Salzmann’s nodular degeneration (SND) is a slowly progressive corneal degeneration that has been associated with ocular surface inflammation and trauma but also can be idiopathic. Management includes observation in asymptomatic patients, medical treatment with lubricants or topical medications, and surgical treatment with superficial keratectomy, phototherapeutic keratectomy (PTK), and lamellar or penetrating keratoplasty. Superficial keratectomy can be used to treat the vast majority of these lesions, with lamellar or penetrating keratoplasty reserved for lesions with associated scarring deep within the stroma.
While initial descriptions of SND in the literature note that it may develop following keratitis,1,2 more recent studies have identified associations with epithelial basement membrane dystrophy, contact lens wear, meibomian gland disease/blepharitis, dry eye and previous ocular surgery.3-5 Salzmann’s nodules may be unilateral or bilateral and are found more frequently in women.4,5 Recognition of this condition is important as it is has a good prognosis if readily treated.
Diagnosis
SND is diagnosed primarily by slit-lamp examination. The nodules appear white, grey or bluish and slightly elevated in the superficial corneal layers and may have an associated iron line (Figure 1). They may appear as single or multiple lesions and are often seen in the mid-periphery (Figure 2). They can be subtle and may be overlooked, especially in the superior cornea where they may hide beneath the upper eyelid during examination.
Figure 1: This slit-lamp photograph demonstrates an irregular elevated nodule with an associated iron line.
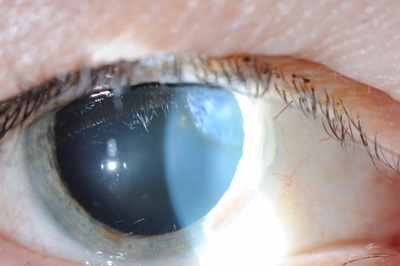
Figure 2: Multiple elevated white-grey nodules are seen in the inferior mid-peripheral cornea.
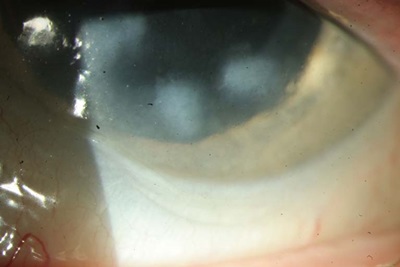
Photo Credit: Debra Cantrell, COA.
Corneal topography can aid in evaluation and monitoring of nodules by showing any associated astigmatism within the visual axis. Histopathological findings include an epithelium of variable thickness overlying a hyaline plaque which may extend into and sometimes replace Bowman’s layer.2,6
Salzmann’s nodules may decrease vision due to encroachment on the visual axis or indirectly by inducing irregular astigmatism, hyperopia and tear film abnormalities. Indications for removal include decreased vision, recurrent erosions, foreign body sensation and tearing. Prior to cataract surgery, the nodules may affect biometry measurements and removal may be warranted to obtain the best possible measurements prior to intraocular lens selection.
Preoperative considerations
Removal of Salzmann's nodules can be performed at the slit lamp, in a minor procedure room with a microscope, or in the operating room, depending on the number and extent of the nodules as well as the patient disposition.
SND may sometimes cause a progressive hyperopic shift with a subsequent myopic shift following removal of nodules,7 and patients should be counseled to anticipate a change in refraction and spectacle prescription.
Surgical instrumentation
Many types of instruments can be used to remove the nodules. Often all that is required is 0.12 mm, Colibri or jeweler’s forceps. In addition, a crescent or Beaver blade or a Tooke knife may assist with dissection. Vannas scissors are usually not necessary but may be used to amputate the nodule when it is well adhered to the limbus. Cautery is rarely required as most bleeding at the limbus resolves spontaneously or with manual pressure from cellulose spears.
Surgical technique
Immediately prior to removal under a microscope, slit-lamp examination is helpful to identify the location and extent of the nodules as they may be difficult to visualize under the microscope. It may also be helpful to identify an edge of a lesion that appears well demarcated as a location that would be best for initial grasping.
Next the patient is prepped and topical anesthetic is administered. For most nodules, epithelial debridement is not necessary. If there is associated epithelial basement membrane dystrophy or to improve visualization of poorly visible nodules, epithelial debridement can be performed manually using a blade or spatula and with or without the assistance of alcohol.8
Forceps are used to grasp the edge of the nodule firmly and raise this edge. If using 0.12 mm or Colibri forceps, they can be spread widely and the two-pronged arm used to rake toward a border of the lesion until the edge is identified and can be grasped. Once an edge is raised, a plane of dissection is visible and usually the nodule can be peeled off by pulling the edge toward the periphery or parallel to the limbus.
If there is difficulty with identification of the plane of dissection or stripping of the nodule, a blade can be used along with the forceps to carefully dissect at the edge of the lesion until a plane is established. If a nodule is well adhered to the limbus and cannot be easily stripped (usually due to an associated fibrovascular pannus), scissors can be used to amputate the lesion along the limbus.
Following removal of the nodules, the underlying corneal surface is often smooth. However, some eyes may have irregularities of the corneal surface due to defects in Bowman’s layer and superficial stroma. In these cases, further treatment with a diamond burr9 or PTK10,11 can be used to smooth these corneal irregularities. When using PTK to treat residual irregularities or scarring, up to 30 µm or more of ablation may be required, especially if a fluid-masking agent is needed for severe irregularities.10
The off-label use of mitomycin C (MMC) also has been reported following superficial keratectomy12 and/or PTK13,14 without recurrences during limited follow-up. MMC 0.02% can be applied on a cellulose sponge for 20 to 30 seconds followed by copious irrigation with saline. We typically reserve the use of MMC for cases with extensive nodules, associated scarring and neovascularization or for recurrences.
Postoperative management
A topical antibiotic is given and a bandage contact lens may be used during re-epithelialization. Because SND is associated with previous corneal inflammation, we also taper steroids, typically over one month, with the goal of reducing the chances of scarring and recurrence. It is important preoperatively and postoperatively to manage any concurrent or underlying ocular surface disease, including dry eye and meibomian gland dysfunction, in order to promote healing and potentially reduce the risk of recurrence.
References
- Salzmann M. Uber eine abart der knotchenformigen Hornhautdystrophie. Z Augenheilkd. 1925;57:92-99.
- Vannas A, Hogan MJ, Wood I. Salzmann’s nodular degeneration of the cornea. Am J Ophthalmol. 1975;79:211-219.
- Werner LP, Issid K, Werner LP, et al. Salzmann’s corneal degeneration associated with epithelial basement membrane dystrophy. Cornea. 2000;191:121-123.
- Farjo AA, Halperin GI, Syed N, et al. Salzmann’s nodular corneal degeneration clinical characteristics and surgical outcomes. Cornea. 2006;25:11-15.
- Hamada S, Darrad K, McDonell PJ. Salzmann’s nodular corneal degeneration (SNCD): Clinical findings, risk factors, prognosis and the role of previous contact lens wear. Cont Lens Ant Eye. 2011;34:173-178.
- Yoon KC, Park YG. Recurrent Salzmann’s nodular degeneration. Jpn J Ophthalmol. 2003;47:401-404.
- Oster JG, Steinert RF, Hogan RN. Reduction of hyperopia associated with manual excision of Salzmann’s nodular degeneration. J Refract Surg. 2001;17:466-469.
- Roszkowska AM, Colosi P, De Grazia L, et al. One year outcome of manual alcohol-assisted removal of Salzmann’s nodular degeneration. Graefes Arch Clin Exp Ophthalmol. 2009;247:1431-1434.
- Malta JB, Soong HK. Diamond burr Superficial keratectomy in the treatment of visually-significant anterior corneal lesions. Arq Bras Oftalmol. 2008;71:415-418.
- Das S, Langenbucher A, Pogorelov P, et al. Long-term outcome of excimer laser phototherapeutic keratectomy for treatment of Salzmann’s nodular degeneration. J Cataract Refract Surg. 2005;31:1386-1391.
- Germundsson J, Fagerholm P. Phototherapeutic keratectomy in Salzmann’s nodular degeneration. Acta Ophthalmol Scand. 2004;82:148-153.
- Bowers PJ, Price MO, Zeldes SS, et al. Superficial keratectomy with mitomycin-C for the treatment of Salzmann’s nodules. J Cataract Refract Surg. 2003;29:1302-1306.
- Khaireddin R, Katz T, Baile RB, et al. Superficial keratectomy, PTK, and mitomycin C as a combined treatment option for Salzmann’s nodular degeneration: a follow-up of eight eyes. Graefes Arch Clin Exp Ophthalmol. 2011;249:1211-1215.
- Marcon AS, Rapuano CJ. Excimer laser phototherapeutic keratectomy retreatment of anterior basement membrane dystrophy and Salzmann’s nodular degeneration with topical mitomycin C. Cornea. 2002;21:828-830.