EPIDEMIOLOGY
Global Information
- Annually, there are 16 million cases of blindness caused by eye injuries.
- 23 million cases of low vision due to eye injuries
- 19 million cases of monocular blindness due to eye injuries
- Incidence and prevalence studies of ocular trauma are difficult to obtain; however, it is known that internationally, ocular trauma causes significant morbidity and loss of production from accidents that are often preventable.
- In developed countries, the incidence of blindness due to injury was 9/100,000 people, but in developing countries, that rate was 75/100,000.
- Within healthcare centers for eye care, 10%–27% of cases in outpatient departments and 38%– 65% of cases in emergency departments are related to eye trauma or chemical exposure.
Regional Information (Asia)
- A case control study of ocular injury in Hong Kong found that wearing protective eye wear negatively correlated with eye injury in the workplace.
- The Andhra Pradesh Eye Disease Study found that the rate of trauma in Hyderabad was 3.97%, with 1 in 167 people in the population considered to be blind in at least 1 eye secondary to trauma.
- A review of eye trauma in a hospital in Taiwan found that 83.1% of the eye trauma population was male with 48.1% related to work trauma.
- Visual prognosis in this study was very poor, with nearly 40% of patients having a visual acuity of 0.1 after treatment.
DIFFERENTIAL DIAGNOSIS
- Chemical burn
- Corneal or conjunctival lamellar laceration
- Corneal or conjunctival foreign bodies
- Traumatic iritis
- Hyphema
- Iridodialysis and cyclodialysis
- Eyelid or external laceration
- Globe rupture
- Penetrating vs perforating
- With or without foreign body
- Orbital fracture
- Retrobulbar hemorrhage
- Commotio retinae or choroidal damage
- Traumatic optic neuropathy
- Nonaccidental trauma
PATHOPHYSIOLOGY/DEFINITION
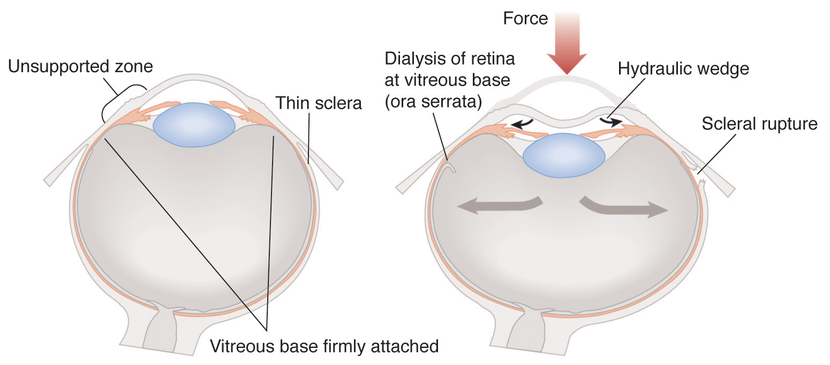
Figure 1. Pathology.
- Blunt force causes peripheral volume displacement with increased “wedge pressure” that causes damage to area of least resistance along the lens, iris root, and trabecular meshwork.
- Lens subluxation, retinal dialysis, optic nerve avulsion and vitreous hemorrhage may also occur.
- Sheering of vessels causes hyphema and force may cause scleral ruptures most likely at thinnest points posterior to the muscle insertion and limbus.
SIGNS AND SYMPTOMS
Signs and symptoms:
- Pain
- Red eye
- Local tenderness
- Facial anesthesia
- Bleeding
- Photophobia
- Foreign body sensation
- Tearing
- Discomfort
- Double vision
- Pain with eye movement
- Visual field defects
- Flashes
- Floaters
- Ecchymosis
- Edema of eyelids
Visual acuity:
- May be decreased based on mechanism and degree of trauma.
Pupils:
- Anisocoria
- Corectopia with peaking of the pupil (highly suspicious for ruptured globe)
- Afferent pupillary defect may be present (Figure 2)
Extraocular movement:
- Restriction in gaze with or without forced duction testing (may indicate entrapment or retrobulbar hemorrhage (Figure 3)
- Pain with eye movement
Intraocular pressure:
- Avoid testing in cases where there is an obvious ruptured globe.
- Pressure may be elevated with retrobulbar hemorrhage, chemical burn, iridodialysis.
- Pressure may be low in globe rupture or initial cyclodialysis.
Visual field:
Color testing:
- May be decreased with optic nerve damage.
External examination, lids and lacrimal system:
- Full or partial thickness laceration involving or not involving the lacrimal system.
- Ptosis may occur.
- Visible orbital fat in the eyelid indicates orbital septum involvement.
Conjunctiva and sclera:
- 360o subconjunctival hemorrhage is suspicious for the presence of a ruptured globe.
- Careful inspection with double eversion of the upper and lower eyelid may reveal crystals from chemical burn, additional lacerations, or foreign body (Figure 4).
- The sclera may be exposed with conjunctival laceration.
- Seidel testing over the sclera may reveal a leak of vitreous indicating perforation of the globe.
- Uveal tissue may prolapse in case of globe rupture (Figure 5)
Cornea:
- Epithelial defects with fluorescein staining ranging from superficial punctate keratopathy in chemical burns to complete loss of epithelium
- Corneal edema and haze (Figure 6)
- Laceration
- Perform Seidel test with fluorescein strip over damaged cornea to assess for leaking of aqueous fluid (Figure 7). Indicate whether lamellar or full thickness .
- Foreign body may be present with small infiltrate surrounding it or a rust ring of multiple retained foreign bodies may be present (Figure 8).
Anterior chamber:
- Hyphema ranges from micro to 100% or “eight ball” (Figure 9). Height should be measured.
- Hypopyon with layering and measurable height may be present.
- Cell or flare may be seen with traumatic iritis.
- Depth of anterior chamber may be reduced or normal with globe rupture.
Iris:
- Tears, iridodialysis (Figure 10) and cyclodialysis (Figure 11)
- Transillumination defects
- Angle recession on gonioscopy with widening of the ciliary body band (Figure 12)
Lens:
- Rupture of the lens capsule may be present.
- Traumatic cataract may develop immediately or later (Figure 13).
- Vossious ring: Anterior capsule may have iris pigmentation from contact during trauma.
- Lens may be displaced or subluxed (Figure 14).
- Siderosis bulbi may occur with iron foreign body (Figure 15, Figure 16).
Retina and vitreous:
- Schaffer’s sign: “tobacco dust” or pigmented cell behind the vitreous
- Possible foreign body
- Confluent areas of retinal whitening with commotio retinae (Berlin edema is whitening in posterior pole) (Figure 17)
- Yellow or white crescent subretinal streak in traumatic choroidal rupture
- Areas of choroidal and retinal necrosis with bare sclera, subretinal, intraretinal, and preretinal hemorrhage in chorioretinitis sclopetaria (Figure 18)
- Multilayered retinal hemorrhages in preretinal, intraretinal and subretinal layers are often too many to count in inflicted childhood trauma (Figure 19)
- Retinal detachment
Optic nerve:
- May initially appear normal
- Pallor with increased intraocular pressure or extensive optic nerve damage
- Hemorrhage and blurring of margins in cases of optic nerve avulsion
- Papilledema may occur in retrobulbar hemorrhage
MANAGEMENT
- Step 1: Assessment of patient stability
- ABCDE: Airway, Breathing Circulation, Disability, Exposure
- Exposure includes chemical exposure to the eye.
- In the case of chemical exposure to the eye, copious irrigation with saline should come first. In the absence of saline, water is appropriate, but neutralizing substances should be avoided.
- A Morgan lens should be used if available.
- Shield the eye, and do not proceed with ocular exam until patient is stable.
- The patient may require emergent medical management prior to ophthalmic examination. Make all attempts to shield the eye prior to examination with hard shield to prevent further damage.
- Never remove intraorbital foreign body prior to full examination.
- Try to obtain information regarding specifics of event (time, chemical, mechanism of injury, low or high velocity projectile, type of material that entered the eye).
- Obtain information about prior ocular surgeries, contact lens wear and visual acuity from friends and family.
- Indicate whether or not the patient was wearing protective eyewear at the time of injury.
- Note any medications with anticoagulation properties.
- Note any family history of personal history of bleeding disorders including sickle cell trait.
- Step 3: Examination and recognition of the problem
- Test both the affected and unaffected eye at time of trauma before any interventions.
- Additional imaging may be necessary including A-scan, B-scan or radiologic testing for further evaluation and should be conducted gently if globe rupture is suspected (Figure 20).
- Step 4: Treatment of underlying problem
- Tetanus prophylaxis is appropriate in most cases.
- Optimal timing of globe repair is within 24 hours of injury.
- Secondary sequelae and symptoms may occur after initial event.
- Angle recession glaucoma, retinal detachment, or traumatic iritis may present days to years after initial trauma. This is an especially important point to discuss with young patients.
- Protective eyewear (eg, polycarbonate lenses) should be worn while performing activities at risk (eg, work, athletics).
- In monocular patients, protective eyewear should be worn at all times.
- Workplace modifications should be made (eg, splash guarded shields, eye wash stations).
CASE STUDY
History of Present Illness
A 23-year-old man was drilling a screw into a metal fence when he felt a sharp pain in his right eye. He was not wearing protective eyewear at the time and presented to the emergency room with a red, painful eye with decreased visual acuity and tearing. The patient had no other trauma. His ABCDEs were cleared and the patient was examined. He had no prior medical or ocular history. He had no history of bleeding disorder and no family history of ocular problems.
Examination
- On examination, visual acuity was decreased to count fingers in the right eye and 20/20 visual acuity in the left eye.
- On slit lamp examination, the patient had edema of the right eyelids, subconjunctival hemorrhage over 180o; corectopia with peaking of the iris (Figure 21), and shallow anterior chamber.
- Testing of intraocular pressure was deferred as well as a dilated fundus exam (Figure 22).
- A computed tomography scan of brain and orbits were performed, which demonstrated an intact globe and absence of foreign body. (Magnetic resonance imaging was not ordered given the possibility of a metallic foreign body.)
Management:
- The patient was admitted, made NPO with bed rest.
- He was given tetanus prophylaxis, systemic antibiotics and analgesia.
- He was taken to the operating room for surgical repair of the cornea with suturing of corneal laceration and dilated fundus exam.
- The patient had no retained foreign body of dilated fundus exam in the OR. He was discharged with postoperative drops and followed closely for signs of infection.
- His visual acuity was 20/800 and 20/20 the following day with IOP of 18 mmHg OU.
Follow-Up:
- Two months later, the patient presented to clinic with visual acuity of 20/200 and 20/20.
- He was found to have a traumatic cataract in the right eye. The patient was taken for lens aspiration via phacoemulsification and intraocular lens implant (Figure 23).
- During the surgery the cornea was hazy superiorly, on formation of the anterior chamber with viscosurgical device after paracentesis, the perforation wound was leaking and the wound as again secured.
- Capsulorrhexis was followed by lens aspiration, and a foldable intraocular lens was implanted.
- Postoperative anterior chamber was formed with IOL in place with minimal lens matter superiorly.
- Patient had vision of 20/60 and 20/20 with IOP of 18 mmHg OU.
- He was advised to wear polycarbonate lenses at all times.
IMAGE LIBRARY
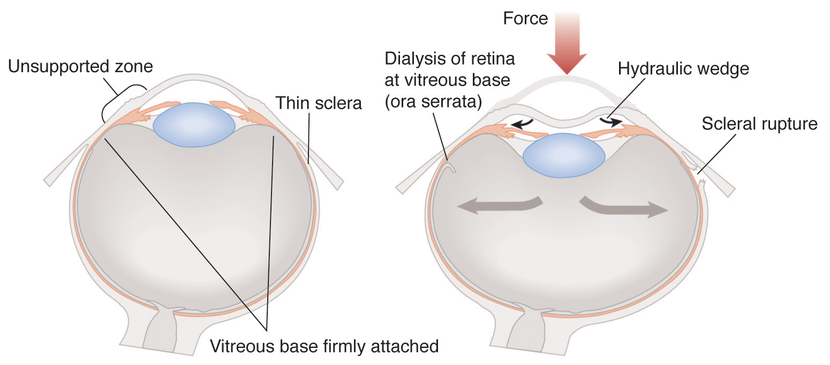
Figure 1. Blunt force causes peripheral volume displacement with increased “wedge pressure” that causes damage to area of least resistance along the lens, iris root, and trabecular meshwork. Lens subluxation, retinal dialysis, optic nerve avulsion and vitreous hemorrhage may also occur. Sheering of vessels causes hyphema and force may cause scleral ruptures most likely at thinnest points posterior to muscle insertion and limbus. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
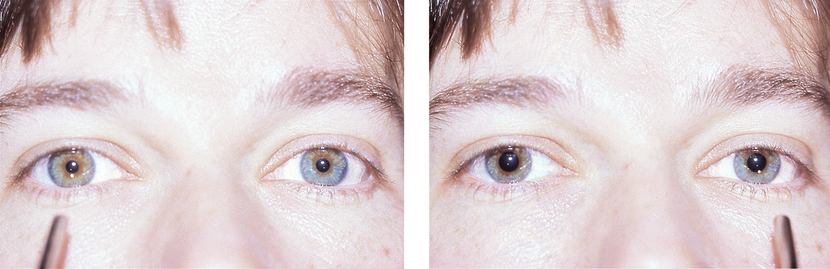
Figure 2. Testing for an afferent pupillary defect (also known as a relative afferent pupillary defect) is performed by the swinging flashlight test with a patient in dim light fixating at a distant target. They first eye is stimulated with pen light for 2 seconds and then quickly moved to contralateral eye for 2 seconds. Constriction of the pupil is noted both indirect light and response when light is placed in contralateral eye (consensual response). An APD is detected when the pupil dilates with administration of the light after it is swung from the contralateral eye. It is important to test the pupils with lights at different levels as some subtle APDs can only be recognized with lower light. (Reproduced, with permission, from Kline LB. Neuro-ophthalmology. Basic and Clinical Science Course, Section 5, American Academy of Ophthalmology, 2012–2013.)
Figure 3. Blunt trauma to the eye and orbit. A. The child is not able to elevate his left eye. Note that the patient is pharmacologically dilated. B. Coronal CT scan demonstrates inferior rectus entrapment (red arrow) secondary to orbital floor fracture. (Reproduced, with permission, from Holds JB. Orbit, Eyelids, and Lacrimal System. Basic and Clinical Science Course, Section 7, American Academy of Ophthalmology, 2013–2014.)
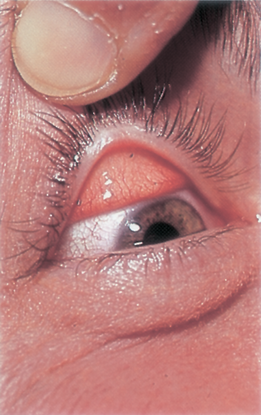
Figure 4. Foreign bodies on everted upper eyelid. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
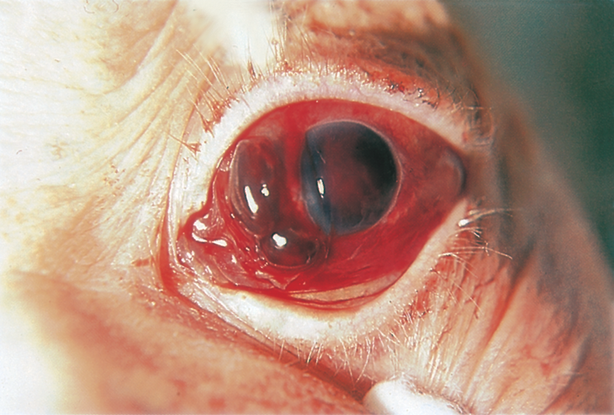
Figure 5. Uveal tissue prolapse through scleral laceration after blunt trauma. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)

Figure 6. Corneal edema and haze with alkali burn. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
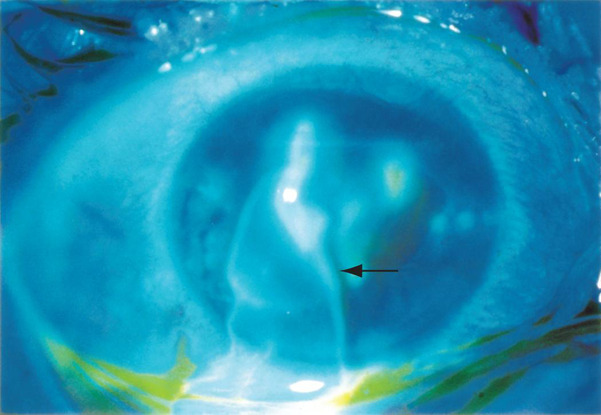
Figure 7. Leakage of aqueous humor from the anterior chamber following corneal laceration. Uveal tissue may prolapse in case of globe rupture. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
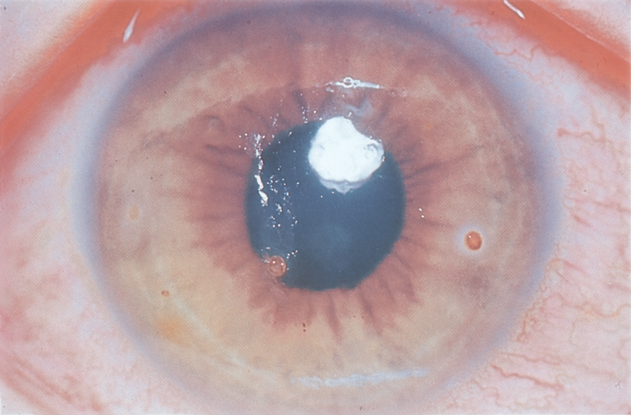
Figure 8. Corneal rust ring. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
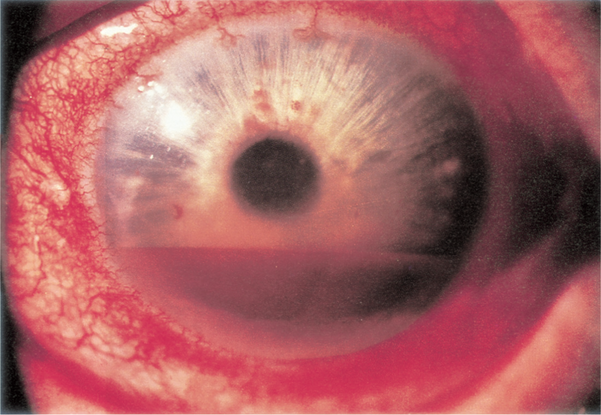
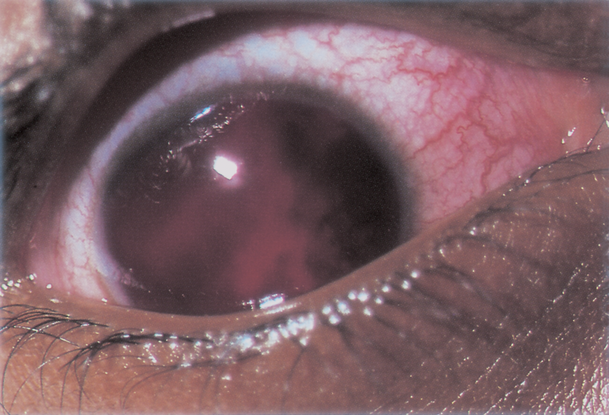
Figure 9. Hyphema. Left: layered hyphema. Right: “Eight-ball” hyphema. (Reproduced, with permission, from Weisenthal RW. External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
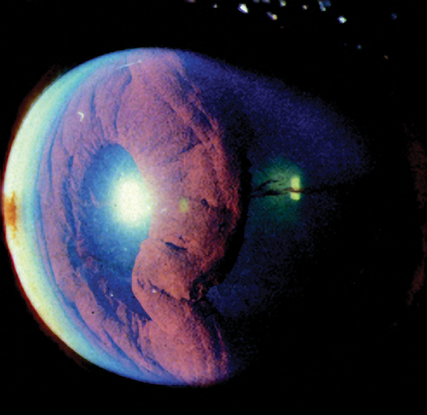

Figure 10. Severe iridodialysis resulting from blunt trauma. Right: posterior view of iridodialysis (arrows). (Left: Reproduced, with permission, from Reidy JJ. External Disease and Cornea . Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2012-2013. Middle-Right: Reproduced, with permission, from Rosa RH, Ophthalmic Pathology and Intraocular Tumors. Basic and Clinical Science Course, Section 4, American Academy of Ophthalmology, 2013–2014).
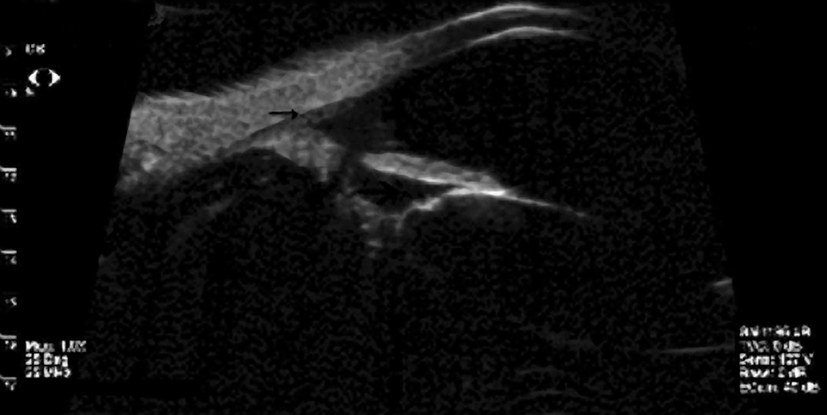
Figure 11. Cyclodialysis seen on ultrasound biomicroscopy. (Reproduced, with permission, from Weisenthal RW.
External Disease and Cornea. Basic and Clinical Science Course, Section 8, American Academy of Ophthalmology, 2013–2014.)
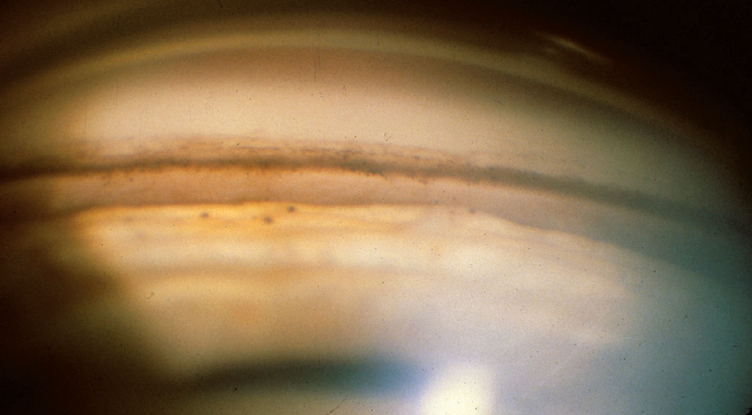
Figure 12. Angle of a 45-year-old man who was hit with a BB as a child. He later developed unilateral glaucoma from angle recession. Note the very deep anterior chamber and the large amount of ciliary body face visible below the scleral spur. The ciliary body band is a light color because it consists of only a thin layer of tissue over sclera. The tiny black balls on the iris are residuals from old hemorrhage. (© 2013 American Academy of Ophthalmology.)
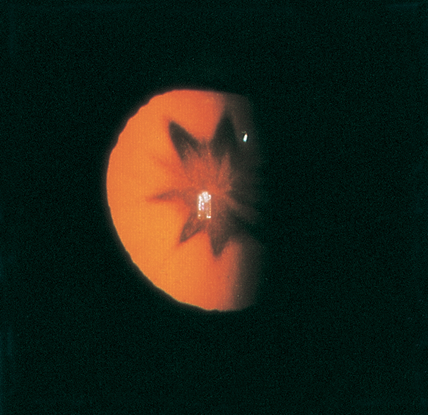
Figure 13. Stellate lens opacity following contusion. (© 2013 American Academy of Ophthalmology.)
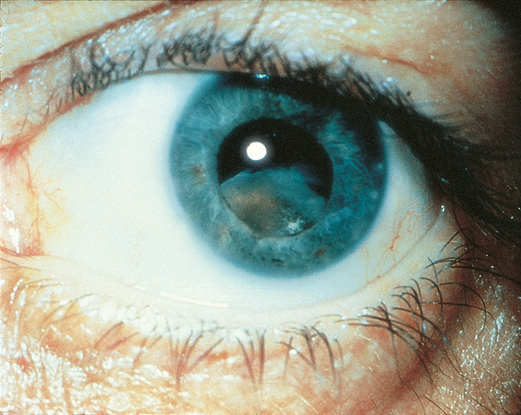
Figure 14. Dislocation of lens following blunt trauma. (© 2013 American Academy of Ophthalmology.)
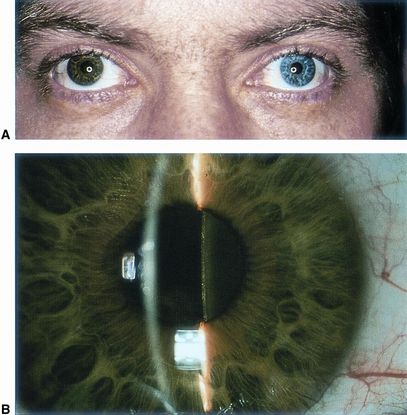
Figure 15. Siderosis bulbi seen in eye following metallic foreign body exposure in trauma. A. Heterochromia iridis caused by Siderosis bulbi. B. Discoloration of lens capsule and cortex. (© 2013 American Academy of Ophthalmology.)
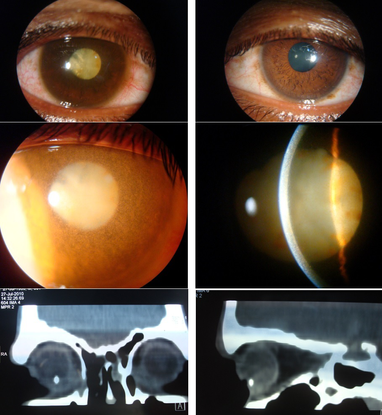
Figure 16. Iron IOFB. A 30-year-old male presented with complaints of diminution of vision in right eye over past few months. He reported a history of injury to that eye by a flying object more than six months previously. His vision was perception of light with inaccurate projection in the right eye and 20/20 in left eye. Ocular examination was significant for iris heterochromia (top) and right exotropia. The right eye showed mild haziness and granular appearance of corneal stroma with endothelial pigment deposition, fixed and non-reactive pupil, total cataract with brown pigment deposits on the anterior capsule (middle) and increased pigmentation of the trabecular meshwork on the gonioscopy. A B-scan revealed a cataract with mobile vitreous opacities and an attached retina. Computerized tomography showed a metallic foreign body (4.7x4.0x2.7mm in size) embedded in the sclera inferiorly in the ciliary body region (bottom). Siderosis bulbi occurs due to toxic effect of ionized iron released from retained metallic foreign body that results in degeneration of the ocular tissues. (© 2013 American Academy of Ophthalmology. Courtesy of Pawan Prasher, MD.)

Figure 17. Commotio retinae (arrows) and vitreous hemorrhage after blunt trauma. (© 2013 American Academy of Ophthalmology.)

Figure 18. Sclopetaria after bullet trauma.(© 2013 American Academy of Ophthalmology.)
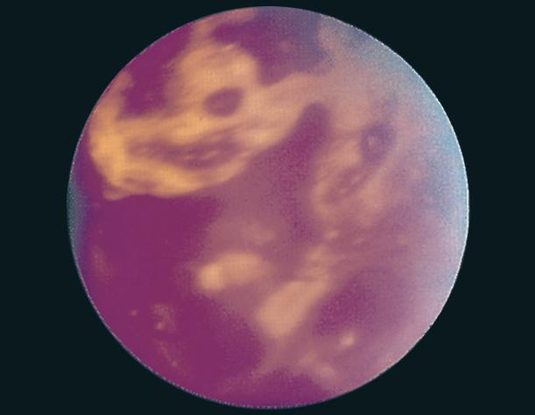
Figure 19. Extensive retinal hemorrhages, left eye, in a 2-month-old infant thought to have been violently shaken. (© 2013 American Academy of Ophthalmology.)
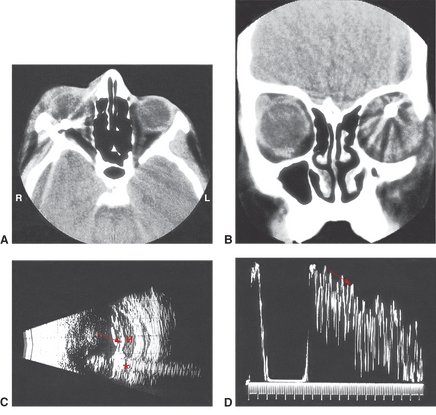
Figure 20. BB pellet penetrating globe rupture with retained foreign body as demonstrated on (A) axial CT, (B) coronal CT, (C) B-scan echography, and (D) A-scan. The subretinal hemorrhage is best seen on B scan with a classic “trail of echoes” reverberation of hyperechogenicity seen anterior and posterior to the BB bullet. Asterisk = foreign body; arrows = “trail of echos.” (© 2013 American Academy of Ophthalmology.)
Case Study
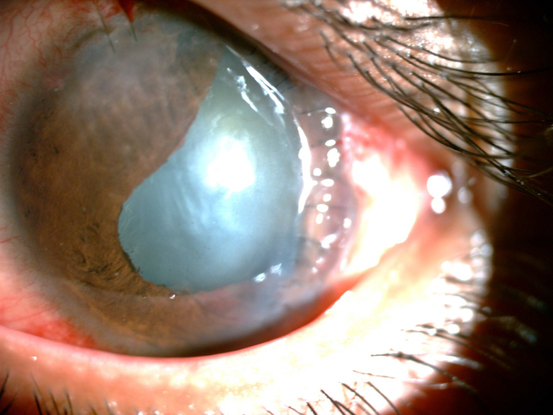
Figure 21. Corectopia following trauma.
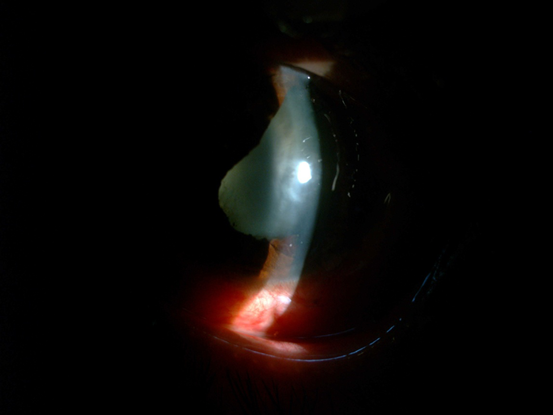
Figure 22. Seidel testing demonstrated leaking of aqueous fluid over a corneal laceration. Measurement of intraocular pressure was deferred and a hard shield was placed over the eye.
File Name: trau22
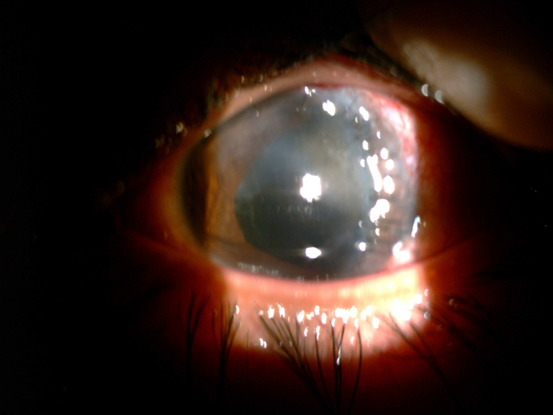
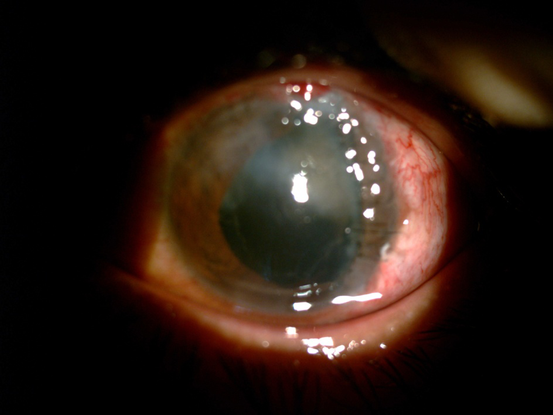
Figure 23. Left: superior corneal haze postoperatively. Right: status after phacoemulsification and IOL implantation
REFERENCES
American Academy of Ophthalmology. International Ophthalmology. Basic and Clinical Science Course, Section 13, 2005–2006. San Francisco: American Academy of Ophthalmology; 2005:121–134.
Friedberg M, Rapuano C. Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. 5th ed. New York: Lippincott, Williams and Wilkins; 2008.
Pierre Filho PTP, Gomes PRP, Pierre ÉTL, et al. Profile of ocular emergencies in a tertiary hospital from Northeast of Brazil. Revista Brasileira de Oftalmologia. 2010;69.
Silva JC, Bateman JB, Contreras, F. Eye disease and care in Latin America and the Caribbean. Surv Ophthalmol. 2002;47:267–274.
CONTRIBUTORS
Executive Editor: R. V. Paul Chan, MD, FACS, New York-Presbyterian Hospital, Weill Cornell Medical College, New York, New York
Section Editors: <<in CMS: insert section ed info specific to that template>>
Asia-Pacific:
Timothy Y. Lai, MBBS, MD, MMedSc, FRCS, FRCOphth, FHKAM, Department of Ophthalmology & Visual Sciences, The Chinese University of Hong Kong
Manish Nagpal, MBBS, MS, FRCS, Retina Foundation & Eye Research Center, Ahmedabad, India
Assistant Editors:
Swetangi D. Bhaleeya, MD, Weill Cornell Medical College; New York, New York
Kristin Chapman, MD, Weill Cornell Medical College, New York, New York
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
Michael Klufas, MD, Weill Cornell Medical College, New York, New York
Samir Patel, medical student, Weill Cornell Medical College; New York, New York
Region Contributor:
Kristin Chapman, MD, Weill Cornell Medical College, New York, New York
Copyright © 2013 American Academy of Ophthalmology®. All Rights Reserved.