Introduction
Isolated extraocular muscle injuries without globe involvement are not uncommon. There is not a great deal written about strabismus caused by direct trauma to the eye muscles. The topic receives scarce coverage in textbooks and is not mentioned in many publications.1,2,3
The purpose of this chapter is to review the existing literature on this subject and to present my own experience in the management of patients presenting with this unique form of strabismus.
Traumatic strabismus may result because of closed or open head and/or orbital trauma. A number of structures responsible for eye movements can be affected in the event of trauma and result in strabismus:
- Supranuclear structures
- Oculomotor nuclei or nerves
- Extraocular muscles
Loss of vision after ocular injury might also lead to secondary sensory strabismus.
Trauma to the extraocular muscles will often result directly in specific ocular motility disorders that can pose a real challenge for treatment. Recent advances in orbital imaging, surgical techniques, and new information on different trauma mechanisms have improved the outcome of these complex cases.
Types of extraocular muscle trauma
There are 3 basic mechanisms that can affect the extraocular muscles in the event of trauma and produce strabismus:
- Muscle involvement in orbital wall fractures
- Muscle contusion
- Traumatic disinsertion or laceration of the extraocular muscles
Each of these entities has defined clinical characteristics which require different management.
Muscle involvement in orbital wall fractures
Strabismus due to muscle involvement in orbital wall fractures can result from either of 2 different mechanisms:
- Muscle incarceration in an orbital wall fracture; or
- Flap tear of a rectus muscle as described by Ludwig in 2001.4,5
The most common form of strabismus related to orbital injury results from fractures of the bony orbit.6
Orbital wall fractures caused by a frontal impact of objects to the globe or the orbit will usually affect the inferior wall or the medial wall, which are the thinnest anatomically. (Figure 1)

Figure 1. The medial and inferior orbital wall are the thinnest and most commonly fractured
The muscles more commonly affected are the inferior rectus, the inferior oblique, the medial rectus, and the superior oblique. Superior rectus and lateral rectus are very infrequently injured by orbital wall fractures.
Entrapment of more than 1 muscle is also possible when the medial wall and the orbital floor are fractured, thereby affecting elevation and abduction in the same eye. (Figure 2)


Figure 2. Patient with fracture of the medial and inferior wall with limitation of elevation and abduction. Arrows indicate both fracture sites.
These fractures occur due to increased orbital pressure produced by the impact, resulting in direct compression and fracture of the bony wall. The force transmitted posteriorly to the orbital rim transiently buckles and then fractures the thin orbital wall. In adults, this produces a comminuted fracture with multiple fragments, often termed “open door fracture” or “blow out fracture,” but in children the bone is more elastic and usually produces a type of fracture called “trapdoor,” because the broken bone bends, entraps the orbital tissue, and then closes.7 It is a linear, minimally displaced fracture that opens transiently at the time of injury and then springs back into place. One important complication of this injury is the possibility of infarction of the entrapped muscle. Often the orbital surgeons may want to wait up to 7 to 10 days for the swelling to diminish before repairing the blowout fracture in adults, but entrapped muscle, particularly in pediatric population, requires early intervention before the muscle is severely damaged due to ischemia.
Compromise of the muscle in the fracture site is variable: the bigger the fracture, the less likely the muscle is going to be entrapped. Patients with large fractures (including blow out fractures) often present with periorbital ecchymosis and manifest enophthalmos due to orbital tissue prolapse into the sinus, but with less motility disturbance. Conversely, patients with trapdoor fractures often will incarcerate the muscle (or the soft tissue surrounding the muscle), thus producing significant restriction of eye movement.
A special type of trapdoor fracture, occurring nearly exclusively in children or young adults, is termed “White-eyed floor fracture.”8 These fractures are usually related to sports or to assault. Contrary to blow out fracture, these patients present with minimal bruising; the eye appears white, without or very minimal subconjunctival hemorrhages. Muscle or perimuscular tissue is often entrapped resulting in severe restriction to ocular motility. However, the pathognomonic characteristic of this fracture type is triggering of the oculocardiac reflex consisting of the following triad of symptoms: nausea/vomiting, syncope and bradycardia. These vagotonic symptoms result from the communication of the ophthalmic branch of the trigeminal nerve and the visceral motor nucleus of the vagal nerve via the reticular formation. The presence of nausea and vomiting has been reported to have a positive predictive value of 75% for a trapdoor fracture.7
Flap tear of a rectus muscle can be produced by the sudden downward force exerted by the orbital tissue displaced to the fracture site. This traction of the connective tissue produces the tearing of the outer orbital layer away from the inner global layer of the muscle. This type of lesion usually produces limitation towards the affected muscle, contrary to what usually occurs when the inferior rectus muscle is entrapped in a floor fracture. (Figure 3)

Figure 3. The outer orbital layer separates from the inner global layer and becomes incarcerated at the fracture site.
The muscle flap tear can also be caused by a lacerating force directed to the globe.9
Both types of injuries, the muscle entrapment and the flap tear, produce a similar clinical scenario with the presence of restrictive strabismus with a positive forced duction test and usually a positive force generation test since the entrapped muscle generally does not lose its contractile ability. If there is substantial prolapse of orbital contents through the orbital fracture, enophthalmos may be present. Infraorbital anesthesia can also be observed due to trauma to the infraorbital nerve.
The patient will often suffer diplopia minimized by an anomalous head posture. (Figure 4)

Figure 4A

Figure 4B
Figure 4. (A) Patient with a trapdoor fracture in the upper medial wall with entrapment of the right superior oblique, demonstrating a Brown Syndrome and an anomalous head posture to avoid diplopia. (B) Patient with a trapdoor fracture in the upper medial wall with entrapment of the right superior oblique, demonstrating a Brown Syndrome and an anomalous head posture to avoid diplopia.
Typically, orbital floor fractures present with a restrictive hypotropia with limitation of elevation on the affected side. Some patients appear with a restrictive hypertropia with limitation of depression on the affected side and this might be due either to the entrapment of tissue in a posterior floor fracture or to the adhesions of a flap tear.10
Muscle contusion
Contusion of an extraocular muscle is produced by the impact of an object on the surface of the muscle without perforating any structure in the eye or its surrounding tissues. After impact, edema or a hematoma is formed in the muscle´s belly limiting the muscle function.11,12 (Figure 5)

Figure 5. Direct contusion of the muscle produces a hematoma.
This type of trauma produces an incomitant strabismus with a forced duction test that might be positive due to the hematoma. The muscle does not contract very well; therefore, the force generation test might be diminished. There is no wound, although ecchymosis of the inferior lid might be observed. The most important feature is that the strabismus improves spontaneously. The most susceptible muscle to suffer a contusion is the inferior rectus due to its exposure during Bell´s phenomenon during the traumatic episode. (Figure 6)
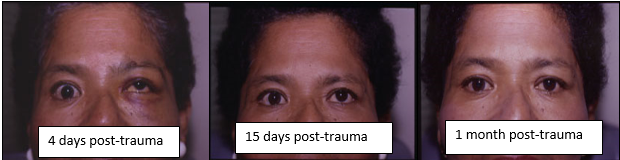
Figure 6. This patient suffered non-perforating trauma with contusion to the left inferior rectus. Complete resolution of her strabismus after one month can be appreciated.
Traumatic disinsertion or laceration of the extraocular muscles
Traumatic disinsertion is caused by the impact of a blunt object that perforates conjunctiva and disinserts the muscle cut flush with the sclera. Attachment of the muscle capsule to the check ligaments and intermuscular membrane prevents the muscle from retracting deeply into the orbit so the muscle is usually found reattached behind the normal insertion site. For this reason, muscle function might be preserved.12 (Figure 7)

Figure 7. Traumatic disinsertion of the eye muscle
Laceration of the muscle is usually caused by the impact of a sharper object that perforates conjunctiva and ruptures the muscle. (Figure 8) These cases, demonstrate larger limitation of the function of the compromised muscle than in cases involving muscle disinsertion. The angle of strabismus might be larger and a fibrotic reaction around the affected tissue can be significant which makes surgical repair more difficult.

Figure 8. Traumatic laceration of the eye muscle.
A “snapped” or torn muscle is one in which the insertion to the globe remains intact, but the muscle belly has been completely ruptured across its width at some point posterior to the muscle insertion. (Figure 9) Muscles that are transected posteriorly are the most difficult to retrieve.

Figure 9. A “snapped” rectus muscle.
Clinical features of these type of cases include incomitant strabismus; the forced duction test is usually negative but might become positive with time due to contracture of the antagonist muscle or if significant reactive fibrosis is present. Force generation test is usually negative or diminished. The patient presents with widening of the palpebral fissure when looking towards the affected muscle. Diplopia and anomalous head posture are also very common if the visual acuity is not affected. All rectus muscles can be injured in this manner but the most frequently injured are the inferior and medial recti. This is due to the fact that these two muscles are closest to the limbus and exposed to trauma during Bell´s phenomenon.13
Evaluation of a Patient with Suspected Extraocular Muscle Injury
Evaluating a patient with suspected extraocular muscle injury can be challenging. In some cases, the severity of the non-ocular or global injuries might be so great as to delay the diagnosis of the ocular motility deficit.
Before evaluating the eye motility status and the condition of the eye muscles, it is crucial to determine that no other globe structures are damaged. Therefore, a thorough eye exam, including a careful examination of the fundus should be performed.
Useful information about the motility status and the eye muscle condition in a patient with suspected extraocular muscle lesions can be obtained with the following:
Evaluation of ocular motility
Ocular ductions and versions should be carefully evaluated to determine the presence of restrictions or motility deficits. When performing the cover test in these patients, it is very important to occlude each eye in turn, long enough to allow the patient to pick up fixation, many of these patients might have decreased visual acuity or visual field defects that make fixation with each eye more difficult. It is easy to underestimate traumatic strabismus because the patient may not want to move their eyes due to pain and not only due to the limitations in its rotations.14
Evaluation of saccadic velocities will also help evaluate the potential contractile power of the muscle. Restricted eyes will be able to make fast saccades up to the limit of their restriction. Paretic eyes will move with subnormal velocity (“floating saccades”) and increased latency.
Forced duction test will provide valuable information about mechanical limitations to full ocular rotation of the globe. This is performed by placing local anesthesia in a cooperative patient and passively moving his eye to the opposite direction of the suspected injured muscle with forceps or a cotton-tip applicator. (Video 1)
Video 1. This patient had an exotropia secondary to an incarceration of the right medial rectus in a medial orbital wall fracture. The video shows that the forced generation test result was positive and the forced traction test was also positive. The eye could be adducted with difficulty due to the medial rectus entrapment in the medial wall fracture.
The force generation test will inform the examiner about the active forces available to move the globe. Local anesthesia is placed on the eye to be tested. The patient is instructed to look in the direction opposite from the field of action of the muscle to be tested. The eye is grasped with forceps at the limbus and the patient is then asked to move the eye towards the muscle to be tested. The amount of tug felt by the examiner through the forceps or the cotton-tip applicator, indicates the contracting power of the affected muscle. (Video 1)
Orbital imaging
Crucial information for the diagnosis and management of a patient with suspected extraocular muscle injury, can be obtained through CT scan or an MRI. The gold standard imaging workup for suspected orbital wall fractures, consists of high resolution CT scans (facial or orbital thin slices of 1-2 mm), since it provides the best image of the relation between the muscle and the fracture site. Even though in children this exam has been found to significantly underestimate extraocular muscle and soft tissue entrapment as compared with the adults, it is still the best method to evaluate these cases. The MRI provides a better image of the structural situation of the muscle and soft tissues. Multi-positional MRI is even better and will provide information about the contractility power that the muscle has. MRI of the orbits with fat suppression provides further details as it focuses on the muscles. Although now days the imaging is many times performed automatically with fat suppression it may still be beneficial to remind the radiologist or the technicians in some institutions.
Coronal cuts will usually give the most useful information when studying the relationship between the muscle and the fracture site in cases of floor fractures, but sagittal and axial cuts can also provide useful information about the structural situation of the rectus muscles.
Dynamic magnetic resonance imaging with surface coil will provide the best image of a traumatized orbit that includes extraocular muscle damage.
Establishing a diagnosis of extraocular muscle trauma
When faced with a case where an extraocular muscle might be affected due to trauma, it is very important to determine what is the condition of the compromised muscle in order to plan for the best strategy in managing the case.
The preoperative evaluation should include an assessment of the degree of restriction, muscle function and the condition of the surrounding tissues.15
A careful history of the events of trauma, clinical evaluation and orbital imaging usually provides enough information to get an accurate diagnosis of the problem.
If the patient suffered a non-perforating trauma of the orbit and has an incomitant strabismus with a positive forced duction test, orbital images will be crucial to rule out if an orbital wall fracture is present with entrapment of an extraocular muscle. If no orbital fracture can be demonstrated, an MRI and the evolution of the case will help determine if a muscle hematoma or a flap tear of the muscle is present.
After a penetrating trauma of the orbit, dynamic magnetic resonance, will provide the best information about the condition of the affected eye muscle and its contractile capabilities. If the patient has an incomitant deviation but still has good eye movement towards the affected side, the muscle is probably detached and not lacerated. In these cases, the check ligaments and intermuscular membrane are usually not extensively damaged and hold the detached extraocular muscle in close to normal position and the muscle will reattach not far back from its normal insertion.1,2 (Figure 10)

Figure 10. This patient suffered a perforating orbital trauma with a tree branch when falling from a horse. The left levator palpebrae was lacerated and the left superior rectus was traumatically disinserted. Notice the left hypotropia in primary position, but still good elevation of that eye. During surgical repair, the superior rectus was found inserted five millimeters back from its normal insertion.
If the muscle is lacerated, ocular motility will be significantly affected and fibrosis around the lacerated muscle can occur, limiting all eye movements. (Figure 11)

Figure 11. This patient suffered a stab incision in the upper orbit (yellow arrow pointing the scar) with laceration of the levator, superior rectus and optic nerve. Notice the limitation of all eye movements of the left eye, due to fibrosis on the superior rectus (fibrosis seen on the CT scan pointed with the red arrow).
Management of strabismus secondary to eye muscle trauma
Once the diagnosis is established, proper action should be taken in a timely manner to get the best postoperative results.
Treating traumatic strabismus is challenging, because both the muscle and the surrounding tissues are involved.3
If contusion of a muscle is suspected, observation is advised. Anti-inflammatory agents might accelerate recovery time. These cases usually resolve with complete restoration of the extraocular movements.
If a flap tear is present in the event of a floor fracture, this flap which is usually adherent to the surrounding orbital tissues, should be dissected and sutured back to the muscle, sometimes advancing it to the muscles’ insertion with a non – absorbable suture and placing a free tenon´s graft over it. Ocular movement exercises in the early postoperative period are useful to avoid new adhesion of this muscle flap to the surrounding tissues.4
Entrapment of an extraocular muscle in an orbital wall fracture usually needs surgical repair. Surgery should not be indicated based on orbital imaging alone but on the basis of both, radiological and clinical signs of entrapment. The presence of vasovagal symptoms can be considered an indication for immediate surgery to release the entrapped muscle and repair the orbital wall fracture.16,17,18 If no vasovagal symptoms are present, surgery for releasing an apparently incarcerated muscle can be deferred for one week until edema resolves and makes surgery easier. In some cases, the swelling of the surrounding tissues produces the ocular motility restriction, waiting one week gives the opportunity for improvement of this limitation and indicates that observation is advised instead of proceeding with a surgical intervention.
Entrapment of an inferior rectus or inferior oblique in a floor fracture are less likely to resolve spontaneously than entrapment of a medial rectus or superior oblique (Figure 12). The edema and ecchymosis around the trochlear complex likely prevents the movement of the superior oblique as well, causing the traumatic Brown’s syndrome. As the inflammation and edema subsides, the superior oblique starts to slide through the complex and the Brown’s syndrome resolves along with it.

Figure 12. Patient who suffered severe cranioencephalic trauma with entrapment of the right superior oblique in an upper medial trapdoor wall fracture (yellow arrow). Notice spontaneous resolution of elevation of the right eye 12 months after trauma.
If there is no obvious muscle incarceration in an orbital wall fracture, or the fracture is not big enough to produce significant orbital prolapse, observation of the patient is the treatment of choice.
Repairing an orbital wall fracture is not without complications. Among them:
Early surgical complications:
- Orbital compartment syndrome
- Implant impingement of rectus worsening the diplopia
- Implant impingement of optic nerve with loss of vision
- Permanent mydriasis
- Infraorbital nerve hypesthesia
Delayed surgical complications:
- Lower eyelid retraction
- Implant extrusion
- Dacryocystitis
- Orbital cellulitis
- Persistent diplopia
- Scar tissue formation around the implants effecting the eye movements
In cases where traumatic disinsertion of the muscle is suspected, the muscle should be localized and reattached to the original insertion without further delay. If the muscle seems weak, a small resection can be added.
In longstanding cases, contracture of the antagonist muscle is often found. These cases require weakening of the antagonist muscle. (Figure 13)

Figure 13. Patient suffered a penetrating left orbital trauma with a metal rod 12 years earlier. The left inferior rectus was found 12 mm back from limbus and was reinserted 5 mm from limbus. The contracted left superior rectus was recessed 4 mm from limbus to get a good alignment in primary position.
Of all traumatic extraocular muscle lesions, muscle lacerations are probably the most challenging to resolve.
An eye muscle can be partially lacerated or completely ruptured across its width. Partially lacerated muscles will be suspected in cases were the MRI demonstrates continuity of the path of the muscle and the patient has some ocular movement towards the affected side (Figure 14). These cases are easily repaired by attaching both ends and the functional result is usually good.

Figure 14. Patient suffered a perforating trauma in the inferior right orbit with a wire. Notice that some depression of the eye can still be seen. The MRI demonstrates a disruption in the path of the inferior rectus and during the surgical procedure some fibers are seen still uniting both muscle stumps. (Courtesy Dr. Cristina Ugrin)
If an extraocular muscle has been completely lacerated, retrieval of both ends of the muscle should be always attempted, either by a direct conjunctival approach if the rupture is located anteriorly, or by an anterior medial orbitotomy if the rupture is located deep in the orbit.19) Other procedures such as muscle transposition or tethering procedures to the orbital walls3 should be considered only if the damaged proximal stump cannot be found.
Extraocular muscle transpositions (EOM) might seem easier to perform than a recovery surgery of the lost proximal muscle stump, but the results are inferior to recovering and reinserting the damaged muscle. EOM transpositions at best can establish fusion within a relatively small area resulting in a limited area of single binocular vision.1 Given the availability of an anterior orbital approach, it is reasonable to attempt the muscle stump recovery since it will give the possibility of a larger area of single binocular vision and decrease the risk of anterior segment ischemia.20
Some authors prefer to defer the recovery of a transected muscle 5 to 6 weeks, to allow time for a thorough ocular motility evaluation, and adequate imaging studies.1 Additional time before exploration allows for resolution of all hemorrhages and edema and for restoration of anatomic planes and normal tissue appearance. Other authors do recommend not waiting much longer than 7 to 10 days to avoid contracture of the antagonist muscles.21
Weakening of the antagonist muscle might be needed, not only due to its contracture, but also when the traumatized muscle was severely damaged and muscle tissue was lost.
The highest magnification is needed in these cases; therefore, they should be done under an operating microscope with a very good assistance and special instruments like angled retractors or malleable valves to assure good exposure of the deep orbit.22 An attentive anesthesiologist that can pick up subtle changes in the cardiac frequency is also very useful.
The proximal stump of the medial rectus is the most difficult to locate due to the lack of attachments of this muscle in comparison with the other recti muscles. The direction of the exploration should be parallel to the medial wall of the orbit and not along the curve of the globe.23,24
Aggressive orbital dissection should be avoided, because this may result in laceration of the Tenon capsule with orbital fat prolapse and the possibility of development of a fat adherence syndrome.25,26
Sometimes, the proximal stump might be attached to the globe, so if it is not found parallel to the medial wall it is worth trying to locate it posteriorly attached to the globe. (Figure 15)

Figure 15. A suture is passed through the proximal stump (white arrow) of a lacerated left inferior rectus from a patient that suffered a penetrating orbital injury with a metal stick that lacerated the inferior rectus and optic nerve. It was located 24 mm back from limbus.
When found, both stump ends should be reattached with non-absorbable sutures.
In cases were the proximal stump cannot be found or there is significant muscle fiber loss, other procedures can be done in order to improve the eye position when looking straight forward.
These procedures include:
- Transpositions of other extraocular muscles
- Tethering procedures.
Transposition procedures should never be performed at the time of acute injury and presumed extraocular muscle loss.3
Transposition of recti or oblique muscles will serve the purpose of creating alternative ducting forces to the injured muscle.1,27,28
The transpositions can be full or partial-tendon width, with or without augmentation carried out by resecting the transposed muscles or by adding a posterior scleral suture.
These procedures always carry the risk of anterior segment ischemia, especially if full tendons are transposed. Nishida et al29,30 recently reported a technique of transposition without splitting nor disinserting the distal ends of the muscles from their insertions, which protects anterior segment circulation. A 6-0 or 5-0 nonabsorbable suture is inserted through each temporal margin of vertical recti at approximately one third of the width from the edge at a distance of 8 to 10 mm behind the insertion. The same suture also is inserted through each scleral wall at a distance of 10 to 12 mm behind the limbus at the superotemporal or inferotemporal quadrant. Then, the lateral margin of each vertical rectus muscle is transposed superotemporally or inferotemporally and sutured to the sclera.
For loss or significant injury of the inferior rectus, inferior oblique anterior transposition has demonstrated to be a very good procedure for improving the hypertropia in these cases.31,32,33,34 Anterior transposition of the inferior oblique muscle creates an inferior anchor to the globe. The neuromuscular bundle that enters the belly of the inferior oblique muscle 15 mm posteromedial to its insertion into the globe, serves as a firm posterior attachment site after an anterior transposition is done.35
In cases where muscle transpositions have failed or the risk of anterior segment ischemia is high, tethering procedures provides the surgeon with another option to improve the eye alignment in primary position. This technique seeks to anchor the globe in a better position using diverse materials like temporalis fascia, fascia lata, superior oblique tendon or non-absorbable sutures, that ties the globe to the orbital walls.36,37,38,39
Conclusion
- Trauma to an extraocular muscle without globe or eyelid involvement is rare but can occur.
- Meticulous examination of the globe should always be done to rule out associated injury to the globe.
- Determining the condition of the compromised muscle is very important to plan for the best strategy in managing the case.
- Crucial information for the management of the patient can be obtained through detailed orbital imaging via CT scan or MRI.
References
- Del Monte MA. Management of Direct Extraocular Muscle Trauma. Amer Orthoptic Jrnl. 2004;54:1.
- Murray AD. Slipped and lost muscles and other tales of the unexpected. Philip Knapp Lecture. J AAPOS. 1998; 2:133-143.
- Murray AD. An Approach to Some Aspects of Strabismus from Ocular and Orbital Trauma. Middle East Afr J Ophthalmol. 2015; 22(3):312-319.
- Ludwig IH, Brown MS. Strabismus due to flap tear of a rectus muscle. Trans Am Ophthalmol Soc. 2001; 99:53-63.
- Ludwig IH, Brown MS. Flap tear of rectus muscles: an underlying cause of strabismus after orbital trauma. Ophthal Plast Reconstr Surg. 2002; 18(6):443-449.
- Lueder GT. Orbital Causes of Incomitant Strabismus. Middle East Afr J Ophthalmol. 2015; 22(3):286-291.
- Wei LA, Durairaj VD. Pediatric orbital floor fractures. J AAPOS. 2011;15:173-180.
- Jordan DR, Allen LH, White J , Harvey J, Pashby R, Esmaeli B. Intervention within days for some orbital floor fractures: the white-eyed blowout. Ophthal Plast Reconstr Surg. 1998; 14:379-390.
- Raab EL, Ackert JM, Ostrovsky A. Rectus muscle flap tear as an independent cause of restricted motility. J AAPOS 2012; 16:386-388.
- Seiff SR, Good WV. Hypertropia and the posterior blowout fracture: Mechanism and management. 1996;103:152-156.
- Tapiero B, Riss I, Dominguez, M, Le Rebeller MJ. A propos d'un cas d'hématome organisé du droit supérieur d'origine contusive [A case of organized hematoma of the upper right muscle caused by contusion] Bull Soc Ophtalmol Fr.1989; 89:1185-1188.
- Krarup, J., De Decker, W. Kompendium der direkten Augenmuskelverletzungen. Klinische Monatsblätter für Augenheilkunde, 181 (6): 437-443.
- Helveston EM, Grossman RD. Extraocular muscle lacerations. Am J Ophthalmol. 1976; 81(6):754-760.
- Henson KJ. Diagnostic tools in the evaluation of strabismus secondary to trauma. Am Orthopt J. 2004;54:2-6.
- Buckley EG. Restrictive strabismus. In: Plager DA, editor. Strabismus Surgery: Basic and Advanced Strategies.Oxford: Oxford University Press; 2004:117–154.
- Kim J, Lee H, Chi M, Park M, Lee J, Baek S. Endoscope-assisted repairof pediatric trapdoor fractures of the orbital floor: characterization and management. J Craniofac Surg. 2010; 21:101-105.
- Sires BS, Stanley RB, Levine LM. Oculocardiac reflex caused by orbital floor trapdoor fracture: an indication for urgent repair. Arch Ophthalmol. 1998; 116:955-956.
- Cobb A, Murthy R, Manisali M, Uddin J, Toma A. Oculovagal reflex in paediatric orbital floor fractures mimicking head injury. Emerg Med J. 2009;26:351-353.
- Underdahl JP, Demer JL, Goldberg RLRosenbaum AL. Orbital wall approach with periorbital imaging for identification and retrieval of lost or transected extraocular muscles. J AAPOS. 2001; 5:230-237.
- Pineles SL, Laursen J, Goldberg RA, Demer JL, Velez FG. Function of transected or avulsed rectus muscles followingrecovery using an anterior orbitotomy approach. J AAPOS. 2012; 16:336-341.
- Wright KW. Recognition and repair of the “lost” rectus muscle. Discussion: 1990;97:136-137.
- Goldberg RA. Is there a “lost”rectus muscle in strabismus surgery? Am J Ophthalmol. 2001;132:101-103.
- Knapp P. Lost muscle. In: Helveston EM, ed. Symposium on Strabismus. Transactions of the New Orleans Academy of Ophthalmology. St. Louis: Mosby; 1978:301–306.
- MacEwen CJ, Lee JP, Fells P. Aetiology and management of the ‘detached’ rectus muscle. Br J Ophthalmol. 1992; 76:131–136.
- Dunlap EA. Surgery of muscle adhesions and effects of multiple operations. Br J Ophthalmol. 1974; 58:307-312.
- Plager DA, Parks MM. Recognition and repair of the “lost” rectus muscle. A report of 25 cases. Ophthalmology. 1990;97:131-136.
- Rosenbaum A L. Costenbader Lecture. The efficacy of rectus muscle transposition surgery in esotropic Duane syndrome and VI nerve palsy. J AAPOS. 2004; 8:409-419.
- Santiago AP,Rosenbaum AL. Selected transposition procedures. In: Rosenbaum AL, Santiago AP, eds. Clinical Strabismus Management: Principles and Surgical Techniques. Philadelphia (PA): Saunders; 1999:476-489.
- Nishida Y, Hayashi O, Oda S. A simple muscle transposition procedure for abducens palsy without tenotomy or splitting muscles. Jpn J Ophthalmol. 2005; 49:179-180.
- Muraki S,Nishida Y, Ohji M. Surgical results of a muscle transposition procedure for abducens palsy without tenotomy and muscle splitting. Am J Ophthalmol. 2013; 156:819-824.
- Olitsky SE, Notaro S. Anterior transposition of the inferior oblique for the treatment of a lost inferior rectus muscle. J Pediatr Ophthalmol Strabismus. 2000; 37:50-51.
- Paysee EA,Saunders RA, Coats DK. Surgical management of strabismus after rupture of the inferior rectus muscle. J AAPOS. 2000; 4:164-167.
- Aguirre-Aquino BI, RiemannCD, Lewis H, Traboulsi EI. Anterior transposition of the inferior oblique muscle as the initial treatment of a snapped inferior rectus muscle. J AAPOS. 2001; 5:52-54.
- Asadi R, Falavarjani KG. Anteriorization of inferior obliquemuscle and downward transposition of medial rectus muscle for lost inferior rectus muscle. J AAPOS. 2006; 10:592-593.
- Stager DR, Weakley DR Jr, Stager D. Anterior transposition of the inferior oblique. Anatomical assessment of the neurovascular bundle. Arch Ophthalmol. 1992; 110:360-362.
- Salazar-León JA, Ramírez-OrtízMA, Salas-Vargas M. The surgical correction of paralytic strabismus using fascia lata. J Pediatr Ophthalmol Strabismus. 1998; 35:27-32.
- VillaseñorSolares J, Riemann BI, Romanelli Zuazo AC, Riemann CD. Ocular fixation to nasal periosteum with a superior oblique tendon in patients with third nerve palsy. J Pediatr Ophthalmol Strabismus. 2000; 37:260-265.
- Goldberg RA, RosenbaumAL, Tong JT. Use of apically based periosteal flaps as globe tethers in severe paretic strabismus. Arch Ophthalmol. 2000; 118:431-437.
- Awad AH, Shin GS, Rosenbaum AL, Goldberg RL. Autogenous Fascia Augmentation of a Partially Extirpated Muscle With a Subperiosteal Medial Orbitotomy Approach. J AAPOS. 1997; 1:138-142.