EPIDEMIOLOGY
Global Information
- Ophthalmic findings of vitamin A deficiency are a sign of systemic Vitamin A deficiency, which is associated with significantly increased risk of mortality and blindness, especially among pre-school-age children.
- Vitamin A deficiency is associated with malnutrition, infectious and diarrheal disease, and respiratory illness.
- Every year 5 to 10 million children develop xerophthalmia (abnormal dryness of the eyes), and 500,000 of those cases will result in vision loss.
- More than 100 million children have subclinical vitamin A deficiency and over 1 million die each year from the disease.
Regional Information (Asia)
|
Table 1. Prevalence of Vitamin A Deficiency in Asia
|
|
Country
|
Population at Risk
|
|
Bangladesh
|
14,725,000
|
|
Bhutan
|
208,000
|
|
India
|
86,920,000
|
|
Indonesia
|
14,119,000
|
|
Myanmar
|
3,905,000
|
|
Nepal
|
2,582,000
|
|
Thailand
|
1,394,000
|
|
Sri Lanka
|
717,000
|
DIFFERENTIAL DIAGNOSIS
PATHOPHYSIOLOGY/DEFINITION
- Vitamin A deficiency alters the immune system by causing metaplasia and keratinization of mucus-secreting epithelium.
- Additionally, antibody response is deficient.
Stages of Xerophthalmia
- Stage 1, night blindness (XN), limitation in scotopic retinal sensitivity
- Retina unable to regenerate rhodopsin
- Stage 2, conjunctival signs (X1A,B)
- Bitôt spot (Figure 6)
- Squamous metaplasia
- Keratinization of mucus-secreting epithelium
- Stage 3, corneal signs
- Superficial punctate keratopathy (X2)
- Corneal ulcers (X3A)
- Keratomalacia greater than one-third of cornea (X3B)
- Stage 4, corneal scars (XS) (Figure 7)
- Xerophthalmic fundus (XF)
- Immunocompromise
- Deficient t-cell-dependent and independent type 2 antibody response
- Deficient cytotoxic response
- Blastogenic transformation of lymphocytes
Risk Factors for Vitamin A Deficiency
- Malnutrition
- Low socioeconomic status
- Living in an endemic area
- Respiratory or diarrheal illness
SIGNS/SYMPTOMS
- Night blindness—children may behave differently at dusk or in darker locations
- Conjunctivitis
- Corneal xerosis
- Bitôt spot (Figure 6)
- Corneal scar (Figure 7)
- Corneal ulcer/necrosis
MANAGEMENT
Prevention
- Empiric vitamin A supplementation programs have helped reduce the incidence of vitamin A deficiency in endemic areas.
- Additional prevention measures:
- Fortification of foodstuffs with Vitamin A
- Increasing dietary intake of Vitamin A
Treatment
- Treatment consists of immediate, high-dose vitamin A supplementation.
- Treatment is inexpensive—a typical regimen of 3 pills of high-dose vitamin A costs less than $0.10.
- Child <12 months:
- 100,000 IU vitamin A now, tomorrow, and 2–4 weeks
- Child > 12 months:
- 200,000 IU now, tomorrow, and 2–4 weeks
- Women of childbearing age; night blindness or Bitôt spots:
- 10,000 IU daily x 2 weeks OR
- 25,000 IU weekly for 4 weeks
- Corneal lesions:
- 200,000 IU now, tomorrow, and 2–4 weeks
CASE STUDY
- A 6-month-old child presents for ocular examination. She has no past medical or surgical history and was born full term, albeit to a mother with poor prenatal care in South Sudan.
- The child’s recent medical history is significant for several episodes of diarrhea and low weight for gestational age.
- Further questioning of the mother reveals she has difficulty seeing at night since her last pregnancy and admits that it is difficult to provide adequate nutrition for herself or the child.
- Over the past several weeks, has noticed her child has had increasing eye redness and tearing in both eyes.
- Slit lamp examination of the child reveals keratinization of the conjunctival of both eyes (Bitôt spots) and an area of corneal thinning without ulceration, epithelial defect or infectious infiltrate in the left eye.
- Fundus examination of the child is within normal limits.
- Examination of the mother also reveals keratinization of the conjunctiva in both eyes and fundus examination significant for yellow-white spots in the peripheral retina.
- Confrontational visual field testing for the mother shows constriction of the visual field of both eyes.
Differential Diagnosis
- Vitamin A deficiency due to malnutrition, vitamin A deficiency due to lipid malabsorption (cystic fibrosis, bowel resection)
Diagnosis
- Child: Conjunctival xerosis with corneal keratomalacia
- Mother: Conjunctival xerosis with nyctalopia and xerophthalmic fundus
Treatment
- Both the mother and child show evidence of systemic vitamin A deficiency with ocular involvement. This is a high-risk condition associated with a high mortality rate of up to 50% or more.
- Both require oral or parenteral vitamin A supplementationL
- The mother with night blindness should receive vitamin A 10,000 IU daily by mouth x 2 weeks.
- The child should receive vitamin A 100,000 IU by mouth now, tomorrow and in 2-4 weeks) as well as broad vitamin and protein-calorie supplements.
- For the child’s keratomalacia, aggressive corneal lubrication with artificial tears and ointment is needed to prevent secondary infection and corneal melting/perforation.
- Close follow-up is necessary to ensure no progression of corneal thinning to perforation and improvement of clinical exam.
REFERENCES
International Ophthalmology. Basic and Clinical Science Course, Section 13. San Francisco: American Academy of Ophthalmology; 2004–2005.
Lens and Cataract. Basic and Clinical Science Course. Section 11, San Francisco: American Academy of Ophthalmology; 2012–2013.
World Health Organization, United Nations Childrens Fund. Global prevalence of vitamin A deficiency. Micronutrient Deficiency Information System Working Paper No. 2. 1995.
IMAGE LIBRARY
Differential Diagnosis
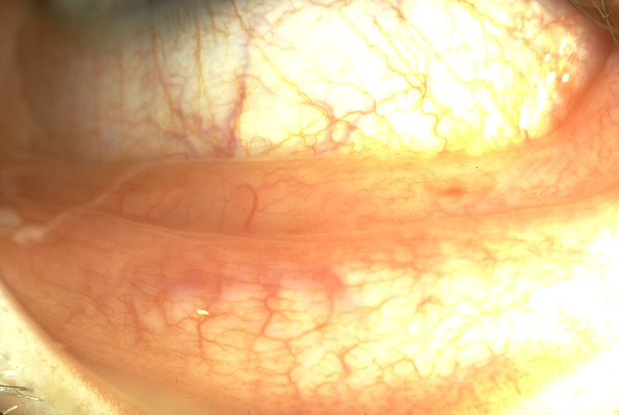
Figure 1. Allergic (hay fever) conjunctivitis. (© 2013 American Academy of Ophthalmology.)
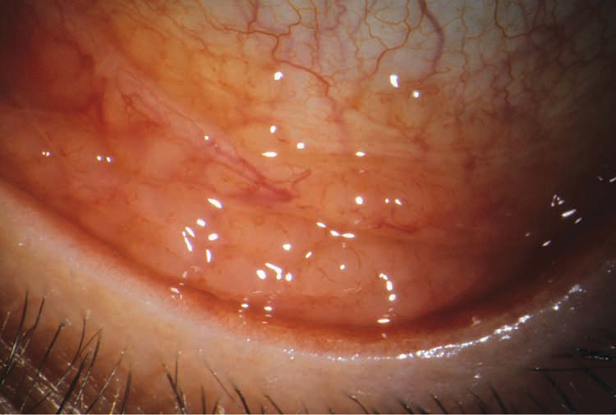
Figure 2. Hemorrhagic viral conjunctivitis. (Reproduced with permission from Rosa RH Jr. Ophthalmic Pathology and Intraocular Tumors. Basic and Clinical Science Course, Section 4, San Francisco American Academy of Ophthalmology; 2013-2014. Courtesy of Anthony J. Lubniewski, MD.)
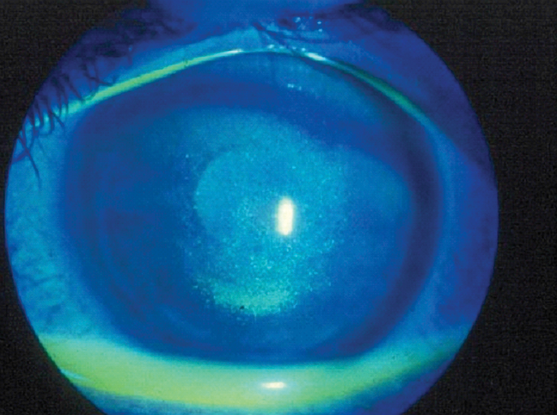
Figure 3. Dry eye syndrome with punctate keratitis and irregular ocular surface. (© 2013 American Academy of Ophthalmology.)
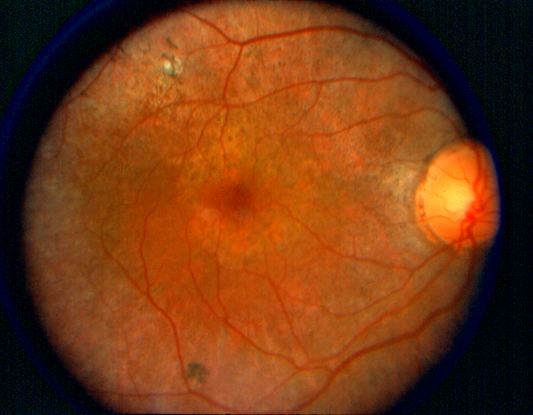
Figure 4. Retinitis pigmentosa. (© 2013 American Academy of Ophthalmology.)
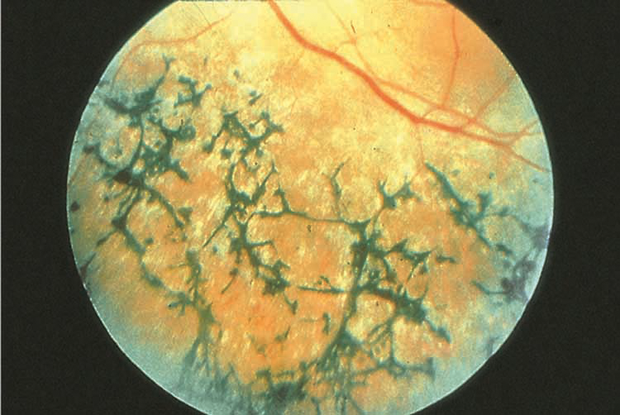
Figure 5. Chorioretinal dystrophy. (© 2013 American Academy of Ophthalmology.)
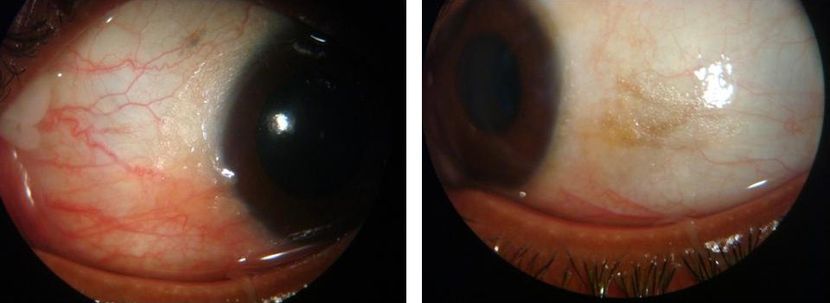
Figure 6. A 30-year-old female presented with complaints of diminution of vision at night, along with dryness and irritation of both eyes for the past few weeks. She had undergone a laparoscopic cholecystectomy 9 months before and had a complicated, postoperative period on account of a common bile duct injury. It required two more surgical procedures and development of liver abscess. Ocular examination at presentation was significant for decreased tear lake, xerosis of the conjunctiva, and silvery-grey, foam- like deposits (Bitôt spots) on the bulbar conjunctiva near the temporal limbus in both eyes. The patient was treated with oral vitamin A 50,000 IU per day and topical lubricants. There was complete resolution of Bitôt spots and marked improvement in night vision within 4 weeks. (© 2013 American Academy of Ophthalmology.Courtesy of Pawan Prasher, MD.)
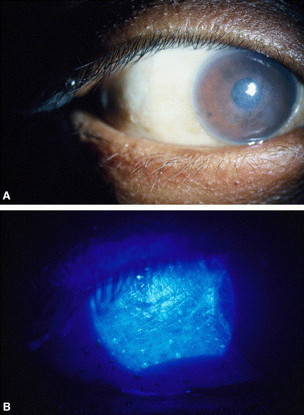
Figure 7. Hypervitaminosis. A. Slit-lamp photograph demonstrating conjunctival xerosis, diffuse punctate keratitis, and corneal scarring from vitamin A deficiency. B. High-magnification view showing xerophthalmia with pooling of fluorescein dye over the completely keratinized conjunctival surface. (Reproduced, with permission, from Lee WB, et al. Ocular complications of hypovitaminosis A after bariatric surgery. Ophthalmology. 2005;112:1031–1034.)
CONTRIBUTORS
Executive Editor: R. V. Paul Chan, MD, FACS, New York-Presbyterian Hospital, Weill Cornell Medical College, New York, New York
Section Editors:
Asia-Pacific:
Timothy Y. Lai, MBBS, MD, MMedSc, FRCS, FRCOphth, FHKAM, Department of Ophthalmology & Visual Sciences, The Chinese University of Hong Kong
Manish Nagpal, MBBS, MS, FRCS, Retina Foundation & Eye Research Center, Ahmedabad, India
Assistant Editors:
Swetangi D. Bhaleeya, MD, Weill Cornell Medical College; New York, New York
Kristin Chapman, MD, Weill Cornell Medical College, New York, New York
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
Michael Klufas, MD, Weill Cornell Medical College, New York, New York
Samir Patel, medical student, Weill Cornell Medical College; New York, New York
Region Contributor:
Peter Coombs, MD, Weill Cornell Medical College; New York, New York
Copyright © 2013 American Academy of Ophthalmology®. All Rights Reserved.