By Julia A. Haller, MD, with Diana V. DO, MD, and Peter K. Kaiser, MD
Download PDF
Intravitreal injection of anti–vascular endothelial growth factor (anti-VEGF) is a well-established treatment for wet age-related macular degeneration (AMD), and most practitioners customize the therapy for each patient. Here, in part 1 of a 2-part series, Julia A. Haller, MD, of Wills Eye Hospital, hosts an MD Roundtable with Diana V. Do, MD, of the University of Nebraska, and Peter K. Kaiser, MD, of the Cleveland Clinic. The trio discuss what they consider before starting treatment, how they handle various decisions along the way, and when to start extending the interval between treatments. Part 2 will appear in the November EyeNet. Full audio of their conversation is available at the end of this article.
The Initial Workup
Dr. Haller: What is your initial workup for a new patient whose visual acuity has declined to 20/100 and may have neovascular AMD? How do you choose your initial anti-VEGF agent?
Dr. Do: To diagnose neovascular AMD and rule out masquerading conditions, I usually complement my clinical examination with adjunctive imaging studies, including fluorescein angiography (FA) and optical coherence tomography (OCT) angiography. Both of these imaging modalities are essential for proper diagnosis.
Dr. Kaiser: I agree. If the patient is African American or Asian, I would also add indocyanine green (ICG) angiography at baseline to look for polyps or a branching vascular network due to polypoidal choroidal vasculopathy (PCV). For Caucasian patients, I don’t perform ICG at baseline even though many of them could have PCV. We don’t have enough evidence to perform ICG at baseline for all patients.
In terms of initial management, many comparison studies of bevacizumab and ranibizumab have shown that whether we inject monthly or use a PRN [as-needed] regimen, the efficacy results are relatively similar, but there’s a big difference in cost. We also know that efficacy is similar for monthly ranibizumab and every other month aflibercept based on the VIEW studies.
For my patients with wet AMD, I always start with bevacizumab. You have to mention to the patient that this is an off-label use of the medication, and I talk with patients about the CATT study. At the Cleveland Clinic, we don’t use a commercial compounding pharmacy. All our [intravitreal] bevacizumab is made in our own pharmacy once a week. We send several syringes for microbiologic testing before we release a batch—and at the end of each week, we throw out what’s left over.
Dr. Do: In regard to bevacizumab and off-label use, many retina specialists in the community do not have the benefit of a hospital-based compounding pharmacy; therefore, safety concerns may be greater with bevacizumab. A few years ago, there were several outbreaks of endophthalmitis caused by contaminated bevacizumab, and this led to severe vision loss in eyes that received the tainted bevacizumab. Since then, stricter guidelines are being enforced. If retina specialists are utilizing bevacizumab for the treatment of retinal vascular disorders, I recommend that they select a compounding pharmacy that follows Chapter 797 guidelines of the U.S. Pharmacopeia–National Formulary and that they choose an accredited pharmacy.
Fortunately, all 3 of our anti-VEGF agents (bevacizumab, ranibizumab, and aflibercept) are effective options for the treatment of neovascular AMD. In my clinical practice, if there are no financial barriers, I usually recommend starting with either FDA-approved aflibercept or ranibizumab because both have Level I evidence for efficacy and safety. If finances are a concern for the patient, then I would recommend bevacizumab. Clearly, bevacizumab is the most cost-effective anti-VEGF agent; however, it is essential that ophthalmologists have the freedom of choice regarding anti-VEGF agents because some patients may respond more favorably to a particular VEGF inhibitor.
Setting Expectations
Dr. Haller: As you embark on therapy, how do you set expectations for the patient?
Dr. Do: In general, I utilize an as-needed treatment regimen that I customize for each patient. I counsel patients by referring to the CATT study, and I advise them that, on average, they will need 7 or 8 injections during the first year of treatment. The number of anti-VEGF injections usually decreases in the second year, but it’s still impor-tant to have frequent follow-up visits because neovascular AMD can recur, and we do not want to miss any active choroidal neovascular lesions.
Dr. Kaiser: I explain that this treatment is variable across patients and even between eyes. I don’t try to predict how many injections they will need, but I tell the patient that I’m going to be very aggressive with my treatment because we know that aggressive early treatment leads to better results.
Dr. Haller: The only thing I would add is that I start off by saying that this is a chronic disease, and currently we don’t have a cure for it. So we’re managing the disease rather than curing it.
Dr. Do: I would like to emphasize that it’s important not to undertreat the patient. Over the past year or so, there has been controversy about long-term anti-VEGF treatment and possible adverse events. Some retina specialists are concerned that prolonged intravitreal anti-VEGF treatment can lead to macular atrophy, which would then compromise vision. However, we know from many studies that the more-limiting factor is undertreating choroidal neovascularization [CNV] because that is the leading cause of severe vision loss. I would recommend not worrying about macular atrophy and treating the wet AMD lesions aggressively if one sees signs of leakage.
Establishing a Dosing Regimen
Dr. Haller: You give an injection and the patient comes back in a month. Are you definitely giving another injection?
Dr. Kaiser: I use the treat-and-extend regimen without a loading period. The loading-period idea was based on data from the phase 3 MARINA and ANCHOR trials, in which monthly injections of ranibizumab were evaluated. They showed that the majority of the visual improvement occurred during the first 3 months, with little improvement beyond that. The PIER study tested this idea with 3 monthly injections followed by quarterly ranibizumab dosing. The results of this regimen were not as good as monthly dosing. In the PrONTO study, as-needed dosing was used instead after the 3-injection loading period, and patients did very well; thus, many people use this regimen. I think the idea of a universal loading period is a fallacy because everybody is different. Some patients need a loading period of 4 or 5 monthly injections; for others, you can start extending after the first injection.
I administer bevacizumab initially, then see the patient 1 month later. If OCT still shows leakage, I treat again with bevacizumab and see the patient 4 weeks later. If OCT shows no intraretinal or subretinal fluid, I treat again (the “treat” part of treat and extend) but schedule the follow-up visit for 6 weeks later (the “extend” part of treat and extend). I don’t worry about any fluid underneath the retinal pigment epithelium [RPE] because that may not become dry for a very long time. To make sure that the CNV is dry, a macular cube scan or radial line scan is needed. With an Optovue, Topcon, or Zeiss OCT, the cube is going to give you more information than radial scans would. With a Heidelberg device, radial scans are probably better. But I think the bottom line is to look at many scans to make sure that no fluid is present before extending the interval.
Dr. Haller: I would say that I err on the side of giving another injection a month later because I’m not 100% sure I’ve gotten them as dry as I can.
Dr. Do: In my clinical practice, most patients need many treatments during the first 6 months. I use an as-needed treatment regimen, and often on the second visit they need another treatment. If a follow-up OCT scan shows completely inactive AMD with a dry retina, I will only observe at that visit and have the patient return a month later for further evaluation. I follow guidelines used in the CATT study; patients in the as-needed treatment arm still had monthly follow-up but were treated only if signs of active wet AMD were present.
Switching or Combining Therapies
Dr. Haller: Let’s consider a patient who has been treated a number of times and is not drying out. What (if anything) would make you switch agents, and which agent would you switch to?
Dr. Do: If I had started with bevacizumab for financial reasons and the patient still had persistent, active wet AMD by OCT or FA, I would recommend switching to an on-label anti-VEGF agent. I would probably select aflibercept because there have been some case reports to suggest that in patients who did not have an optimal response to bevacizumab, switching to aflibercept provided additional benefit. However, there are no randomized clinical trials that provide clear data on when we should consider switching agents or which anti-VEGF agent to switch to.
Dr. Haller: Would you order repeat FA if a patient still had fluid seen on OCT after several treatments? How long would you keep treating monthly before you decided to switch?
Dr. Do: For follow-up, we are clearly utilizing OCT more frequently than FA. OCT is extremely useful in monitoring the therapeutic response. If a patient is not having a good response to a particular anti-VEGF agent, there’s still no consensus on the optimal time to switch agents. However, one can’t label patients as suboptimal responders if one has not been monitoring them frequently enough. For example, a 6-week follow-up interval might be too long. It might be more beneficial if the patient is seen every 4 weeks.
If I am confident that the diagnosis is truly neovascular AMD, based on my original FA at baseline, then I won’t necessarily repeat FA. However, if for some reason I think that there may be a confounding factor, such as PCV, I might add ICG to make sure I haven’t missed any polyps. The only reason for identifying PCV would be to consider adding photodynamic therapy (PDT) to the anti-VEGF agent to have a more synergistic effect.
Dr. Kaiser: Based on the VIEW study, we know that after 3 injections of aflibercept, approximately 20% of patients will have persistent leakage. With 3 injections of ranibizumab, about 30% of patients will have persistent leakage. Therefore, you’d expect that roughly 80% of your aflibercept patients and 70% of your ranibizumab patients should be pretty dry after 3 injections. For those who are not, you want to consider a switch.
If the patient is receiving bevacizumab or ranibizumab, I would switch to aflibercept. From aflibercept, what do you switch to? A recent study reported that patients with persistent leakage after 3 injections did better over time on aflibercept than ranibizumab.1
There have been many reports about switching to aflibercept. Ranibizumaband bevacizumab existed before aflibercept. When aflibercept became available, everyone switched their patients with inadequate response to aflibercept. Although there have been several case series about switching in the opposite direction, it appears that a beneficial effect is less common when switching from aflibercept to one of the other drugs. So for a patient already on aflibercept, I would maintain monthly aflibercept until dry, when I would extend.
Dr. Haller: Would you repeat FA at any point? You [Dr. Kaiser] alluded to getting ICGs at baseline for African American and Asian patients. If you had a Caucasian patient who was not responding, would you use ICG?
Dr. Kaiser: I may, especially if they have a type 1 lesion [sub-RPE vessel proliferation]. A type 2 lesion [vessels above the RPE] is almost never going to be PCV. However, I would still switch the anti-VEGF therapy at this point and would consider adding PDT if PCV is present because PCV may not respond to anti-VEGF treatment alone.
There are 2 ongoing studies in Asia addressing the addition of PDT to ranibizumab or aflibercept in patients with PCV. Currently, we don’t know if adding PDT is needed at this stage, but many of us do add it, especially in Asia.
Dr. Haller: When you’re adding PDT, are you using a full-dose regimen?
Dr. Kaiser: Yes. I was the study chair of the Novartis SUMMIT trials, where we looked at combination ranibizumab and PDT versus ranibizumab alone. In the MONT BLANC study, we also evaluated reduced-fluence PDT, and we didn’t see much of a difference in safety or efficacy between reduced- and standard-fluence PDT. According to the Asian literature on PCV, it seems that standard fluence is the way to go.
Dr. Do: Usually, if I have to incorporate PDT, I use standard fluence for all conditions.
Dr. Haller: For a lesion that’s fairly large and not responsive—a lesion that you’re convinced is PCV—would you treat one focal area and then sequentially treat other areas, or would you treat a large area at the outset?
Dr. Do: The PDT laser spot size is based on the greatest linear dimension [GLD] of the entire choroidal neovascular lesion (including the polyps and the branching vascular network). It’s essential to obtain ICG angiography (in cases of polypoidal choroidal vasculopathy) or fluorescein angiography (in cases of neovascular AMD) to determine the GLD if one is considering PDT. In the past, direct thermal laser photocoagulation was also a potential treatment option in select cases where the polyps and branching vascular networks were extrafoveal in location.
More at the Meeting
Interested in AMD? Check out the joint session with the Asia-Pacific Academy of Ophthalmology titled Age-Related Macular Degeneration Across Diverse Populations: Variations in Epidemiology, Imaging and Treatment Strategies (Sym45). Topics will include: OCT-A imaging of AMD, new imaging for PCV, new treatment approaches, and more. When: Sunday, Oct. 16, 2:00-3:30 p.m. Where: Grand Ballroom S100ab. Access: Free.
|
Long-Term Follow-up
Dr. Haller: Let’s consider the patient after 1 year. Would you continue monthly follow-up visits indefinitely?
Dr. Do: In the first year, I try to see them every month. I know that this frequent follow-up schedule may be burdensome, but I emphasize to patients that it is very important to monitor their eye condition in order to prevent vision loss. In the second year, if the eye has responded favorably to anti-VEGF therapy and the OCT does not show any CNV activity, I will customize the follow-up interval. If I feel it is safe, I may extend the follow-up interval, but I counsel the patient that this is a chronic condition, and they will still need frequent visits. In the best scenarios, if the AMD lesion is completely dry, I may use quarterly follow-up.
Dr. Haller: When extending the follow-up interval, would you still give an injection every 3 months if the patient had AMD that was dry?
Dr. Do: If the patient had completely dry and inactive choroidal neovascularization on examination and imaging studies, I would not treat, but I would continue close observation based on the as-needed treatment regimen.
Dr. Kaiser: With the treat-and-extend routine, you’re going to do a lot more treatments in the first year than in the second and subsequent years. We know that patients do well with at least quarterly dosing of aflibercept based on the VIEW study and subsequent extension study. For ranibizumab, we know quarterly dosing does not result in visual gain based on the PIER study.
The big question is if you are using the treat-and-extend dosing, if you are treating the patient every 3 or more months, when can you stop—or can you stop? If I have a patient who has had 3 quarterly visits (or 3 visits at 2-month intervals) in which they didn’t have signs of leakage or progression on OCT and vision was stable, I would try to stop the treatment by switching to PRN therapy. However, I would have the patient return more frequently for follow-up in the short term. Unfortunately, it’s very rare that treatment can be stopped, and that’s why developing a sustained-release anti-VEGF therapy is so important.
___________________________
Listen to the roundtable below:
___________________________
1 Jaffe GJ et al. Ophthalmology. 2016;123(9):1856-1864.
___________________________
Dr. Do is professor of ophthalmology and vice chair for education at the University of Nebraska Medical Center in Omaha. Relevant financial disclosures: Allergan: C,S; Bayer: C,S; Genentech: C,S; Regeneron: C,S.
Dr. Haller is Ophthalmologist-in-Chief at Wills Eye Hospital in Philadelphia. Relevant financial disclosures: Celgene: O; Janssen: C; KalVista: C; Merck: C; ThromboGenics: S.
Dr. Kaiser is the Chaney Family Endowed Chair for Ophthalmology Research and professor of ophthalmology at the Cleveland Clinic Lerner College of Medicine in Cleveland. Relevant financial disclosures: Alcon: C; Allergan: C; Bayer: C; Kanghong: C; Novartis: C; Ohr: C; Ophthotech: C; Regeneron: C; SKS Ocular: C.
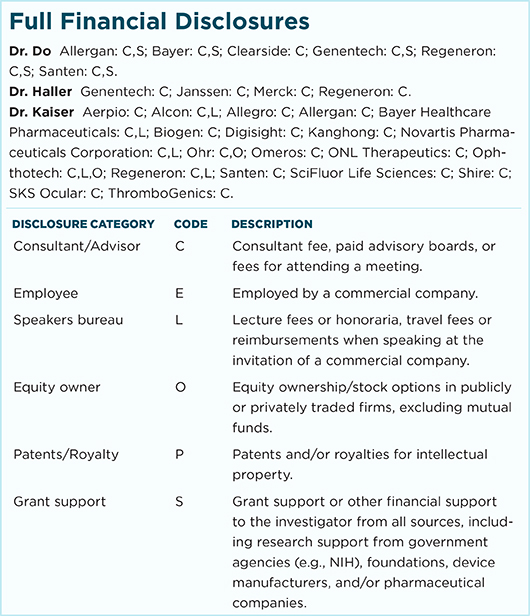
For full disclosures and the disclosure key, see below.