The links to each individual chapter of the Color Atlas of Gonioscopy are available at the Chapters link, below.
While gonioscopy remains the gold standard by which the angle is evaluated, numerous anterior segment imaging techniques exist to assist in determining anterior segment structure. The two most commonly employed techniques are ultrasound biomicroscopy (UBM) and slit-lamp-based optical coherence tomography (OCT). Additional techniques, such as Scheimpflug photography, can give estimates regarding angle depth; since the angle is not directly evaluated, this is not discussed further here. Both UBM and OCT provide inherent advantages over gonioscopy in that both can provide information about the angle without direct visualization. Each of these technologies can provide information about structures beyond those normally seen on gonioscopic exam, including the ciliary body, posterior iris, and lens. Both techniques can potentially be helpful in augmenting or replacing gonioscopy in situations in which a view of the angle is precluded by corneal edema or other media opacity. At this time, these technologies are not a replacement for gonioscopy. The equipment is costly compared to gonioscopy and compressive evaluation cannot be used. They can, however, provide valuable information regarding the dynamic appearance of the angle in various states of illumination. When gonioscopy and either UBM or OCT are used together, a great deal of structural information about the angle can be obtained.
Ultrasound Biomicroscopy
UBM was first introduced in 1990 by Pavlin, Sherar, and Foster (Pavlin et al, 1990). A 50 MHz transducer is used in a B-scan mode, with tissue penetration of approximately 5 mm. An immersion technique is used to improve image clarity (Pavlin et al, 1991, and Tello et al, 1994). With the patient in the supine position, a 20 mm cup is placed on the eye to hold a coupling medium (methylcellulose or normal saline). The probe is placed within the coupling medium and the images are captured in real time (Liebmann, 2001). A resolution of approximately 25 μm is typically achieved. Although image acquisition is straightforward, reproducible measurements require an experienced examiner and the supine position can alter the physiologic anatomical configuration of the angle.
Optical Coherence Tomography
Anterior segment OCT was first described in 2000 (Hoerauf at al, 2000). That technique utilized a slitlamp adaptation of the original OCT technology, using light at a wavelength of 830 nm, rather than sound waves, to obtain an image based on the reflection of this light back to the probe (Fujimoto et al, 1995). The resolution of the image depends on numerous factors including patient cooperation, tissue opacity, and the wavelength of light used. Since the original design, higher-resolution OCT has become available using light at 1300 nm wavelength (Radhakrishnan, 2005). Axial resolution in this system is typically 18 μm. Anterior segment OCT has the clear advantage over UBM in that it is a noncontact examination and can be performed with the patient sitting upright. Disadvantages include a slightly less dynamic examination and the inability to visualize the ciliary body and the other structures behind the iris.
Applications
At its inception, anterior segment imaging was most frequently used to determine angle anatomy, although its uses have greatly expanded over the years (11‑1 to 11‑8). Specifically, angle occludability and closure can be carefully measured (Pavlin, 1995, and Tello et al, 2002). Iris configuration change after peripheral iridotomy, both in narrow angles and in pigment dispersion syndrome (Pavlin et al, 1992, and Barkana et al, 2007), can also be measured. Additionally, the response of the angle to pupil constriction to light and dark has been studied (See, 2007, Barkana et al, 2007). It is worth noting that gonioscopy can also be used in these situations. One of the most useful aspects of anterior segment imaging is the ability to determine anterior segment configuration not always well appreciated on gonioscopic examination. For example, in plateau iris configuration, anterior segment imaging is very effective in recognizing both the anteriorly rotated ciliary body and the narrow peripheral angle (Pavlin et al, 1992). Similarly, any mass, cyst, or swelling in the ciliary body or posterior iris can be well appreciated. Anterior segment imaging is useful diagnostically in aqueous misdirection, demonstrating the anterior rotation of the ciliary body, and tight apposition of the iris and lens to the cornea (Ishikawa, 2004). Structures such as IOL haptics, filtering blebs, and intraocular foreign bodies have all been evaluated by UBM or anterior segment OCT. Anterior segment OCT also holds particular promise in evaluating the cornea after lamellar surgery. However, these techniques continue to evolve, and at no point should they be used as a substitute for gonioscopic examination of the angle.
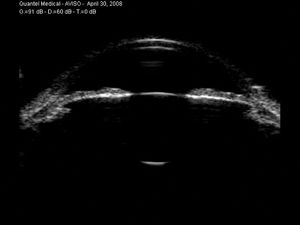
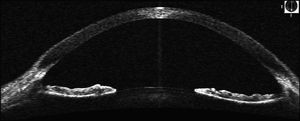
11-1 Normal anterior chamber imaged by UBM.
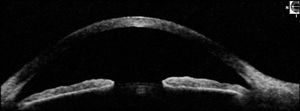
11-2 Normal anterior chamber imaged by anterior segment OCT.
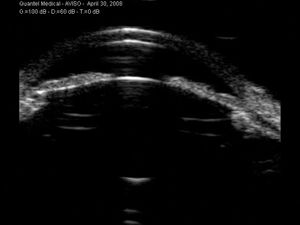
11-3 Narrow angle seen on UBM. Note that the exact angle of the iris insertion can be easily visualized.
11-4 Very narrow angle seen on UBM. The iris is being vaulted forward by the lens, suggesting that peripheral iridotomy may be of limited benefit.
11-5 Iris back-bowing seen on anterior segment OCT in a patient with no prior evidence of pigment dispersion syndrome.
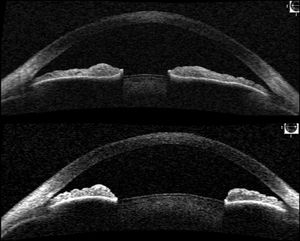
11-6 Evaluation of the angle on anterior segment OCT in light (upper figure) and dark (lower figure). Note the remarkable difference in angle configuration caused by pupil constriction
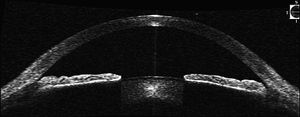
11-7 An example of plateau iris seen on anterior segment OCT. The peripheral iris appears to drop off just before inserting in its normal location.
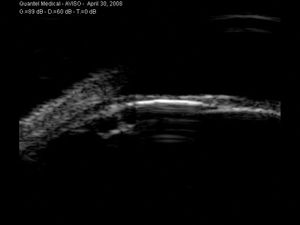
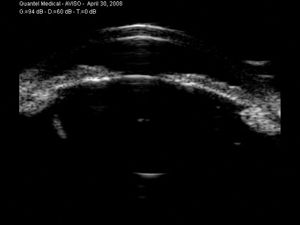
11-8 An example of a posterior iris cyst seen on UBM. The cyst causes focal narrowing of the angle.