is substituted by another cranial nerve; in DRS, this involves branches of the oculomotor (III) nerve (Figure 5). Thus, the lateral rectus is not only abnormally innervated by the third cranial nerve but can also be subnormally innervated by the corresponding sixth cranial nerve.
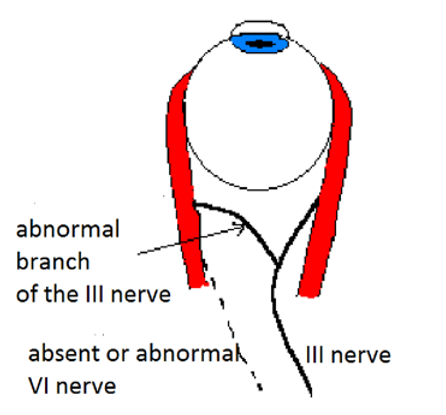
Figure 5. The absent or deficient innervation of the lateral rectus by the VI nerve is replaced by an abnormal branch from the III nerve.
Hoyt and Nachtigaller believed that the proximity of the third and sixth nerves as they pass through the cavernous sinus and enter the orbit provide many theoretical opportunities for an intermingling of their axons.29
The abnormalities seen in DRS are primarily related to this paradoxical innervation of the lateral rectus muscle. The multiple different clinical scenarios seen in these patients will be determined by how much normal or abnormal innervation the lateral rectus receives and at what position of the horizontal movement of the eye the abnormal innervation is initiated.
Electromyographic Studies in Duane Syndrome
Electromyography has been very helpful in explaining the different features seen in DRS, but these studies do not explain the underlying etiology. Breinin was the first to describe the absence of electrical potentials in the lateral rectus muscle on abduction and the presence of action potentials on adduction.30 Many other electromyographic studies on DRS followed Breinin’s paper, demonstrating the different degrees of anomalous innervation to the lateral rectus during adduction and the different action potentials of the lateral rectus muscle in abduction, ranging from no activity to equal activity in adduction versus abduction.31 Further studies also demonstrated that the paradoxical innervation of the lateral rectus comprises variable synergistic innervation, not only in conjunction with the medial rectus, but also with the superior rectus, inferior rectus, or both.32
Classifying Duane Syndrome
No single classification appears to be totally satisfactory for DRS. This syndrome presents with a wide spectrum of clinical findings, making classification difficult. A management-based classification should include not only the ocular duction deficits, but all the other diverse patterns present in this condition.
Several classification schemes for DRS were proposed, but no single categorization satisfactorily encompasses the diversity of the many forms of DRS observed clinically. The approach proposed by Huber in 1970 is based on data obtained in electromyographic studies33 and is widely accepted by most clinicians. This classification has remained popular because it utilizes a clinical description of the major clinical findings but does not distinguish between the many innervational variants of the syndrome.
He classified DRS in 3 different types:
Type I, where abduction is more limited than adduction (Figure 6).
Type II, where adduction is more limited than abduction (Figure 7).
Type III, where both abduction and adduction are limited. (Figure 8).

Figure 6. Duane type I: abduction more limited than adduction.

Figure 7. Duane type II: adduction more limited than abduction.
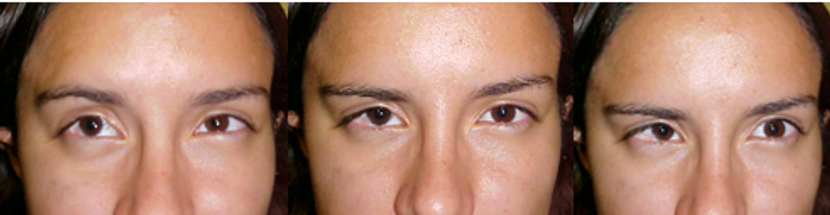
Figure 8. Bilateral Duane type III: abduction and adduction similarly limited.
In type I cases, the lateral rectus receives little or no innervation from the sixth cranial nerve and paradoxical innervation from the third cranial nerve.
In type II cases, the lateral rectus is inappropriately innervated by the third cranial nerve, and subnormally innervated by the sixth cranial nerve. Nemet and Ron have shown that the anomalous contraction of the lateral rectus in adduction occurs at different angles of adduction; this might help explain the different degrees of limitation of adduction in this type of DRS.34 The amount of fibers that abandon the innervation of the medial rectus to supply the lateral rectus is variable. The more fibers innervate the lateral rectus instead of the medial rectus, the more exotropic the patient will be, and the more limitation of adduction will be encountered.
Type III cases represent a severe form of type I case in which there is no normal sixth nerve innervation to the lateral rectus muscle. The inappropriate innervation by the third cranial nerve to the lateral rectus is so severe that it prevents the globe from moving from the primary position into adduction.
Patients with unilateral type I DRS have esotropia more frequently than exotropia, those with type II have exotropia and those with type III have esotropia and exotropia occurring equally common.
Type I is by far the most common variety (78%), followed in order of frequency by type III (15%) and type II (7%), according to the data from different authors as compiled by DeRespinis and coworkers.12
Huber’s classification has been useful for many years and is still widely used in many places. A better classification, that is more clinically oriented, is the one based on the type of deviation in primary position. This classification divides the cases into orthotropic-Duane, esotropic-Duane and exotropic-Duane and is more relevant than Huber’s classification when planning a surgical treatment of these cases (Figure 9).

Figure 9. Top row: Patient with orthotropic-Duane. Middle row: Patient with esotropic-Duane. Bottom row: patient with exotropic-Duane.
The use of this classification should be accompanied by a detailed description of the other associated ocular findings.
Clinical Manifestations of DRS
The clinical manifestations in DRS can be quite variable and will depend upon the wide array of innervational abnormalities of the lateral rectus that can occur in these patients.
The most important clinical features recognized in these patients include the following:
- Strabismus: Although many patients with DRS can be orthophoric in primary position, many patients are esotropic and a few can be exotropic (Figure 9). In some cases, a hypertropia may occur in addition to the horizontal deviation due to a concomitant IV nerve palsy or a superior rectus overaction/contracture syndrome (Figure 10).35,36 The deviation in esotropic patients is usually less than 30 prism diopters in unilateral cases with the non-affected eye fixating.34

Figure 10. Patient with bilateral DRS and right superior rectus overaction/contracture syndrome
- Alterations in Ocular Rotations: A deficit in abduction is usually the most prominent finding and represents the most frequent reason for consultation in patients with DRS. This abduction deficit can be very variable ranging from -4 (the eye not crossing the midline) to a normal abduction (Figure 11). The amount of limitation of abduction will depend partly on the amount of co-contracture of the medial rectus muscle, but even more importantly will depend on the degree of existing normal sixth nerve innervation to the lateral rectus muscle. Very often the degree of abduction deficit seems out of proportion to the degree of esotropia in primary position. Deficits in adduction to different magnitudes are also common in DRS, mainly due to the co-contraction of the lateral rectus muscle in attempted adduction.

Figure 11. Variable degree of abduction deficit in the left eye of 3 patients with DRS.
- Eyelid Fissure Changes and Globe Retraction: Narrowing of the palpebral fissure in adduction occurs as a result of passive movement of the eyelids over the retracting globe but is also due to a decrease in electrical activity seen in the levator muscle on adduction, as demonstrated by simultaneous electromyographic recordings of the levator and medial rectus muscles.37 The vertical rectus muscles can also co-contract with the lateral rectus muscle, causing an even more pronounced globe retraction.
- Compensatory Head Posture (CHP): A compensatory head posture is almost always present in patients with DRS who do not have their eyes aligned in primary position. This compensatory mechanism helps the patient to achieve binocular single vision. The head turn will be toward the side of the affected eye in esotropic-Duane and away from the affected eye in exotropic-Duane cases (Figure 12). The magnitude of the compensatory head posture is variable and dependent upon the amount of deviation in primary position.

Figure 12: Top row: Face turn directed to the left affected eye in eso-Duane. Bottom row: Face turn opposite to the right affected eye.
- Upshoots and Downshoots: Upshoots and downshoots are sudden vertical deviations that occur in DRS patients when the eye begins to move up or down in the adducted position. These abnormal vertical movements have been attributed to mechanical and innervational causes. The mechanical explanation for this phenomenon was simultaneously described by Alan Scott and Carlos Souza Dias at a joint symposium of the Consejo Latinoamericano de Estrabismo (CLADE) and the Smith-Kettlewell Eye Research Institute in 1976. They have attributed this movement to the sideslip of the tight lateral rectus muscle as the globe moves above or below the horizontal plane in adduction. This has been termed the “bridle effect.” These vertical movements can be so severe or disfiguring as to become the most important complaint in DRS patients. They are more commonly seen in type II or III patients in which the co-contraction of the horizontal muscles is very severe. The intense co-contraction of both horizontal muscles will produce a significant retraction of the eye when it is in primary position, but as soon as the eye moves a little up or down from the horizontal plane, it will escape the retraction by moving fast up or down, causing the up or down shoot. (Video 1, Video 2)
Innervational causes can be responsible for some cases of anomalous vertical movements and can be produced by abnormal synergistic innervation between the medial rectus muscle and the superior, inferior rectus, or oblique muscles as demonstrated electromyographically in the studies of Scott and Wong.38 These findings can also be produced by coexisting oblique muscle dysfunction. The vertical movement observed in underlying mechanical strabismus is different from that observed in cases with an innervational etiology. When a mechanical cause is involved, the vertical movement is abrupt; when an innervational etiology is the cause of the vertical movement, this vertical deviation steadily increases as the eye moves from abduction to adduction. Patients with innervational causes more frequently have coexisting vertical deviation in primary position (Figure 13). Some patients display only upshoots, others downshoots, and others both anomalous vertical movements; in these last cases, these movements can be asymmetrical or symmetrical.
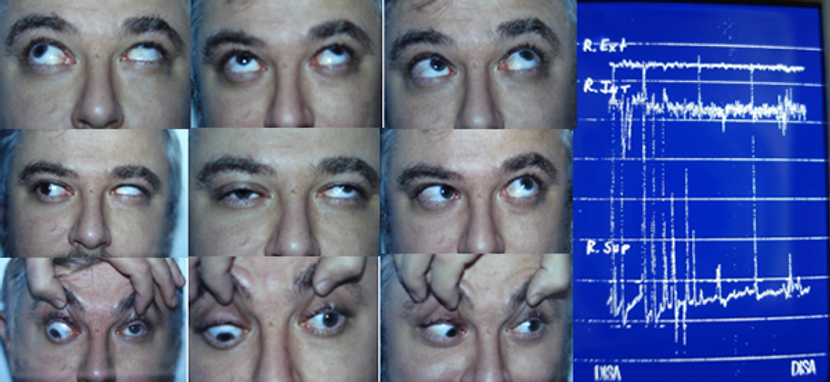
Figure 13. Patient with exo-Duane and left hypertropia due to anomalous co-contraction of the left medial rectus and left superior rectus as seen in the electromyography study of the patient. (Courtesy Maria Cristina Ugrin, MD)
- Alphabetical Patterns: A large incidence of increased innervation of the lateral rectus in elevation or depression explains the frequent observation of X, V, or A patterns in these patients (Figure 14). These patterns can be explained by the co-contraction of the vertical and lateral recti when the patient is looking toward the affected field of gaze, and they have been demonstrated in some electromyographic studies in some of these patients. The V pattern was the most common alphabetical pattern found in a series of 101 patients with DRS, 75% in the study of Isenberg and Urist; the A pattern and no pattern were found less frequently, except in bilateral cases of DRS, where A patterns seem to be more frequent.39 Bilateral cases are also more likely to be associated with alphabetical patterns.40

Figure 14. V pattern, A pattern and X pattern.
- Sensory Anomalies: Most patients with DRS adopt a compensatory head turn when the eyes are not aligned in primary position to maintain single binocular vision. Even if suppression can be seen in some patients, most of them are aware of a second image when questioned, but they usually tend to ignore this second image. In a study of 22 patients with DRS, Sloper demonstrated that patients over 5 years of age have a reduced stereoacuity in the absence of amblyopia. He hypothesized that this is probably a consequence of abnormal visual experience caused either by intermittent ocular misalignment or reduced oculomotor co-ordination.41 The range of amblyopia in Duane syndrome was from 3% to 25%, with the weighted average being 14% among studies. Amblyopia was mainly due to strabismus and not to anisometropia.12
Examining a Patient with Duane Syndrome
As with any other strabismic patient, determining vision, motility, binocular status, and refraction represents the initial steps in evaluating a patient with DRS. Most studies that have examined the refraction in DRS patients have shown that hyperopia is the most common refractive error observed.12
Most patients with misalignment in primary position will adopt a compensatory head posture in order to maintain binocularity; therefore, strabismic amblyopia is not a common feature in patients with unilateral DRS. Amblyopia is more frequently noted in patients with bilateral DRS: it was found in 25% of patients bilaterally affected in the study of Urist and Isenberg.39
Careful evaluation of the ocular ductions to look for anomalous vertical movements is very important, as this information is critical in determining the optimal surgical strategy in each case. It is also important that the patient maintain a neutral head posture so the examiner can recognize the various associated motility disorders.
Measuring the eyelid fissure in adduction and abduction is important in order to determine the degree of globe retraction. This represents an indirect sign of the amount of anomalous innervation to the lateral rectus muscle. A greater degree of anomalous innervation is correlated with an increased amount of globe retraction.
When examining eye rotations, it is important to look for:
- Abduction and adduction deficits
- Alphabetical patterns
- Anomalous vertical movements (upshoots and downshoots)
Abduction deficit can vary from no abduction at all (the eye not passing the midline) to almost complete abduction. Two factors will be responsible for this limitation: the amount of normal innervation to the lateral rectus and the degree of contracture of the medial rectus that will not allow the globe to abduct. Differentiating these 2 components of the abduction limitation can be determined with the forced duction test and the forced augmentation test as described by Jampolsky.42 This test compares the voluntary abduction end-point with the possible extension of this end-point by forcing further abduction manually with a forceps. The force generation test can also be very useful in helping to determine the amount of active force generated by the lateral rectus.
Adduction is not affected in most patients with DRS but will be significantly reduced in the few cases of type II Duane with large exotropia in primary position and in type III cases in which adduction and abduction are equally compromised. In these cases, the lateral rectus receives a large amount of abnormal innervation that will prevent the eye from moving into adduction. This abnormal innervation of the lateral rectus can be determined by the force degeneration test as described by Romero Apis.43 This test will demonstrate anomalous lateral rectus innervation as the eye goes into adduction, and is performed as follows: The patient is asked to look halfway between primary position and full adduction and then, grasping the temporal limbus with a forceps, the examiner attempts to move the eye further into adduction while the patient is asked to further adduct the eye. Resistance caused by the co-contracting lateral rectus in adduction can often be appreciated at this point. Then the patient is asked to abduct the eye, and grasping the eye again at the temporal limbus, the examiner attempts to adduct the eye. It can be noted that the resistance has disappeared or diminished, since in attempted abduction the lateral rectus does not receive the abnormal innervation from the third nerve.
The alphabetical patterns seen in these patients are usually not elicited by oblique dysfunctions but rather by co-contraction of the lateral and vertical rectus muscles. The V pattern was the most common alphabetical pattern noted in a series of 101 patients with DRS (75% in the study of Isenberg and Urist). In this study, A pattern and no pattern were noted equally.38 Some patients can also present with X pattern.
In order to accurately measure the angle of the deviation in patients with DRS, it is imperative to control the fixating eye during alternate cover measurements. The secondary deviation (when the Duane syndrome eye is fixing) will always be larger than the primary deviation, as in paretic muscle disorders (Figure 15). The patient will always seek the preferred head position in order to avoid diplopia and maintain binocularity. The examiner places the prism over the affected eye and performs a cover-uncover on the non-affected eye, changing the prism on the affected eye, until no movement is observed in this eye. Deviations may vary and be different for distance versus near fixation, right gaze versus left gaze, and upgaze versus downgaze.

Figure 15. Patient fixing with the right healthy eye and fixing with the left Duane eye.
The fact that DRS is frequently associated with other ocular and systemic congenital anomalies demonstrates the necessity of performing a thorough ocular examination. Systemic malformations, especially hearing defects, must always be excluded by a general physical examination in DRS patients.
Differential Diagnosis
The diagnosis of Duane retraction syndrome is usually not difficult, because the clinical features of the disease are very specific, but sometimes these features can be very subtle and pose some uncertainties.
The differentiation between an esotropic-Duane patient with limitation of abduction and minimal retraction and a patient with congenital sixth nerve palsy can be difficult, especially in very young children.
The main differences between a sixth nerve palsy patient and an esotropic-Duane patient will be the following:
- There is an absence of retraction with attempted adduction in sixth nerve palsy.
- The esotropic angle is usually smaller in DRS patients compared with sixth nerve palsy patients who have the same limitation of abduction.
- No vertical anomalous movements are seen in sixth nerve palsy
- Deficiency of abduction is less pronounced in elevation and depression in DRS, while it remains the same in sixth nerve palsy patients.
Patients with exotropic-Duane can also pose some confusion with patients with third nerve palsy but again, no retraction or anomalous vertical movements are noted in patients with third nerve palsy.
Other strabismic entities that can pose a diagnostic dilemma with DRS are:
- Ciancia syndrome
- Congenital exotropia
- Oculomotor apraxia
- Moebius syndrome
- Traumatic restrictive strabismus
- Accessory extraocular muscles
In most of these cases the presence of globe retraction and anomalous vertical movements will clarify the diagnosis.
The presence of anomalous extraocular muscles, especially in those cases in which the anomalous orbital structure is inserted close to the optic nerve and runs posteriorly toward the orbital apex, will make the differential diagnosis challenging. These cases also present with globe retraction and variable limitation of eye movements. In these cases, orbital imaging will often be helpful in making the correct diagnosis. (Figure 16)
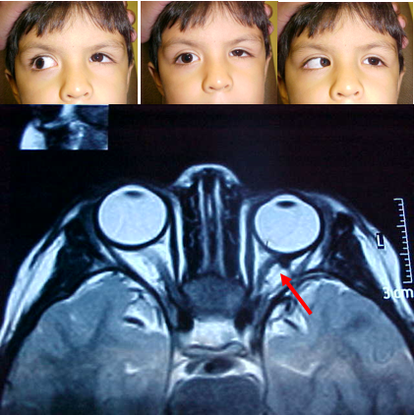
Figure 16. Patient with enophthalmos and limitation of eye movements due to an accessory extraocular muscle (arrow).
Ocular and Systemic Associations of Duane syndrome
DRS is a disease in which the chance of finding other anomalies is significant. Pfaffenbach and colleagues found an incidence of 33% of 1 or more congenital anomalies among his series of 186 patients with DRS.21 In this same study, the rates of musculoskeletal, foot, and ear anomalies found in these patients with DRS was 10 to 20 times higher than in the general population.
Among the most frequent ocular malformations found in DRS are:
- Dysplasia of the iris stroma
- Pupillary anomalies
- Cataracts
- Heterochromia
- Colobomas
- Nystagmus
- Epibulbar dermoids
- Ptosis
- Optic nerve hypoplasia
Other dysinnervation disorders described in patients with DRS include:
- Crocodile Tears syndrome: In this anomaly, accessory branches from the gustatory nerve end erroneously in the lacrimal gland, which is abnormally innervated. The patient does not tear under normal stimulus but does produce tears with gustatory stimuli.44
- Marcus Gunn Jaw-Wink syndrome: in this syndrome, nerve fibers usually directed to the muscles of mastication end erroneously in the levator muscle. The eyelid of the patient moves when the patient uses the muscle of mastication while chewing or breastfeeding. (Videos 3 and 4)
Video 3. Marcus Gunn Jaw-Wink syndrome
Video 4. Marcus Gunn Jaw-Wink syndrome
The most associated affected areas in DRS are the central nervous system, the head and face, and the limbs. The more frequently encountered anomalies are:
- Preauricular tags
- Cervical spina bifida
- Chiari type I malformation
- Cleft palate
- Thenar hypoplasia
- Rib anomalies
- Foot anomalies
- Sensorineural hearing deficits
The most frequently associated syndromes observed in DRS are:
- Goldenhar syndrome
- Klippel-Feil syndrome
Combined abnormalities of the vertebral column and limbs, ear defects, and other ocular malformations with DRS are known as Duane plus.
All organs or structures commonly affected with DRS develop during the second month of gestation, making it seem likely that a common teratogenic factor may be responsible for these alterations. This hypothesis is reinforced by the fact that some studies have demonstrated a high incidence of DRS in thalidomide embryopathy.45
Patient Management: Treatment and Follow-Up
Treatment of Duane Syndrome
Nonsurgical treatment in Duane syndrome includes treatment of amblyopia, if present. In cases with a small compensatory head position, prisms can be prescribed to normalize the head posture or to manage intermittent diplopia, if needed.
In most patients with DRS, surgical treatment is not indicated. Surgical treatment can produce disappointing results; therefore, it is advisable not to operate on patients with normal binocular vision in primary position that do not have disfiguring globe retraction or anomalous vertical movements, or in cases in which the binocular vision can be maintained with a slight face turn. The patient must be informed that there is no treatment or surgical procedure that will restore normal ocular movements in all gaze positions. Surgery does not eliminate the fundamental abnormality of innervation.
Most ophthalmologists agree that the indications for performing a surgical correction in DRS patients include the following:
- Noticeable ocular deviation
- Marked anomalous head posture
- Disfiguring retraction of the globe on attempted adduction
- Cosmetically unacceptable vertical deviation of the eye in adduction
There are no rigid rules regarding surgical treatment of this syndrome; each case should receive individualized consideration according to the clinical manifestations observed.
The major goals in the surgical treatment of DRS are:
- Improve an anomalous head posture
- Correct any angle of strabismus in primary position
- Improve globe retraction
- Expand binocular field of single vision
The clinical variants to consider for choosing the most appropriate surgical strategy for each case include:
- Abduction and adduction capacity (detecting any normal innervation on the lateral rectus)
- Degree of retraction
- Possible anomalous innervation to vertical recti causing upshoots and downshoots
- Angle in primary position
- Anomalous head posture
- Presence of anomalous vertical movements
- Outward rotation of the eye in upgaze or downgaze that is due to the LR increasing or recruiting more motor neuron activity when looking up or down
- Contractured muscles detected by forced duction testing
The surgical procedures commonly used in these patients are:
- To correct an ocular deviation in primary position associated with an anomalous head posture:
- Unilateral or bilateral medial rectus recession
- Unilateral or bilateral lateral rectus recession
- To correct an ocular deviation and improve abduction and binocular single vision field:
- Vertical rectus transposition procedures
- Recess-resect procedures in the Duane eye
- To correct globe retraction and upshoot and downshoot of mechanical origin:
- Combined horizontal rectus recessions
- Faden procedure on the lateral rectus
- Y splitting of the lateral rectus
- To correct vertical deviation
- Vertical muscle recession
Combination of these procedures must be used according to the particular clinical characteristics of each case.
Medial Rectus Recessions
Unilateral single medial rectus muscle recession improves or eliminates face turn, corrects esotropia in primary position of gaze, and maintains good stereoacuity in most patients with moderate compensatory head posture. This has been considered the procedure of choice in most DRS cases with esotropia (Figure 17).46 Unilateral medial rectus recession can correct up to 20 PD of deviation in primary position.47,48

Figure 17. Preoperative (top row) and postoperative (bottom row) pictures after left medial rectus recession 6 mm. Improvement of head posture and orthophoria in primary gaze, slight improvement of abduction of the left eye
Recessions larger than 5 mm of the medial rectus of the affected eye may result in significant limitation of adduction, producing diplopia in the field of gaze where the patient was diplopia free before the surgery. This is especially true in cases where adduction saccadic velocities are very slow, and some limitation of adduction is present. It is better to leave the patient with a small residual anomalous head position and not sacrifice the entire adduction capacity of the affected eye.
Larger recessions can result in markedly decreased adduction and lead to a consecutive exotropia, synergistic divergence, or limited ocular rotations, which can be very difficult to manage. This is usually produced by anomalous contraction of the lateral rectus that does not encounter the same resistance as before the surgery from the now-weakened medial rectus.
There are 3 situations where adding a recession on the contralateral medial rectus can be useful:
- In cases of large-angle esotropia in primary position (more than 20 PD) (Figure 18)

Figure 18. Patient who underwent right medial rectus recession of 7 mm and left medial rectus recession of 5 mm for an esotropic-Duane of 25 diopters in primary gaze. Top row: Preoperative pictures. Bottom row: First day postoperative pictures, patient is orthotropic, with less retraction in adduction but also some limitation in adduction.
- Cases with esotropia and significant globe retraction where a lateral rectus recession is added to the medial rectus recession to correct the globe retraction. This will diminish the effect of the weakening of the ipsilateral medial rectus recession and a contralateral medial rectus recession will help correct the esotropia in primary position.
- To prevent the recurrence of contracture in the medial rectus of the affected eye by creating a fixation duress on the non-affected eye and driving the affected eye outward (due to Hering’s law), thus diminishing the likelihood of any re-contraction of the affected eye’s recessed medial rectus.49
Lateral rectus recessions
Unilateral single lateral rectus muscle recession improves or eliminates face turn, corrects exotropia up to 20 PD in primary position of gaze, and will help alleviate a severe globe retraction. If the exotropia is over 25 PD, adding a recession of the contralateral lateral rectus might be considered.50 If an asymmetric bilateral recession is chosen, the recession of the contralateral lateral rectus should be larger.51(Figure 19)
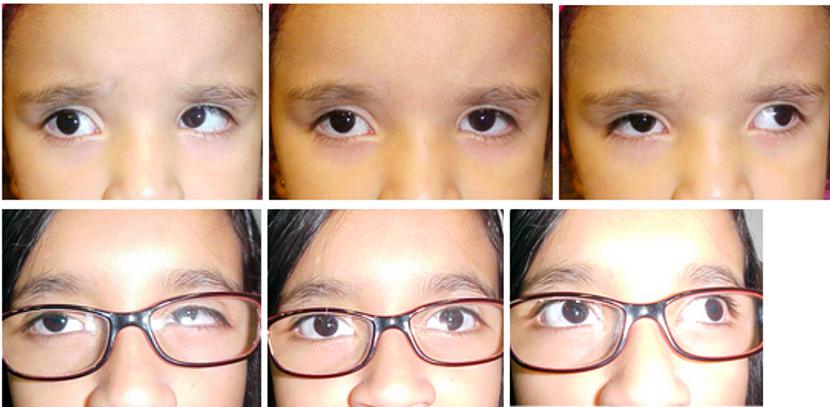
Figure 19. Patient with exotropic-Duane before and after right lateral rectus recession of 7 mm.
However, recession of the contralateral rectus muscle should be avoided in cases with large globe retraction that may signify significant anomalous innervation of the affected lateral rectus. In these cases, recessing the lateral rectus of the unaffected eye will elicit more innervation to the recessed lateral rectus in order to maintain fixation. This augmented innervation will also affect the medial rectus of the affected eye through Hering’s law. If the lateral rectus of the affected eye is receiving a significant amount of abnormal innervation from the third nerve, it will also contract, thereby worsening the exotropia.
Contrary to the medial rectus recessions, the lateral rectus recessions can be larger (7 to 10 mm). It is very difficult to have an overcorrection. Some authors have even attached the lateral rectus to the periosteum or to the lateral canthal tendon without experiencing postoperative overcorrections.52,53
Transposition procedures
Transpositions of the vertical muscles to the lateral rectus in DRS cases have been advocated by different authors for a number of years.15,54 The goal of this surgery is to generate active abduction vector forces in order to enlarge the area of single binocular vision.
Adding a posterior lateral fixation suture to the transposed vertical muscles (Foster suture), can result in fewer undercorrections and surgically induced vertical deviations.55
Superior rectus transposition to the lateral rectus was first described by Johnston and Crouch, who treated 32 DRS patients, with no vertical deviation noted postoperatively (Figure 20).56 Superior rectus transposition will correct esotropias of 12-14 PD in primary position. When the deviation is larger, a unilateral or bilateral medial rectus recession can be added.57,58

Figure 20. Patient who underwent left medial rectus recession of 4 mm and transposition of the left. Superior rectus to the lateral rectus with Foster suture augmentation. Notice improvement of face turn and left abduction.
Inferior rectus transposition has also been advocated in the treatment of patients with esotropic DRS.59 Inferior rectus transposition seems to be more useful in cases with V pattern or more limitation of abduction in depression.
Transposition procedures should only be very carefully considered in DRS patients. They may create restriction in adduction, mainly in cases where severe innervational anomalies are present. Undercorrections, overcorrections, induced vertical deviations, and worsening of co-contraction with anomalous vertical movements have been reported in up to 30% of the patients who underwent horizontal transposition of the vertical rectus muscles to the lateral rectus muscle.60
These procedures should be avoided in patients who have significant globe retraction and in patients who show any evidence of anomalous innervation on the vertical rectus muscles.
Recess – resect procedures
Resecting the lateral rectus of the affected eye of DRS patients is generally not advocated, because there is a concern that the globe retraction might worsen as a result. However, this procedure has been performed successfully in selected patients.60 Patients with esotropic-Duane with an angle of more than 25 diopters in primary position, patients with mild globe retraction (palpebral fissure diminishes less than one-third in adduction), and patients with very limited abduction (-3.5), clinically normal adduction and an absence of anomalous vertical movement might all receive some degree of improvement from this approach. (Figure 21) Resection of the lateral rectus should never be more than 3.5 mm, and the combined recession of the medial rectus should be moderate (never more than 5 mm) in order to avoid overcorrections.

Figure 21. Patient underwent left medial rectus recession of 4.5 mm and left lateral rectus resection of 3.5 mm. Top row: Preoperative pictures. Bottom row: postoperative pictures. Notice the improvement of face turn and abduction of the left eye.
Combined horizontal rectus recessions
Combining medial and lateral rectus recessions of the affected eye of DRS patients has proven to be a very useful procedure to diminish globe retraction. The amount of recession required must be large, and in order to maintain balance in primary position, the lateral rectus is recessed 1 mm more than the medial rectus. In cases of esotropia in primary position, the medial rectus must be recessed more, and in cases of exotropia the lateral rectus has to be recessed much more, in order to correct the strabismus in addition to the globe retraction.61
Faden procedures
Faden procedures (posterior fixation sutures) have also been advocated for treatment of DRS. This technique can be used in 2 situations:
- On the lateral rectus of the affected eye, in order to avoid the side-slipping of the muscle in cases of significant upshoot or downshoot of mechanical origin
- On the contralateral medial rectus of a Duane eye with significant limitation of abduction in order to limit the excursion of the operative eye when looking towards the affected eye to match the duction deficits
Y splitting of the lateral rectus
This procedure was described by Jampolsky62 and it is very useful in treating mechanical upshoots and downshoots. The lateral rectus is split horizontally in half from the insertion as far back as possible, spreading the muscle halves 20 mm apart. Each half of the muscle should be recessed a couple of millimeters (or even more) if an exotropia in primary position is present. (Figure 22)

Figure 22. Y split of the lateral rectus.
Vertical rectus muscle recessions
Recession of the superior rectus muscle is required in cases where a secondary contracture of the muscle results from severe and persistent upshoot of innervational origin. In such cases, a hypertropia exists in all superior fields of gaze; this also includes all the other characteristics of a superior rectus overaction/contracture syndrome.63 Superior rectus recessions in these cases must be large; this also ameliorates the globe retraction, which is present in some cases (Figure 23).

Figure 23. Before and after right superior rectus recession of 9 mm and right lateral rectus recession of 6 mm with Y split.
Summary
Duane retraction syndrome is a complex condition that can present in a great variety of clinical manifestations. Comprehensive ocular and systemic evaluation are mandatory in order to better understand the clinical presentation. Although no currently available procedure can normalize ocular motility in these patients, many of the most noticeable signs and symptoms can be satisfactorily reduced with a personalized surgical approach for each case.
References
- Heuck G. Uber angeborenene vererbten Beweglichkeitsdefect der Augen. Klin Monatsbl Augenkeilkd. 17:253 1879.
- Stilling G. Untersuchungen über die Entstehung der Kurzsichtigkeit. Wiesbaden, Germany: JF Bergaman, 1887;13.
- Sinclair WW. Abnormal associated movement of the eyelids. Ophthalmol Rev. 14:307-319,1895.
- Mac Lebose NM. Paralysis of left external rectus, movement inwards of the affected eye associated with contracture of the orbicularis palpebrarum on the same side and marked retraction of the left globe. Trans Ophthalmol Soc UK. 16:299, 1895.
- Türk S. Bemerkungen zu einem Falle von retraction des Auges. Zbl Prakt Augenheilk. 1899;23:14.
- Duane A. Congenital Deficiency of abduction, associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. Arch Ophthalmol. 1905; 34:133.
- Ahluwalia BK, Gupta NC, Goel SR, Kuhrana AK. Study of Duane’s retraction syndrome. Acta Ophthalmologica. 66:728-730,1988.
- Prieto Diaz – Souza Dias. In Ediciones cientificas Argentinas. Quinta Edicion. Buenos Aires, 2005. P.427
- Mehel E, Quere MA, Lavenant F, et al: Aspects epidemiologiques et cliniques du syndrome de Stilling-Turk-Duane. J Fr Ophthalmol. 1966;19:533.
- Mohan K, Sharma A, Pandav SS. Differences in epidemiological and clinical characteristics between various types of Duane retraction syndrome in 331 patients. J AAPOS. 2008;12(6):576-580.
- Khan AO, Oystreck D. Clinical characteristics of bilateral Duane syndrome. J AAPOS. 2006;10:198-201.
- DeRespinis PA, Caputo AR, Wagner RS, Guo S. Duane’s retraction syndrome. Surv Ophthalmol. 1993;38:257-288.
- Parsa CF, Robert MP. Thromboembolism and congenital malformations: from Duane syndrome to thalidomide embryopathy. JAMA Ophthalmo 2013;131(4):439-447.
- Pineles SL, Velez FG. Accessory fibrotic lateral rectus muscles in exotropic Duane syndrome with severe retraction and upshoot. 2015;19(6):549-550.
- Gobin MH: Surgical management of Duane’s syndrome. Br J Ophthalmol 58:301-306,1974
- Demer JL, Clark RA, Key-Hwan L, Engle EC: Magnetic resonance imaging evidence for widespread orbital dysinnervation in dDominant Duane’s retraction syndrome linked to the DURS2 locus. Invest Ophthalmol Vis Sci. 2007;48:194-202.
- Duke-Elder WS: Normal and abnormal development. Congenital deformities, in System of Ophthalmology, Vol 3 pt. 20 St Louis, CV Mosby, 1964:991-995.
- Francois J. Heredity in Ophthalmology. St Louis, CV Mosby, 1961:247-251.
- Appukuttan B, Gillanders E, Juo SH, et al. Localization of a gene for Duane retraction syndrome to chromosome 2q31. Am J Hum Genet. 1999;65(6):1639-1646.
- Miyake N, Chilton J, Psatha M et al. Human CHN1 mutations hyperactivate alpha2-chimaerin and cause Duane’s retraction syndrome. Science. 2008;321(5890):839-843.
- Pfaffenbach DD, Cross HE, Kearns TP. Congenital anomalies in Duane’s retraction syndrome. Arch Ophthalmol. 1972;88(6):635-639.
- Vincent C, Kalatzis V, Compain S, et al. A proposed new contiguous gene syndrome on 8q consists of branchio-oto-renal (BOR) syndrome, Duane syndrome a dominant form of hydrocephalus and trapeze aplasia: Implications for the mapping of the BOR gene. Hum Mol Genet. 3:1859,1994.
- Kirkham TH: Inheritance in Duane’s syndrome. Br J Ophthalmol 54:323-329, 1970.
- Al-Baradie R, Yamada K, St Hilaire C, et al. Duane radial ray syndrome (Okihiro syndrome) maps to 20q13 and results from mutations in SALL4, a new member of the SAL family. Am J Hum Genet. 2002;71(5): 1195-1199.
- Kohlhase J, Heinrich M, Schubert L, et al. Okihiro syndrome is caused by SALL4 mutations. Hum Mol Genet. 2002;11(23):2979-2987.
- Assaf AA. Congenital innervation dysgenesis syndrome (CID)/congenital cranial dysinnervation disorders (CCDDs). Eye (Lond). 2011;25(10):1251-1261.
- Matteuci, P. I difetti congenti di abduzione con particolare riguardo allá pathogenesi. Rassegna Ital Ottalmologia. 15, 345–380.
- Parsa CF, Grant PE, Dillon WP Jr, du Lac S, Hoyt WF. Absence of the abducens nerve in Duane syndrome verified by magnetic resonance imaging. Am J Ophthalmol. 1998;125(3):399-401.
- Hoyt WF, Nachtigaller H. Anomalies of ocular motor nerves. Am J Ophthalmol. 60:443-448, 1965.
- Breinin GM. In discussion of: de Gindersen T, Zeavin B. Observations on the retraction syndrome of Duane. Arch Ophthalmol. 55:5760, 1956.
- Sato S. Electromyographic study on retraction syndrome. Jpn J Ophthalmol. 4:57-66,1960.
- Huber A: Electrophysiology of the retraction syndromes. Br J Ophthalmol 58:293-300, 1974.
- Huber A. Duane’s retraction syndrome. Considerations on pathogenesis and aetiology of the different forms of Duane’s retraction syndrome. In: Strabismus London: Henry Kimptom, 1970;36.
- Nemet P, Ron S. Ocular saccades in Duane’s syndrome. Br J Ophthalmol. 1978;62:528.
- Pressman SH, Scott WE. Surgical treatment of Duane’s syndrome. 1986; 93:29-38.
- Jampolsky A. Duane Syndrome in Rosenbaum A, Santiago AP: Clinical Strabismus Management. WB Saunders Company. Philadelphia, 1999. p.325-342.
- Papst W, Esslen E. Symptomatology and therapy in ocular motility disturbances. Am J Ophthalmol. 1964; 58:275-291.
- Scott AB, Wong GY. Duane’s syndrome: an electromyographic study. Arch Ophthalmol. 1972;87:140.
- Isenberg S, Urist MJ. Clinical observations in 101 consecutive patients with Duane’s retraction syndrome. Am J Ophthalmol. 1977; 84:419-425.
- Chung M, Stout JT, Borchert MS. Clinical diversity of hereditary Duane’s retraction syndrome. 2000;107(3):500-503.
- Sloper JS, Collins AD. Effects of Duane’s retraction syndrome on sensory visual development. 1999; 7:25-35.
- Jampolsky A. A simplified approach to strabismus diagnosis. In Burian HM (ed): Symposium on Strabismus. Transactions of the New Orleans Academy of Ophthalmology. St Louis CV Mosby, 1974:34.
- Romero Apis D. In Estrabismo: Aspectos Clínicos y Tratamiento. Editorial DALA. Mexico DF 2010:236.
- Molinari A. Krokodilstränen und Retraktionssyndrom. Klin Monatsbl Augenheilkd 1996;208:56-57.
- Papst W. Thalidomid und kongenitale Anomalien der Augen. Dtsch Ophtalmol Ges 65:209-215, 1963.
- Natan K, Traboulsi E. Unilateral rectus muscle recession in the treatment of Duane syndrome. J AAPOS. 2012;16:145-149.
- Jampolsky A. Strategies in strabismus surgery. In: Pediatric ophthalmology and strabismus. Transactions of the New Orleans Academy of Ophthalmology. New Your, Raven 1986: 366-367.
- Kraft SP. Surgery for Duane’s syndrome. Am Orthoptic J. 1993;43:18-26.
- Kaban TS, Smith K, Day C, et al. Single medial rectus recession in unilateral Duane Syndrome type I. Am Orthoptic J. 1995;45:108-114.
- Kraft SP. A surgical approach for Duane syndrome. J Pediatr Ophthalmol Strabismus. 1988;25:119-130.
- Kekunnaya R, Negalur M. Duane retraction syndrome: causes, effects and management strategies. Clin Ophthalmol. 2017;11:1917-1930.
- Sukhija J, Singh M, Singh U. Profound weakening of the lateral rectus muscle with attachement to lateral canthal tendon for treatment of exotropic Duane syndrome. J AAPOS 2012;16:298-300.
- Sharma P, Tomer R, Menon V, Saxema R, Sharma A. Evaluation of periosteal fixation of lateral recuts and partial VRT for cases of exotropic Duane retraction syndrome. Indian J Ophthalmol. 2014;62(2):204-208.
- Yazdian Z, Rajabi MT, Yazdian MA, Rajabi MB, Akbari MR. Vertical rectus muscle transposition for correcting abduction deficiency in Duane’s syndrome type I and sixth nerve palsy. J Pediatr Ophthalmol Strabismus. 2010;47:96-100.
- Velez FG, Foster S, Rosenbaum AL. Vertical Rectus Muscle Augmented Transposition in Duane Syndrome. J AAPOS. 2001;5:105-113.
- Johnston SC, Crouch Jr ER, Crouch ER. An innovative approach to transposition surgery is effective in treatment of Duane’s syndrome with esotropia. Invest Ophthalmol Vis Sci. 2006;47:2475.
- Kekunnaya R, Kraft SP, Rao VB, Velez FG, Sachdeva V, Hunter DG. Surgical management of Strabismus in Duane retraction syndrome. J AAPOS. 2015;19(1):63:69.
- Mehendale RA, Dagi LR, Wu C, Ledoux D, Johnston S, Hunter DG. Superior rectus transposition and medial rectus recession for Duane syndrome and sixth nerve palsy. Arch Ophthalmol. 2012;130(2):195-201.
- Sener EC Yilmaz PT, Fatihoglu ÖU. Superior or inferior rectus transposition in esotropic Duane syndrome: a longitudinal analysis. J AAPOS. 2019;23:21.el-7.
- Morad Y, Kraft SP, Mims JL 3rd. Unilateral recession and resection in Duane syndrome. J AAPOS. 2001;5:158-162.
- Sprunger DT. Recession of both horizontal rectus muscles in Duane syndrome with globe retraction in primary position. J AAPOS. 1997;1:31-33.
- Jampolsky A. Discussion of Eisenbaum AM, Parks MM: A study of various surgical approaches to the leash effect in Duane’s syndrome. Presented at the joint session of the American Association for Pediatric Ophthalmology and Strabismus and the American Academy of Ophthalmology. Chicago, 1980.
- Arora P, Ganesh S, Shanker V. Duane’s retraction syndrome with sever upshoot and ipsilateral superior rectus contracture: A rare presentation. J Clin Ophthalmol Res. 2014;2(2):108-110.