Manual small-incision extracapsular cataract extraction, or MSICS, has become an extremely efficient and financially feasible technique for cataract removal in situations in which phacoemulsification is problematic, as well as for treating patients in developing countries. Numerous studies.1-3 have compared the efficacy of and postoperative differences between phacoemulsification and MSICS and have found them to be comparable. In this article and video, we present our technique for MSICS as performed at Goutami Eye Institute in Rajahmundry, India.
The MSICS technique
Creating a large scleral pocket—as big as the diameter of the cornea, if necessary—can almost negate the need for postoperative suture removal and reduce any induced astigmatism. This can be performed superiorly or temporally. To begin, a peritomy is performed, and a relaxing incision is made to allow for adequate scleral exposure. An 11 blade is used to make a 6 to 8 mm (depending on the density of the lens) linear incision 2 mm posterior to the limbus. Cauterization may be necessary to control any bleeding in order to enable good visualization. A crescent blade is then used to create a tunnel that extends 2 mm into the cornea and extends at either end so the tunnel takes on a trapezoidal shape (Figure 1). A paracentesis is made and viscoelastic is injected to fill the anterior chamber. A keratome is used to enter the anterior chamber and a capsulorhexis is performed in whatever manner the surgeon prefers. My colleagues and I at Goutami favor a curvilinear capsulorhexis, but the can-opener method or other versions of a capsulotomy can be used as well.
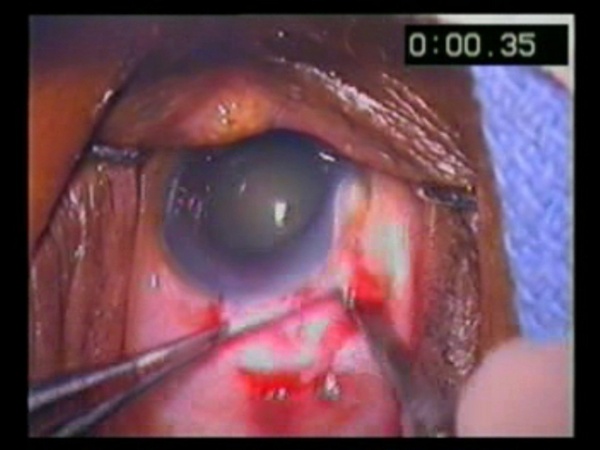
Figure 1
The most important thing about the capsulorhexis is to make it large, around 6 mm. A keratome is then used to enlarge the wound by cutting on the inward stroke to ensure a smooth wound edge (Figure 2). The large capsulorhexis allows ample room to prolapse the nucleus into the anterior chamber, which is done during hydrodissection by placing gentle downward pressure on one pole of the nucleus to prolapse the other end (Figure 3).
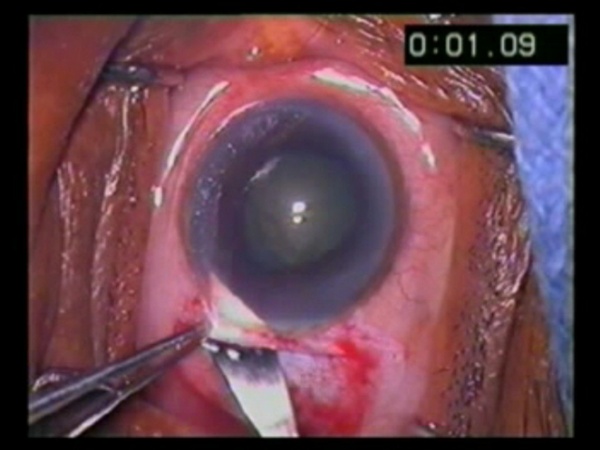
Figure 2
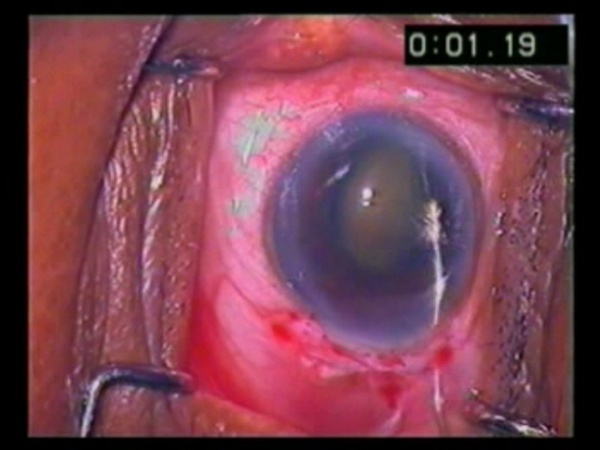
Figure 3
If the capsulorhexis is too small, preventing prolapse of one pole, multiple small nicks can be made in the capsulorhexis edge to aid the surgeon. Please note that multiple nicks are necessary in order to prevent too much tension from building up in one area and causing a radial tear in the capsule. A cannula or other instrument with a sharper tip able to impale the lens can be used to rotate the lens out of the bag. Viscoelastic is then injected onto the lens to protect the endothelium and at the pole opposite the wound to build pressure and enable ease of delivery. A vectis can be used to place pressure on the posterior lip of the wound or inserted to aid delivery of the lens. If it is difficult to deliver the lens, enlarging the wound will often help.
Cortical material is removed in whatever way the surgeon prefers. A lens is placed in the bag or sulcus as needed. Viscoelastic is removed. 10-0 nylon sutures can be placed at the wound if the surgeon desires, but in our experience, a properly constructed wound will preclude the need for sutures. We inject subconjunctival antibiotics after draping conjunctiva back over the wound. This helps keep the conjunctiva in place without sutures.
Comparably good results
Many studies have discussed the feasibility of performing this surgery in developing countries. Multiple studies have demonstrated results with MSICS that are as good as with phacoemulsification.1-4 Postoperative visual acuities and average postoperative astigmatism after MSICS in our study were comparable to the results achieved in these studies.
We believe that the stability of the MSICS wound is due to the funnel-shaped entry created by this technique. It allows the anterior chamber to remain stable during the procedure. Therefore a surgeon can feel confident that there will be a good seal at the wound, even without sutures, much like with a smaller scleral tunnel wound.
References
- Ruit S, Tabin G, Chang D, et al. A Prospective Randomized Clinical Trial of Phacoemulsification vs Manual Sutureless Small-Incision Extracapsular Cataract Surgery in Nepal. American Journal of Ophthalmology. 2007;143(1):32-38.
- Gogate PM, Kulkarni SR, Krishnaiah S et al. Safety and Efficacy of Phacoemulsification Compared with Manual Small-Incision Cataract Surgery by a Randomized Controlled Clinical Trial. Ophthalmology. 2005;112(5):869-874.
- Tabin G, Chen M, Espandar L. Cataract surgery for the developing world. Current Opinions in Ophthalmology. 2008;19(1):55-59.
- George R, Rupauliha P, Sripriya AV, Rajesh PS, Vahan PV, Praveen S. Comparison of endothelial cell loss and surgically induced astigmatism following conventional extracapsular cataract surgery, manual small-incision surgery and phacoemulsification. Ophth Epidemiol. 2005;12(5):293-297.