Glaucoma is a leading cause of blindness for people over 60 years old. But blindness from glaucoma can often be prevented with early treatment.
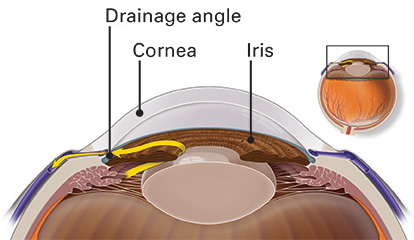
In a healthy eye, fluid leaves the eye through the drainage angle, keeping pressure stable.
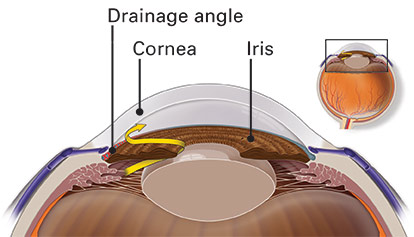
With angle-closure glaucoma, the drainage angle becomes blocked by the iris.
What’s the difference between angle-closure glaucoma and chronic angle-closure glaucoma?
Angle-closure glaucoma
Angle-closure glaucoma (also called closed-angle glaucoma or narrow-angle glaucoma) is a type of glaucoma that happens when someone’s iris blocks the drainage angle in their eye. You can think of it like a piece of paper sliding over a sink drain. When the drainage angle gets completely blocked, eye pressure begins to rise. If this happens suddenly, it is called an acute attack.
Acute angle closure glaucoma is a true eye emergency, and you should call your ophthalmologist right away or you may lose vision permanently.
Here are the symptoms of an acute angle-closure glaucoma attack:
• your vision is suddenly blurry
• you have severe eye pain
• you have a headache
• you feel sick to your stomach (nausea)
• you throw up (vomit)
• you see rainbow-colored rings or halos around lights
Chronic angle-closure glaucoma
Many people with angle-closure glaucoma develop it slowly. This is called chronic angle-closure glaucoma. There are no symptoms at first, so they don’t know they have it until the damage is severe or unless they have an attack of acute angle closure. One out of three people (30 percent) with chronic angle-closure will have a sudden blockage, causing an attack.
Causes
Doctors do not know for sure what causes chronic angle-closure glaucoma. They think there may be many causes, including:
- a lens that is too large (keeping fluid from flowing normally through the pupil).
- an iris that is thicker than normal
- an iris with a roll on the side that blocks fluid (called "plateau iris")
One or more of these factors can cause a gradual closing of the drainage angle, leading to a rise in eye pressure.
Who is at risk for chronic angle-closure glaucoma?
Some people have a higher than normal risk of getting angle closure. This includes people who:
- are over age 50
- have family members with angle-closure glaucoma
- are of Asian or Inuit heritage
- are female
- are farsighted
- have an unusually small eye or a large lens inside the eye
Talk with an ophthalmologist about your risk for getting glaucoma. People with more than one of these risk factors have an even higher risk of angle-closure glaucoma.
How is chronic angle-closure glaucoma diagnosed?
The only sure way to diagnose chronic angle-closure glaucoma is with a complete eye exam. A glaucoma screening that only checks eye pressure is not enough to find chronic angle-closure glaucoma.
During a glaucoma evaluation, your ophthalmologist will:
How is chronic angle-closure glaucoma treated?
Glaucoma damage is permanent—it cannot be reversed. But medicine and surgery help to stop further damage. Treatment of chronic angle-closure almost always requires laser or surgery to reopen the blocked drainage angle. In most people, some eye drop medicine is also needed to help control the eye pressure.
Medication
Used every day, eye drop medicine helps lower eye pressure. Some eye drops do this by reducing the amount of aqueous fluid the eye makes. Others reduce pressure by helping fluid flow better through the drainage angle. Glaucoma medications can help you keep your vision, but they may also cause side effects. They can also interact with other medications. It is important to give a list of every medicine you take regularly to all of your doctors. Be sure to talk with your ophthalmologist if you think you may have side effects from glaucoma medicine.
Never change or stop taking your glaucoma medications without talking to your ophthalmologist. If you are about to run out of your medication, ask your ophthalmologist if you should have your prescription refilled.
Laser surgery
There are two main types of laser surgery to treat chronic angle-closure glaucoma. They both move the iris away from the drainage angle and help fluid drain from the eye. These procedures are usually done in the ophthalmologist’s office or outpatient surgery center.
- Iridotomy. The ophthalmologist uses a laser to create a tiny hole in the iris. This hole helps fluid flow to the drainage angle.
- Iridoplasty. The ophthalmologist uses a laser to shrink the iris back away from the drainage angle.
Operating room surgery
Some glaucoma surgery is done in an operating room. These procedures either reopen the blocked drainage angle or create a new drainage channel for the aqueous humor to leave the eye.
- Cataract surgery. In some people, their lens is large enough to push the iris up over the drainage angle, causing angle-closure glaucoma. If the lens is also cloudy, it is called a cataract. Your eye surgeon can remove the lens and replace it with a thin, clear implant lens. This can reopen the drainage angle and help lower your eye pressure.
- Synechialysis. If the iris has been blocking the drainage angle for a long time, the iris may permanently stick to the angle. This connection is called a synechia. It blocks the flow of fluid out of the eye. Your eye surgeon can use tiny instruments inside the eye to break these connections and pull the iris away from the drainage angle. This may restore the flow of aqueous fluid out of the eye.
- Trabeculectomy. This is where your eye surgeon creates a tiny flap in the sclera (white of your eye). He or she will also create a bubble (like a pocket) in the conjunctiva (the thin membrane that covers the inside of your eyelids and white part of your eye) called a filtration bleb. It is usually hidden under the upper eyelid and cannot be seen. Fluid will be able to drain out of the eye through the flap and into the bleb, lowering eye pressure. In the bleb, the fluid is absorbed by tissue around your eye.
- Glaucoma drainage devices. Your ophthalmologist may implant a tiny drainage tube in your eye. It sends the fluid to a collection area (called a reservoir). Your eye surgeon creates this reservoir beneath the conjunctiva, lowering eye pressure. The fluid is then absorbed into nearby blood vessels.
Glaucoma is a silent thief of sight
Chronic angle-closure glaucoma usually has no symptoms in its early stages. In fact, half the people with glaucoma do not know they have it! Having regular eye exams can help your ophthalmologist find this disease before you lose vision. Your ophthalmologist can tell you how often you should be examined.
Your role in chronic angle-closure glaucoma treatment
Treating glaucoma successfully is a team effort between you and your doctor. Your ophthalmologist will prescribe your glaucoma treatment. It is up to you to follow your doctor’s instructions. You can expect to visit your ophthalmologist about every three to six months. However, this can vary depending on your treatment needs. If you have any questions about your eyes or your treatment, talk to your ophthalmologist.