The middle of the eye is filled with a substance called vitreous. In the healthy, young eye, this clear, gel-like substance is firmly attached to the retina and the macula by millions of microscopic fibers. As the eye ages, or as a result of eye disease, the vitreous shrinks and pulls away from the retina. The vitreous, over time, separates completely from the retina. This is called a posterior vitreous detachment (PVD) and is usually a normal part of aging. It happens to most people by age 70.
In some people with PVD, the vitreous doesn’t detach completely. Part of the vitreous remains stuck to the macula, at the center of the retina. The vitreous pulls and tugs on the macula, causing vitreomacular traction (VMT). This can damage the macula and cause vision loss if left untreated.
What Causes Vitreomacular Traction?
VMT is usually caused by part of the vitreous remaining stuck to the macula during a posterior vitreous detachment.
People with certain eye diseases may be at a higher risk for VMT, including those with:
Also, taking pilocarpine to treat age-related blurry near vision (presbyopia) can increase your risk of VMT.
What Are Symptoms of Vitreomacular Traction?
The most common symptoms of vitreomacular traction (VMT) include:
These symptoms can also be a sign of another eye disease. This is why it’s important to see an ophthalmologist for an evaluation when you first notice any of these symptoms.
How Is Vitreomacular Traction Diagnosed?
To diagnose VMT, your ophthalmologist needs to look inside your eye. To do this, they may use one or more of these tests:
Optical Coherence Tomography (OCT). OCT is the most common test ophthalmologists perform to diagnose VMT. The OCT is an imaging test that uses light waves to take pictures of each of the retina’s layers. It can help show how damaged the macula may be.
Fluorescein angiography. This imaging test uses a special camera to take photographs of the retina. A small amount of yellow dye (fluorescein) is injected into a vein in your arm. The dye helps your ophthalmologist see how well blood is circulating inside the retina. It also helps find swelling of the macula, which is common in VMT.
These tests help find out if you have VMT. They also can tell your doctor what treatment may be needed.
Treatment
After a diagnosis of vitreomacular traction (VMT), there are usually three treatment options:
Observation or a “wait-and-see” approach. If your VMT is mild and not affecting your vision, treatment might not be needed. Because some cases of VMT will resolve on their own, you and your ophthalmologist may decide to observe (watch) the condition with follow-up visits. You also will be asked to monitor your vision at home each day with an Amsler grid. Your ophthalmologist will review proper use of the Amsler grid.
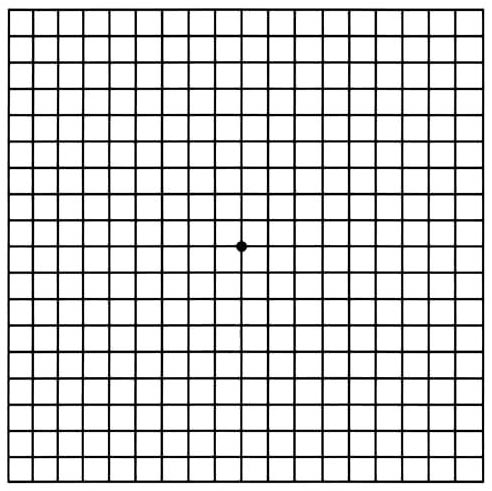
Amsler Grid
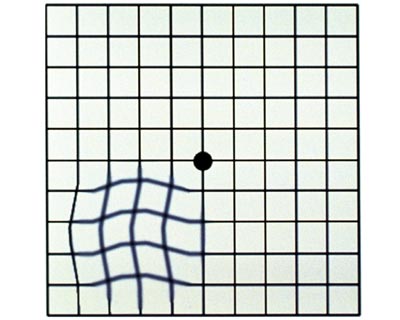
For someone with VMT, an Amsler grid may appear to have wavy lines or blank spots.
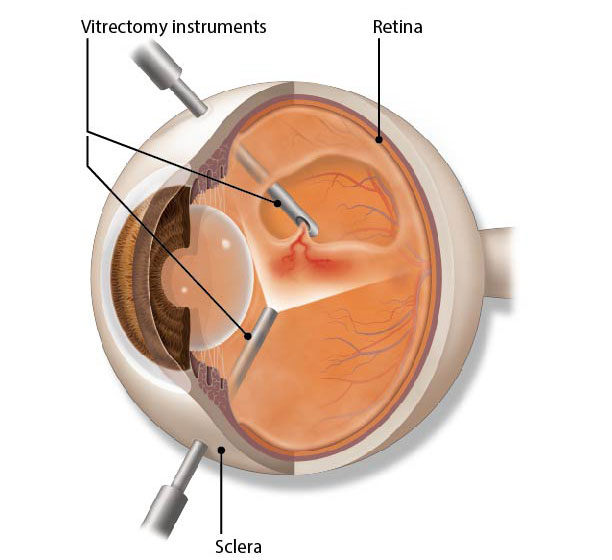
Surgery. Severe cases of VMT can lead to vision-threatening retinal conditions, such as:
In these cases, a procedure called a vitrectomy may be recommended to restore the macula to its normal (lying flat) shape. The surgeon uses tiny instruments to remove the vitreous from the eye and replaces it with a saline fluid. Any scar tissue on the macula is also peeled with special instruments under a microscope. This relieves the traction that is damaging the macula.
Medication. Some people with serious cases of VMT might not be good candidates for vitrectomy surgery. A medication called ocriplasmin is a treatment option for these patients. The drug is given by intravitreal injections (injection into the center of the eye) and works by dissolving the tiny protein fibers that connect the vitreous with the macula. In addition, your ophthalmologist may inject a bubble of gas and have you perform special head positioning to relieve the traction.