Download PDF
The pros and cons of a new approach.
Even as ophthalmologists continue to debate the clinical merits of the femtosecond laser in cataract surgery, early adopters of the technology have had to devise systems for incorporating a single laser into their cataract practices while still maintaining efficient workflow for several operating rooms and multiple surgeons.
One of these innovations—still rare in the United States—takes the quest for efficiency and quality of care to lengths that, if widely adopted, could fundamentally alter the manner in which femtosecond cataract surgery is performed in the developed world.
The simple but, arguably, revolutionary change is this: Call in a second surgeon to perform the femtosecond laser portions of the surgery.
“It’s obvious that using 2 surgeons per case would increase efficiency and throughput because you could have both the laser and nonlaser parts of the procedure going on essentially simultaneously,” said Steven C. Schallhorn, MD, medical director for Optical Express, a refractive surgery chain based in the United Kingdom. “You would maximally utilize the femtosecond laser. You could probably double the use of the laser on each surgery day.”
Today’s way: 1 case, 1 surgeon. Yet in most U.S. practices, a single surgeon performs both parts of the procedure despite logistical inefficiencies.
Because femtosecond lasers for cataract use are expensive, surgery centers usually have just one of them. But it is inherently inefficient to house the laser within a single operating room, which greatly restricts the number of surgeons who can use it. As a result, it is common for the laser to be located in a nonsterile laser room adjacent to or near 1 or more operating rooms. If everything goes as planned, this enables the surgeon and staff to move efficiently through their laser-assisted cases with minimal downtime.
“The surgeon toggles between the 2 ORs and the laser room, like a triangle,” said refractive cataract surgeon George O. Waring IV, MD, at the Medical University of South Carolina, in Charleston. “After the first patient’s intraocular lens [IOL] is implanted, the surgeon goes back to the laser for the second patient and then into a second OR for that patient, and so on.”
The newer way: 1 case, 2 surgeons. One surgeon well known for embarking on this road less traveled is Eric D. Donnenfeld, MD, who practices at Ophthalmic Consultants of Long Island, in Rockville Centre, N.Y. Greater efficiency and quality of care are the goals, Dr. Donnenfeld said. “It makes no sense to me to have an OR sit empty while the surgeon is doing a laser, when the cost of keeping an OR up and running and fully staffed is so significant,” he said.
“Although I do all my conventional cataract surgery myself, for surgeries that include a femtosecond laser I have another physician who does most of the lasers for me, and then I complete the manual parts of the cataract surgery myself,” he said.
Adoption of the 2-surgeon approach to femtosecond cataract surgery is rare in the United States—for now—Dr. Donnenfeld said. “I don’t think this is being done a lot, but I think it will become a more significant part of the surgical landscape as time goes on,” he predicted.
From the Sidelines, Cautious Curiosity
Dr. Schallhorn called the 2-surgeon system “a very interesting model” that bears watching as it develops further. “At Optical Express, we’ve thought about dividing our femtosecond laser cataract surgery between 2 surgeons, but it’s not something that we’ve done because we’re just now ramping up with the laser for premium IOL and refractive lens exchange [RLE] surgeries,” he said.
Similarly, Dr. Waring said that he has not yet invited a second surgeon to do the laser portion of his surgeries—but he has considered it. “The majority of our surgery is laser assisted, and for now I prefer doing this myself, particularly for complex cases. But we’re using our femtosecond laser so heavily that we have thought about assigning a fellow to run the laser,” Dr. Waring said.
Dawn of the “Laser Specialist”?
Why would a skilled ophthalmic surgeon give up the operating room for a laser procedure room? Dr. Donnenfeld provided this account about the colleague with whom he divides femtosecond cataract cases:
“There is someone in our practice who just likes doing the laser and who doesn’t like the idea of doing a lot of intraocular surgery,” Dr. Donnenfeld said. “This allows him to stay surgically active, and he has developed a special expertise with it.
“He does this for other cataract surgeons as well as for me,” said Dr. Donnenfeld, adding that since his colleague works more with the laser than the other surgeons, has more experience with it, and has made himself very good with the femtosecond laser, he has better laser outcomes than anyone else in the practice. “So this is kind of a win-win for the patients.”
There might be an advantage of having a laser-only surgeon involved in these IOL procedures, Dr. Schallhorn said. “Techniques with the femtosecond laser—docking, adjusting, and patient positioning—are fairly unique, and there’s a learning curve associated with them. Having surgeons who are really expert at doing the femtosecond part of the procedure is a good thing,” he said.
Lessons From LASIK?
In some high-volume refractive surgery practices overseas, ophthalmic laser specialization is a well-established tool for delivering care to large numbers of patients as efficiently as possible.
For instance, the 15 ophthalmologists at Shinagawa LASIK Center in Tokyo see more than 200 patients each day, according to the center’s website.
On several visits to Shinagawa, Dr. Waring recalled, he and his late father, George O. Waring III, MD, observed a remarkably efficient process in which a single LASIK surgery might involve several laser-specific, expert surgeons.
“You might have one doctor who’s assigned to femtosecond lasers and actually running multiple laser models in a few different rooms, while another doctor is running multiple excimer lasers. So a patient would be operated on by multiple surgeons as they were going through the different stages of the surgery,” Dr. Waring said.
Although it would be speculative to postulate a direct relationship between multidoctor LASIK at centers such as Shinagawa and today’s interest in femto-cataract “laser specialists,” the similarities are striking, he said.
|
A Father-Son Cataract “Tag Team”
About a year ago, William B. Trattler, MD, and his father, Henry L. Trattler, MD, who work at a Miami-based group practice, decided that they would do femtosecond laser–assisted cataract surgery together 1 day a week. The rest of the time, each continues to see patients and to perform surgeries solo. The younger Dr. Trattler pronounced this verdict on their dual-doctor, femto-cataract surgery days: “It’s been working out fantastically.” The goals of this “tag team” approach were to provide patients with a very personal experience and to maintain efficiency during the day in the OR.
Efficiency. “When I operate on Thursdays, he does the femtosecond laser portion of the procedures in 1 room, and I work out of 2 operating rooms, going back and forth between the ORs to do the manual portion of the procedures,” the younger Dr. Trattler said. They typically complete 12 to 15 laser-assisted cases on Thursdays and also have time for other surgeries, such as pterygium procedures, conventional cataract cases, and phakic IOLs, he said. “It’s really efficient because we can definitely do more cases in a shorter period of time. And we’re not sacrificing patient care because my father is very experienced with the laser,” the younger Dr. Trattler said.
Patient satisfaction. “An even more important part is optimizing the patient experience,” he said. “My dad has an amazing way with patients, and the time he spends with them translates into a better surgical experience for the patient. Patients tell us that they enjoy the fact that both of us are helping out with the surgery.”
Another Efficiency Idea: Bilateral Same-Day Cataract Surgery
Some researchers have reported that overall systemic efficiency, as well as patient satisfaction, would increase overnight if immediately sequential bilateral cataract surgery were to become the default approach to routine cataract surgery.1
But this idea remains controversial, particularly in the United States, because of persistent concerns about the possibility of subjecting patients to the risk of bilateral endophthalmitis2 and for reimbursement-related reasons. Specifically, Medicare pays surgeons and surgical facilities less for 2 immediately sequential procedures than it does if the same patient undergoes the 2 surgeries on different days.3,4
Although reimbursement may continue to be an issue, published reports and experience in the Kaiser Permanente capitated health system suggest that patient safety may not be an overwhelming obstacle.
Endophthalmitis rates. Advocates of same-day bilateral surgery have raised the topic’s visibility in the last decade by establishing the International Society of Bilateral Cataract Surgeons (ISBCS) and by publishing reports on members’ outcomes. One retrospective analysis of 95,606 same-day surgeries reported an overall rate of postoperative endophthalmitis of 1 in 5,759 eyes. Intracameral antibiotics reduced the rate further, to 1 in 14,352 cases, and no patient had bilateral simultaneous endophthalmitis.5
In Kaiser Permanente’s Northern California region last year, surgeons performed approximately 3,000 bilateral same-day cataract procedures, accounting for about 8% of the total cataract case load, without any cases of unilateral or bilateral endophthalmitis, said Neal H. Shorstein, MD, associate chief of quality care for Kaiser Permanente in Walnut Creek, Calif. This year, the number is expected to exceed 4,000, he said.
Asepsis. Kaiser Permanente surgeons in the Diablo Service Area in Northern California follow strict aseptic protocol for bilateral sequential surgeries, Dr. Shorstein said. “We try to make the 2 events as independent as possible. The patient stays in the operating room after the first surgery is complete, but everything in the room gets changed over,” he said.
“A new tray is brought in, and there are brand-new drapes. The patient is re-prepped with povidone-iodine. Then everybody cleans their hands again and gets new gowns and gloves.”
After the changeover ends, the IOL for the patient’s second eye is brought into the OR, Dr. Shorstein said. “The second lens stays out of the room during the first procedure so that there’s no confusion in lenses. We also bring in separate documentation and paperwork for the second eye at that time.”
For extra protection, the intracameral antibiotic used in the second eye must come from a different lot number than the first, to further reduce the risk that both eyes would be exposed to a contamination or dilutional error, he said.
“There’s still a rare, rare risk of having a systematic failure in cleaning and sterilization, which could cause bilateral endophthalmitis or toxic anterior segment syndrome. But we’ve not had that happen at Kaiser Permanente,” Dr. Shorstein said.
Intracameral antibiotic. The availability of intracameral cefuroxime and other agents for infection prophylaxis at Kaiser Permanente reassures his colleagues who were anxious about the notion of bilateral surgery, Dr. Shorstein said. “It’s definitely helped ease the worries of our surgeons that our infection rate is now so low, in large part because of intracameral antibiotics. Our rate in Kaiser Permanente Northern California is about 1 in 10,000 or so,” he said.
Patient preference. Bilateral surgery also has been a hit with patients, Dr. Shorstein said. “A lot of patients want this. It’s convenient for them, and they’d rather have both eyes healing at the same time, and not have to go through it sequentially.” Patients wear a set of clear, protective goggles (Encore Eyeshield, Dioptics Medical Products) until the next morning when they are no longer needed. Patients report that the goggles enable them to function reasonably well the afternoon and evening after surgery, he said.
This reception among patients echoes the situation in refractive surgery, where same-day bilateral LASIK and phakic IOL implantation became the norm because patients prefer it, said Dr. Schallhorn. “There is a very strong patient preference for having both eyes done on the same day, and for seeing well right away in both eyes,” he said.
The Medicare payment barrier. Unlike in Kaiser Permanente’s capitated environment, where the surgeon fee stays flat, regular Medicare reduces the surgeon’s fee 50% for the second eye in same-day cases. This is a “very significant barrier” to wider adoption of immediately sequential bilateral cataract surgery in the United States, Dr. Schallhorn said. Nevertheless, he predicted that patient demand and the inherent systemic efficiency of this bilateral approach eventually will push it into the mainstream. “I think that as more papers get published, and as safety protocols and reimbursement issues are ironed out, we’ll be heading in that direction,” he said.
___________________________
1 Lansingh VC et al. Clin Experiment Ophthalmol. 2015 May 13. [Epub ahead of print]
2 American Academy of Ophthalmology Cataract and Anterior Segment Panel. Preferred Practice Pattern Guidelines. Cataract in the Adult Eye. 2011. Available at www.aao.org/ppp.
3 Neel ST. JAMA Ophthalmol. 2014;132(11):1359-1362.
4 Neel ST. JAMA Ophthalmol. 2014;132(11):1282-1288.
5 Arshinoff SA, Bastianelli PA. J Cataract Refract Surg. 2011;37(12):2105-2114.
|
Potential Stumbling Blocks
Several factors must be addressed before a 2-surgeon approach is likely to become widely accepted. These range from surgeons’ sense of personal responsibility to patient perceptions and issues of remuneration.
Surgeon reluctance. “I think most people in our profession feel that they want to do the entire case themselves—that taking care of the patient means doing all parts of the cataract surgery,” Dr. Donnenfeld said. “It’s very analogous to 20 years ago when people would state that you can’t do LASIK on a patient if someone else does the refraction.”
This reluctance to divide laser cataract procedures exists despite the fact that ophthalmologists routinely split the surgical cases of patients with dual ocular diagnoses, Dr. Donnenfeld said. He cited the examples of combined vitreoretinal and cataract surgery, and combined cataract and glaucoma surgery.
Fully informing the patient. The patient must be fully informed and should consent to having a second surgeon operate the femtosecond laser, said Richard L. Lindstrom, MD, a refractive and cataract surgeon at Minnesota Eye Consultants, in Bloomington, Minn. “Patients probably would say yes, if you explain [that] the second person’s expertise is based on greater experience,” Dr. Lindstrom said.
In Dr. Donnenfeld’s practice, patients participate in a full informed consent discussion and are told they will have 2 different surgical specialists, he said. Patient satisfaction with the 2-doctor system has been very high, but “of course, if the patient requests that I perform the laser I am happy to oblige,” he added.
Said Dr. Waring: “I think the key would be telling the patient about it beforehand, so they’re expecting to see your associate who specializes in the laser. Then they won’t be surprised and upset.”
Finding the right second surgeon. It is helpful for the surgeon who operates the laser to have a reassuring bedside manner as well as laser expertise because this will boost patients’ overall satisfaction, Dr. Trattler said. “Personality is important because patients are nervous. You need someone who can address those worries and concerns, talk to the patients, and make them feel confident and comfortable.”
Erosion in the doctor-patient relationship. Joshua P. Vrabec, MD, at the University of Michigan Kellogg Eye Center, noted, “When we start introducing new doctors or taking away face time from the patient, there’s a danger that we might be eroding the patient-doctor relationship. This is an important issue, especially when you’re doing something that could potentially harm them. The patient wants to know whom they can trust to be the person to get them through if a problem occurs.” For this reason, he has these key questions about the team approach:
- Offered the choice, will the patient accept a second doctor?
- Will both surgeons meet with the patient preoperatively and postoperatively?
- Which surgeon is really responsible if there’s a complication?
- How will having 2 surgeons affect patient trust?
Harm to the profession itself. Dr. Vrabec said he also worries that overzealous innovations for promoting surgical efficiency might also provoke public enmity against ophthalmologists in general.
“We as individuals need to make sure that we’re doing everything that we can to protect our profession,” he said. “If the balance goes too far toward the way of efficient choices, cost-effective measures, and things that maximize our profit, then our patients may begin to ask if we are still placing them first, which could have untoward consequences for our profession.”
Financial barriers. Another potential obstacle to the success of the 2-surgeon approach—and it’s no small matter—is the issue of payment. In practices where Medicare pays the surgical fee, a second surgeon is a nonissue because Medicare will not cover the cost.
But even in practices where patients pay out-of-pocket for procedures such as femto-cataract and RLEs, there might be financial barriers, Dr. Lindstrom said. Revenue from dual-doctor surgeries will not necessarily be sufficient for Doctor No. 1 to want to share it with Doctor No. 2, he said.
“If you think about it, the surgeon is probably making as much from the femtosecond laser part of the procedure as from the cataract part itself. And I think that is one reason why most surgeons will want to do both parts of their femtosecond laser–assisted cataract procedures themselves,” he said.
Meet the Experts
ERIC D. DONNENFELD, MD Cataract and refractive surgeon practicing at Ophthalmic Consultants of Long Island, in Rockville Centre, N.Y.; clinical professor of ophthalmology at New York University Medical Center; and a trustee of Dartmouth Medical School. Relevant financial disclosures: Abbott Medical Optics: C,L,S; Alcon: C,L,S; Bausch & Lomb Surgical: C,L,S; LenSx: C; TLC Laser Eye Centers: L,O; Wavetec: C.
RICHARD L. LINDSTROM, MD Refractive and cataract surgeon at Minnesota Eye Consultants, in Bloomington, Minn. Relevant financial disclosures: Abbott Medical Optics: C; Alcon: C; Bausch & Lomb Surgical: C,P; Lensar: C,O.
STEVEN C. SCHALLHORN, MD Medical director for the U.K.-based Optical Express chain of refractive surgery centers and a professor of ophthalmology at the University of California, San Francisco. Relevant financial disclosures: Abbott Medical Optics: C; Optical Express: C.
NEAL H. SHORSTEIN, MD Cataract surgeon and associate chief of quality for Kaiser Permanente in Walnut Creek, Calif. Relevant financial disclosure: Kaiser Permanente: S.
WILLIAM B. TRATTLER, MD Refractive, corneal, and cataract surgeon at the Center for Excellence in Eye Care, in Miami; director of the center’s corneal service, and on the voluntary faculty at Florida International University College of Medicine. Relevant financial disclosures: Alcon: C; Abbott Medical Optics: C,L,S; Bausch & Lomb: S; Lensar: C.
JOSHUA P. VRABEC, MD Assistant professor of ophthalmology at the University of Michigan, in Ann Arbor; director of medical student education at Kellogg Eye Center’s Comprehensive Ophthalmology and Cataract Surgery Clinic, where he mentors surgeons on the use of femtosecond laser in cataract surgery. Relevant financial disclosures: None.
GEORGE O. WARING IV, MD Director of refractive surgery and assistant professor of ophthalmology at the Medical University of South Carolina, in Charleston, and adjunct assistant professor of bioengineering at Clemson University, in Clemson, S.C. Relevant financial disclosures: Abbott Medical Optics: C,L; Alcon: C,L; Bausch & Lomb: C.
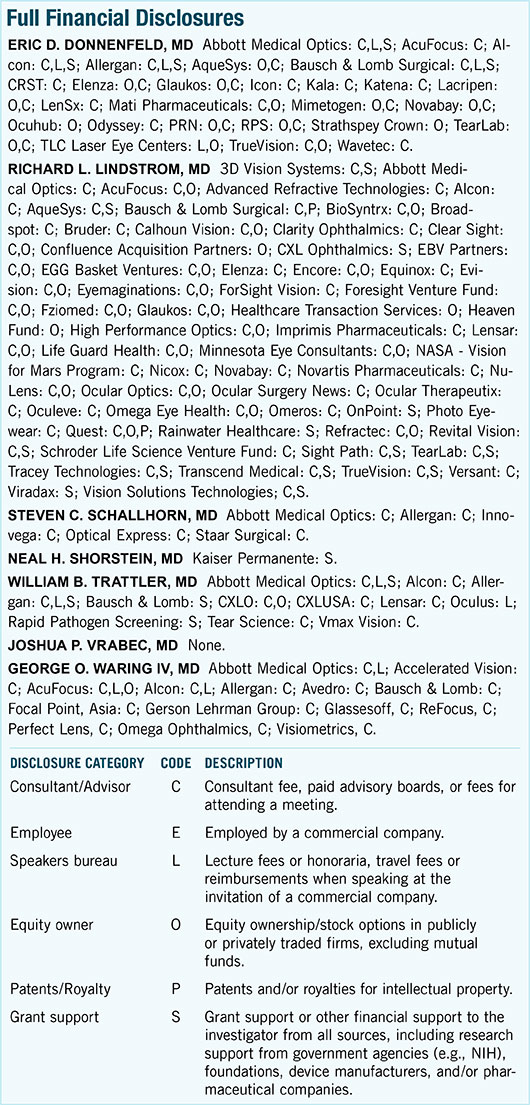
For full disclosures and the disclosure key, see below.
|