Sutures have been the gold standard for many years for wound closure following clear corneal cataract surgery when a wound does not properly self-seal. However, they are not ideal. Therefore, alternative methods of wound closure are currently under investigation, such as the use of hydrogel wound sealant.
The problems with sutures
Sutures are time-consuming to place, can induce astigmatism, may require removal and often cause conjunctival hemorrhage. Additionally, they can be a nidus for infection, inflammation and neovascularization.
Wounds closed with sutures also have been known to leak. An initial wound leak study (n=21) sought to challenge sutured incisions during intraocular pressure fluctuations, which normally occur when patients touch or rub their eyes. The team of researchers with whom I work developed an ocular force gauge to reproducibly test corneal incisions. We used it to expose eyes to up to 1 ounce of force. Leak rates were 36 percent in single-plane incisions (n=11) and 10 percent in biplane incisions (n=10).1
A larger study included the results of 176 patients who underwent cataract surgery at 23 centers in the United States and attended all follow-up visits. They were evaluated for fluid egress prior to suture placement using the ocular force gauge. If the wound leaked with 1 ounce of force or less, a 10-0 nylon suture was placed using a 3-1-1 technique (explain?) with a buried knot. Then wounds were re-challenged using the ocular force gauge and were evaluated for the prevention of fluid egress. Sutures were removed at day 28 per physician discretion.
The study found that 33 percent of sutured wounds leaked in the immediate postoperative period with 1 ounce or less of force applied. Two additional eyes exhibited leakage within the first seven days postoperatively. Incision architecture did not influence leak rates.
Just over 30 percent of eyes experienced at least one device-related adverse event: subconjunctival hemorrhage; induced corneal astigmatism; infection; corneal edema; eye pain, irritation or discomfort; foreign-body sensation; elevated intraocular pressure; or other suture-related complications. And 12.6 percent of eyes required premature suture removal due to an adverse event.
An alternative to sutures
Providing an alternative to sutures, a new ocular sealant (ReSure Sealant, Ocular Therapeutix, Inc., Bedford, Mass.) has recently been evaluated in a clinical trial and was found to effectively prevent wound leaks in 95.9 percent of cases under the same evaluation with the ocular force gauge.2
This clinical study, which was conducted at 24 ophthalmic clinical practices in the United States, evaluated the safety and effectiveness of the sealant compared with sutures to prevent fluid egress from clear corneal incisions in the immediate postoperative period following uneventful cataract surgery. In this study, 488 of 500 healthy patients undergoing uncomplicated clear corneal cataract surgery exhibited leakage at the time of surgery. Of these, 48.8 percent leaked spontaneously, and an additional 25.4 percent leaked with minimal touch pressure using an ocular force gauge.1
The study randomized the 488 patients who demonstrated leakage to receive either the sealant or a nylon suture at the main incision site. Incision leakage was re-evaluated at 1, 3, 7 and 28 days postoperatively.
Twelve of the 295 eyes in the sealant group (4.1 percent) exhibited leakage of the wound with provocation (see Figure 1) compared with 60 of 176 eyes in the suture group (34.1 percent), which was a statistically significant difference (P < 0.0001). The overall incidence of device-related adverse ocular events reported for patients treated with the sealant was significantly lower than for those treated with sutures (1.6 percent versus 30.6 percent, P < 0.0001).
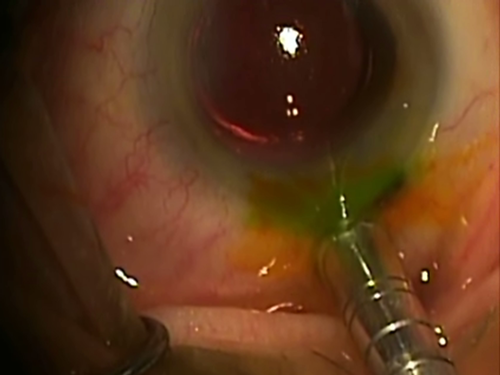
Figure 1: In the pivotal trial, the sealed corneal incision was tested for its integrity with an ocular force gauge.
How a hydrogel wound sealant works
The hydrogel sealant described here is composed of polyethylene glycol (PEG), trilysine and buffering salts, and is more than 89 percent water. It is applied to a dry surface as a liquid and polymerizes into an adherent hydrogel in less than 30 seconds (see Figure 2). It contains a blue colorant that aids visualization for accurate placement and observation. Within hours, the colorant dissipates, leaving clear sealant on the eye (see Figure 3).
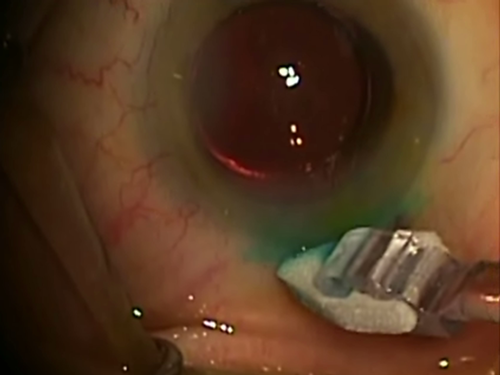
Figure 2: The hydrogel sealant is applied to the ocular surface with a soft applicator.
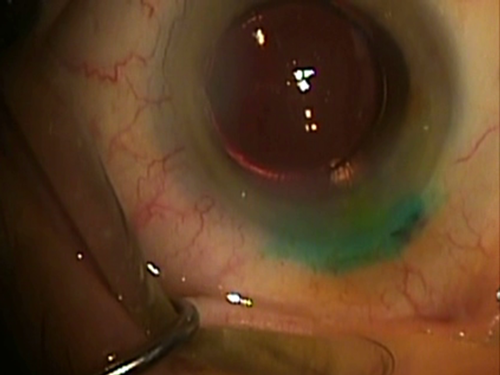
Figure 3: Freshly gelled on the eye, the hydrogel sealant has a soft texture. The blue color fades within one hour, rendering the sealant invisible, except to slit lamp examination.
The pliable nature of hydrogels allows them to conform to the corneal tissue, creating a smooth surface so as not to induce astigmatism or create foreign body sensation. Some ophthalmologists have used cyanoacrylate glue off-label to temporarily seal a wound leak, but cyanoacrylate polymerizes into a very hard and brittle structure that often requires the placement of a bandage contact lens on the eye to address the associated patient discomfort. The hydrogel sealant has a soft texture, is designed to dissolve or slough off within seven days and does not need to be removed.
Studies show that most of the sealant typically stays on for about three days and sloughs off as the wound re-epithelializes. Therefore, the sealant remains on the wound during the immediate postoperative period when wounds are most vulnerable to leaks and is a great way to provide additional protection for the wound.
References
- Masket S, Hovanesian J, Raizman M, Wee D, Fram N. Use of a calibrated force gauge in clear corneal cataract surgery to quantify point-pressure manipulation. J Cataract Refract Surg. 2013;39(4):511-518.
- Masket S, Hovanesian JA, Levenson J, et al. Randomized comparison of a hydrogel sealant versus sutures for prevention of fluid egress following cataract surgery. Ophthalmology. Submitted for publication.