Establishing the Diagnosis
Definition and Classification
Infantile exotropia is a relatively rare strabismus disorder characterized by outward deviation of one or both eyes. Onset is before age 6 months and persists beyond this age (Figure 1).1,2,3 It is classified as primary infantile exotropia, where patients are healthy with no evidence of systemic or ocular disease (Table 1).2 It usually occurs sporadically,1,4 but may be familial as autosomal dominant inheritance with variable penetrance, as was suggested in one case report.5 Some authors classify early onset intermittent exotropia in this subclassification.2 A list of causes for secondary infantile exotropia can be found in Table 1.
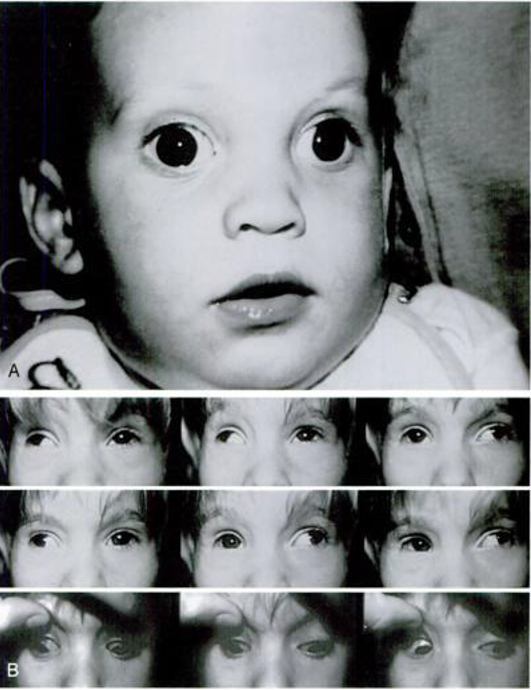
Figure 1. Infantile exotropia. Top: infant at age 6 months. Note large angle of outward deviation. Bottom: same child at age 12 months. Note limited adduction of each eye, pseudo-overaction of all four oblique muscles, creating an X-pattern. (Reprinted with permission from Rosenbaum AL and Santiago A (eds): P Clinical Strabismus Management, Principles and Surgical Techniques, Philadelphia, WB Saunders, 1999.)
| Table 1. Classification of Infantile Exotropia |
|---|
| Primary Infantile Exotropia |
Constant (Congenital) Exotropia
- Idiopathic / Sporadic
- Hereditary / Familial
Early onset intermittent exotropia |
| Secondary Infantile Exotropia |
Ocular Disorders
- Diseases causing vision loss (eg, cataract, retinoblastoma, ptosis)
- Miscellaneous disorders (eg, albinism, nystagmus)
- Other strabismus conditions
- Innervational (eg, 3rd nerve palsy, Duane syndrome)
- Mechanical (eg, Brown syndrome, strabismus fixus, orbital tumor)
- Systemic Disorders
- Neurologic disease (eg, cerebral palsy, hydrocephalus)
- Craniofacial syndrome
- Genetic syndrome (eg, Prader-Willi syndrome)
|
From Table 13-1, Kraft SP. Selected Exotropia Entities and Principles of Management. In: Rosenbaum AL, Santiago A (eds): Clinical Strabismus Management, Principles and Surgical Techniques, 1999; 176-201. Philadelphia, WB Saunders. (Reprinted with permission).
Incidence
Because of its rarity, there are few population-based studies to identify its true incidence. A study by Archer et al identified that only 2 in 3000 (6 per hundred thousand) neonates develop true primary infantile exotropia,6 although other researchers estimated this at 1 in 30,000 births in the general population.4 Older literature suggested that infantile exotropia may be more common in patients of Asian and African descent.3
Etiology
Theories as to neurophysiologic causes of infantile exotropia include (1) deficient development of the convergence system during the vulnerable early period between 2 and 4 months of age;6, 7 (2) monocular defocusing and total deprivation from birth;8, 9 (3) disruption of binocular vision shortly after birth, altering the development of normal vergence reflexes;6 (4) disruption of normal binocular processing in the visual cortex.10 Neuro-anatomic causes include (5) asymmetry in muscle structure between the lateral rectus and medial rectus;11 and finally (6) increased diameter of the lateral rectus compared to the medial rectus.12 However, in the latter two studies, whether the deviation caused the changes in the muscle or the muscle anatomy led to the deviation is unclear.2
Clinical Characteristics
Primary infantile exotropia in a patient is heralded by onset of outward deviation before 6 months of age, preferably with confirmation by an ophthalmologist by age 1 year.2 Alternatively, photographs that clearly show the patient’s age at the time a deviation is documented can aid in diagnosis. Notations from family physicians and pediatricians, especially if they are corroborated with a Hirschberg’s corneal light reflex measurement, are particularly helpful. Parents and other persons who have regular contact with the patient usually reliably see the exodeviation because of the large degree of deviation: it almost always exceeds 30 prism diopters (pd), and may be a large as 90pd. Near deviations parallel those at distance but may occasionally be larger.1, 2, 4, 5
The distribution of refractive errors in infantile exotropia is similar to that of the normal infant population.1 Strabismic amblyopia is seen in a minority of patients but is responsive to traditional therapy.1, 4 Dissociated vertical deviation with inferior oblique muscle overaction is observed in the range of 50%-61%, lower than in infantile esotropia.1, 4, 13 Superior oblique overaction may also be an associated finding.1, 4 Latent nystagmus is rare1 but has been reported.14 Pattern deviations may also occur; V patterns are much more commonly observed than A patterns, and X patterns seen in tight lateral rectus syndrome may also occur. Patients with X patterns exhibit pseudo-overaction of all oblique muscles.1, 4, 5,15
Evaluation
Vision
In very young, preverbal babies and children, testing for vision entails evaluating fixation preference. Does the baby prefer to look with one eye? Does one eye deviate more often? Or, does the child alternate fixation? Can it be central? Is it steady? Can it be maintained? This helps identify patients with amblyopia, which should be treated either with occlusion or penalization. (See chapters on amblyopia [ADD LINK TO AMBLYOPIA]). Any significant refractive error obtained following cycloplegic refraction should be corrected, and amblyopia treatment should be started once that diagnosis is established. Patients should be reevaluated after at least two weeks of spectacle wear and amblyopia treatment.
Strabismus/Motility Evaluation
Strabismus evaluation should commence with evaluation of the relationship of the pupillary axis to the visual axis. Patients with positive angle kappa, or those whose pupillary axis is displaced temporal to the visual axis, may have a pseudo-exotropia appearance. There will be no movement on alternate prism cover test in this situation. True infantile exotropia will have nasally directed refixation movements as the alternate prism cover test is performed until neutralization or no movement is achieved. Whenever possible, not only should primary gaze deviations with distance fixation be measured, but also those in up- and down-gaze, to identify A, V, or Y pattern deviations. Lateral gazes should also be assessed to check for horizontal noncomitance. X-patterns may be observed in tight lateral rectus syndromes because of lateral rectus contractures with pseudo-overactions of all oblique muscles in longstanding deviations.2
The process is repeated for near fixation, especially in the functional gazes of primary or straight gaze as well as down gaze. In the very young child who will not cooperate for alternate prism cover testing either at distance or near fixation, the Krimsky or modified Krimsky test at near may be all that is feasible to estimate the degree of the deviation. Although splitting of prisms is not as accurate as having the base-in prisms in front of one eye, this is more acceptable than stacking prisms of the same direction in front of an eye. Sensory tests for fusion will be difficult to do in the very young child, and will be poor even for the cooperative child because of the large angle of deviation that impedes fusion.
It is easier to evaluate the presence of concomitant vertical deviations and dissociated vertical deviations once the horizontal deviation is corrected using free prisms. The alternate prism cover test, using base-up prisms for neutralization in front of the hypotropic eye until neutralization is achieved, defines the true vertical deviations. The simultaneous prism cover test measures dissociated vertical deviation.
Slit-lamp biomicroscopy and posterior pole evaluations complete the strabismus assessment. Other tests that may be considered in the cooperative child include saccadic velocity analysis, passive forced duction testing, and the active force generation test.16
Differential diagnosis
Aside from a positive angle kappa that has an eye that appears to be deviated outward, the misalignment should be differentiated from early onset intermittent exotropia. Patients with positive angle kappa, although showing a nasally displaced Hirschberg’s corneal light reflex, will have no refixation movements on alternate prism cover tests, and will have good sensory fusion. On the other hand, patients with early onset intermittent exotropia will exhibit refixation movements on the alternate prism cover test, but will also typically do well on sensory tests because bifoveal fixation is not lost until later in the course of the disease.13
Treatment
Non-surgical management
As with patients who have any type of strabismus, amblyopia should be addressed with treatment such as occlusion or penalization, and refractive error corrected. This helps in stabilizing the degree of deviation, but is unlikely to lead to resolution of the exotropia.2 Those who improve with occlusion therapy of the dominant eye1 are more likely to have early onset intermittent exotropia than true infantile exotropia.2 Orthoptics, especially convergence exercises, can be tried but is not likely to be successful because of the large angle of deviation and because the patient’s age precludes effective cooperation with the exercises.
In the absence of amblyopia or eye preference, alternate occlusion therapy as anti-suppression therapy can be instituted, just as it is done for intermittent exotropia.17 Long-term alternate occlusion reverses the nasal versus temporal smooth pursuit asymmetry in patients with infantile esotropia.10 Whether this is true for infantile exotropia is unclear, but results from patients with infantile esotropia suggest it may still be prudent to do alternate occlusion for infantile exotropia while awaiting surgical correction.2
Botulinum toxin injection to the lateral rectus (LR) muscle, typically 2.5-5.0 units to both lateral rectus muscles, can be offered as an alternative to surgery. This technique minimizes secondary vertical deviation and ptosis that sometimes accompany higher doses or unilateral injections.18 The experience with botulinum is obtained mostly from the more common intermittent exotropia, and is fraught with recurrence.19 There are few studies of infantile exotropia treated with botox. Fewer than 50% of patients with constant exotropia responded to botulinum toxin injection of one LR muscle.20
Surgical management
Surgery is required almost universally in cases of true infantile exotropia.
Timing of surgery
Surgery for infantile exotropia should be performed within the first six months of life to maximize potential for attaining single binocular vision with stereopsis.4 Reasonable sensorimotor results are obtained in healthy infants aligned before age 2 years.1, 4, 21, 22 Experts agree that once diagnosis is made, after only a few weeks of follow-up to establish repeatable, reproducible angles of deviation and amblyopia treatment has commenced, surgery should be performed with minimal delay. Earlier surgical intervention affords the best chance of attaining good alignment before age 2 years, because reoperations are common, due not only to undercorrections, but also to dissociated vertical deviations or oblique muscle dysfunction.1, 5, 21, 22, 24, 25, 26
Surgical procedure
The goal of surgery is to align the patient’s eye to within 8PD of orthotropia.2 The lateral rectus can be recessed, and the medial rectus muscle resected or plicated, based on established surgical tables. Surgeons have varying preference, with different permutations all reported in the literature: bilateral lateral rectus recessions, lateral rectus recession with medial rectus resection, and even 3- or 4- horizontal muscle surgery. Despite the risk of developing monofixation esotropia with foveal suppression in patients with slight overcorrection in early surgeries, this situation is rare. A much more common result is undercorrection. Hence, more experts suggest a purposeful targeting of a slight overcorrection in the immediate postoperative period.1, 2, 4 One recent study has suggested reducing the lateral rectus recession by 1-2 mm from typical surgical tables to reduce the risk of overcorrection in this very young sensory labile population.27 Fresnel prisms can be used to correct any residual deviation, as well as overcorrections, to prevent foveal suppression.
Outcomes
A recent retrospective review showed that both motor and sensory outcomes can be good even in early-onset constant exotropia with all patients in their group of 34 testable patients showing gross stereopsis, achieving even bifoveal fixation in 29%.28 In an earlier series that compared patients with intermittent and infantile exotropia, however, gross stereopsis following surgical alignment was reported in only 70% of patients, where none achieved bifoveal fixation.29 Testing done at around age 6 in another series showed patients with infantile exotropia showing stereopsis of less than or equal to 100 arc seconds, performing dismally as compared with those with early onset intermittent exotropia who had excellent stereopsis of greater than or equal to 60 arc seconds.26 Exotropic redrifts are common after surgery, especially in patients with larger preoperative distance deviation.31,32 After at least 3 years of observation, redrifts exceeding 10 PD were observed in 41%.33
In a recent paper, authors suggested that postoperative surgical outcomes appear to be influenced more by the duration of the misalignment, rather than the age at surgery.30 This would suggest that the timing of early surgery is of equal particular importance in the management of infantile exotropia and infantile esotropia.
References
- Biglan AW, Davis JS, Cheng KP, et al. Infantile exotropia, J Pediatr Ophthalmol Strabismus, 1996; 33: 79-84.
- Kraft SP. Selected Exotropia Entities and Principles of Management. In: Rosenbaum AL & Santiago A (eds):P Clinical Strabismus Management, Principles and Surgical Techniques, pp 176-201. Philadelphia, WB Saunders, 1999.
- von Noorden GK and Campos EC. Exodeviations. In: Binocular Vision and Ocular Motility, Theory and Management of Strabismus, 356-376. St. Louis, Mosby, 2002.
- Biedner B, Marcus M, David R, et al: Congenital constant exotropia: surgical results in six patients. Binocular Vision Eye Muscle Surg Q. 1993; 8: 137-140.
- Brodsky MC, Fritz KJ. Hereditary congential exotropia: A report of three cases. Binocular Vision Eye Muscle Surg Q. 1993; 8: 133-136.
- Archer SM, Sondhi N, Helveston EM: Strabismus in infancy. 1989; 96: 133-137.
- Aslin RN. Development of binocular fixation in human infants. J Exp Child Psychol. 1977; 23: 133-150.
- Quick MW, Tigges M, Gammon JA, et al. Early abnormal visual experience induces strabismus in infant monkeys. Invest Ophthalmol Vis Sci. 1989; 30: 1012-1017.
- Tusa RJ, Repka MX, Smith CB, et al. Early visual deprivation results in persistent strabismus and nystagmus in monkeys. Invest Ophthalmol Vis Sci. 1991; 32: 134-141.
- Tychsen L. Infantile Esotropia: Current Neurophysiologic Concepts. In: Rosenbaum AL & Santiago A (eds):P Clinical Strabismus Management, Principles and Surgical Techniques, 117-138. Philadelphia, WB Saunders, 1999.
- Rosenbaum AL, Egbert JE, Keogan T, et al: Length-tension properties of extraocular muscles in patients with esotropia and intermittent exotropia. Am J Ophthalmol. 1994; 117: 791-799..
- Hou JW, Fukatsu H, Ishigaki T: MR Imaging in patients with strabismus. Chin Med J. (Eng) 1994; 107: 631-635.
- Choi YM, Kim SH. Comparison of clinical features between two different types of exotropia before 12 months of age based on stereopsis outcome. Ophthalmology. 2013; 120: 3-7.
- Mein J, Harcourt B: Non-paralytic strabismus—early onset strabismus. In: Diagnosis and Management of Ocular Disorders, 221. London, Blackwell Science, 1986.
- Biglan A. Pattern Strabismus. In: Rosenbaum AL & Santiago A (eds):P Clinical Strabismus Management, Principles and Surgical Techniques, 202-215. Philadelphia, WB Saunders, 1999.
- Santiago AP and Rosenbaum AL. Tests of Muscle Function. In Rosenbaum AL & Santiago A (eds):P Clinical Strabismus Management, Principles and Surgical Techniques, pp ????. Philadelphia, WB Saunders, 1999.
- Hatt SR, Grananaraj L. Interventions for intermittent exotropia. Cochrane Database Syst Rev. 2013; 5: CD003737. Published online 2013 May 31. doi: 1002/14651858.CD003737.pub3
- McNeer KW, Magoon EH, Scott AB. Chemodenervation Therapy: Technique and Indications. In Rosenbaum AL & Santiago A (eds):P Clinical Strabismus Management, Principles and Surgical Techniques, pp 423-432. Philadelphia, WB Saunders, 1999.
- Spencer RF, Tucher MG, Choo KY, et al: Botulinum toxin management of childhood intermittent exotropia. Ophthalmology 1997; 11: 1762-1767.
- Scott AB, Magoon EH, McNeer KW, et al. Botulinum treatment of childhood strabismus. 1990; 97: 1434-1438.
- Hiles DA, Biglan AW: Early surgery of infantile exotropia. Trans Pa Acad Ophthalmol Otolaryngol. 1983; 36, 161-168.
- Paik HJ, Yim HB. Clinical effect of early surgery in infantile exotropia. Korean J Ophthalmol. 2002; 16: 97-102.
- Rubin SE, Nelson LB, Wagner RS, et al. Infantile exotropia in healthy children. Ophthalmic Surgery. 1988; 19: 792-794.
- Park JH, Kim SH. Clinical features and the risk factors of infantile exotropia recurrence. Am J Ophthalmol. 2010; 150: 464-467.
- Yoo EJ, Kim SH. Optimal surgical timing in infantile exotropia. Can J Ophthalmol. 2014; 49: 358-362.
- Choi YM, Kim SH. Comparison of clinical features between two different types of exotropia before 12 months of age based on stereopsis outcome. 2013; 120: 3-7.
- Nam KT, Kim SH. Traditional and reduced recession surgical dosage for bilateral lateral rectus recession for infantile exotropia. Br J Ophthalmol. 2014; 98: 1420-1423.
- Suh SY, Kim MJ, Choi J, et al. Outcomes of surgery in children with early-onset exotropia. Eye. (Lond) 2013; 27: 836-840.
- Hunter DG, Kelly JB, Buffenn AN, Ellis FJ. Long-term outcome of uncomplicated infantile exotropia. J AAPOS. 2001; 5: 352-356.
- Yoo EJ, Kim SH. Optimal surgical timing in infantile exotropia. Can J Ophthalmol. 2014; 49: 358-362.
- Yam JC, Chong GS, Wu PK, et al. Preoperative factors predicting the surgical response of bilateral lateral rectus recession surgery in patients with infantile exotropia. J Pediatr Ophthalmol Strabismus. 2013; 50: 245-250.
- Yam JC, Chong GS, Wu PK, et al. Prognostic factors predicting the surgical outcome of bilateral lateral rectus recession surgery for patients with infantile exotropia. Jpn J Ophthalmol. 2013; 57: 481-485.
- Yam JC, Wu PKW, Chong GS, et al. Long-term ocular alignment after bilateral lateral rectus recession in children with infantile and intermittent exotropia. J AAPOS. 2012; 16: 274-279.