Download PDF
In the middle of a hot summer in Galveston, Texas, Ellie Roberts,* a 62-year-old woman, began to develop fever, sore throat, and malaise. She presented to an urgent care physician, who presumed that she had cat-scratch disease because she was caring for several small kittens at home. However, despite six days of treatment with azithromycin, her fever still hadn’t subsided, and she began to develop floaters in her left eye. She did not have headache or eye pain associated with her floaters. Mrs. Roberts became very concerned because she had read online that floaters can be a symptom of a sight-threatening retinal detachment. She urged her primary care physician to give her a referral to an eye doctor, and she subsequently presented to the department of ophthalmology at our institution.
We Get a Look
Presentation. Mrs. Roberts was visibly ill in the waiting room. By the time she came to our clinic, she had experienced fever (100-102 degrees F) and malaise for 23 days, and her floaters had been getting worse. She also reported night sweats, a 10-pound weight loss over one month, and blurry vision.
The remainder of her review of systems was unremarkable. She had no significant past medical history and no ocular history except for refractive error. She had not been taking any medications prior to her current illness.
As previously noted, Mrs. Roberts said that she loved to care for her kittens and an adult cat at home in her free time. She hadn’t been able to travel lately, since she had been taking care of her ailing husband. She also mentioned that one of her neighbors had been hospitalized recently for a fever of unknown origin.
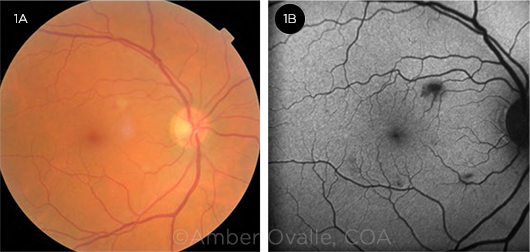
Exam findings. On examination, the patient’s best-corrected visual acuity was 20/25+1 in the right eye and 20/30 in the left. Her pupils, intraocular pressures, and ocular motility were normal. She had 1+ cells in the anterior chamber and vitreous in both eyes, with vitreous debris in the left eye. Dilated fundus exam of the right eye showed two small lesions that looked like cotton-wool spots (Fig. 1A), along with a small hemorrhage. The remainder of the examination was unremarkable.
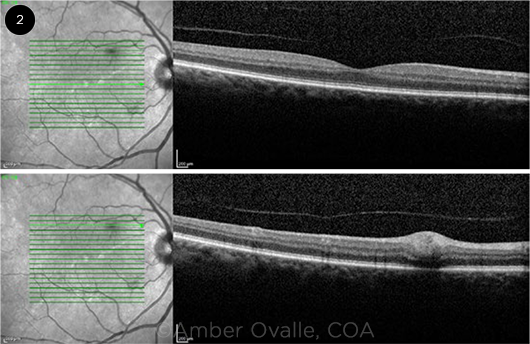
Additional observations. The two small lesions in the right eye caused blockage of fluorescein on angiography (Fig. 1B), and optical coherence tomography localized a hyperreflective lesion to the retinal nerve fiber layer (RNFL, Fig. 2). Apart from the vitreous cells and debris, posterior examination of the left eye was normal.
 |
|
RIGHT EYE. (1A) Cotton-wool spot with a small hemorrhage located superonasal to the fovea and a second cotton-wool spot inferotemporal to the optic nerve. (1B) The cotton-wool spots seen in Fig. 1A caused blockage of fluorescein on angiography.
|
Differential Diagnosis
Given the presence of 1+ cells bilaterally in the anterior chamber and vitreous, we diagnosed Mrs. Roberts’ ocular disease as a bilateral panuveitis. However, the more intriguing question was the underlying condition. The differential diagnosis for uveitis is long, with a wide range of etiologies, including infectious, systemic autoimmune and inflammatory, and hypersensitivity disorders. Additionally, some cases of uveitis are isolated to the eye.
Infectious etiologies. Infectious causes of uveitis include (but are not limited to) herpesvirus, cytomegalovirus (CMV), Epstein-Barr virus (EBV), toxoplasmosis, HIV, syphilis, Bartonella henselae, tuberculosis, West Nile virus, and Rickettsia species.
Systemic autoimmune and inflammatory causes. Diseases associated with systemic inflammation can also cause uveitis. Some of the common culprits include sarcoidosis, multiple sclerosis, systemic lupus erythematosus, Vogt-Koyanagi-Harada syndrome, and Behçet syndrome.
Hypersensitivity reactions. Certain drugs and drug classes can incite uveitis, including rifabutin, cidofovir, fluoroquinolones, bisphosphonates, and BRAF inhibitors.
Disorders restricted to the eye. A number of conditions that cause uveitis have no extraocular manifestations. These include pars planitis, birdshot chorioretinopathy, and sympathetic ophthalmia.
Neoplastic. Intraocular malignancies including lymphoma/leukemia, melanoma and retinoblastoma can present with signs and symptoms resembling uveitis. These are frequently termed “masquerade syndromes.”
Idiopathic. Even after extensive workup, the etiology for uveitis is never found in many instances. Up to 30% of uveitis cases do not have apparent etiology and are classified as idiopathic.
 |
|
OCT. Swelling of the nerve fiber layer in the right eye is seen on optical coherence tomography.
|
Making the Diagnosis
A careful history and review of systems can aid in narrowing the extensive differential diagnosis for panuveitis. In Mrs. Roberts’ case, the absence of any significant past medical history, including autoimmune disease or prolonged medication use, pointed us away from systemic inflammatory or hypersensitivity etiologies. In addition, her concurrent systemic symptoms suggested an infectious cause, rather than a disorder restricted to the eye, so we tailored our workup toward those conditions in the differential.
Laboratory testing. Before we examined Mrs. Roberts, she was already being worked up for a fever of unknown origin and had undergone a battery of tests. These included complete blood count, metabolic panel, urinalysis, QuantiFERON-TB Gold, antinuclear antibodies, erythrocyte sedimentation rate, rheumatoid factor, lactic dehydrogenase, CMV immunoglobulin M (IgM) and polymerase chain reaction, and creatinine kinase results, all of which were normal.
After we saw her in clinic and established a diagnosis of panuveitis, we recommended additional testing based on our differential, including HIV, syphilis IgG, EBV, and Bartonella serology, all of which were negative. The infectious disease physician recommended a chest, abdomen, and pelvis computed tomography scan, which revealed right thoracic inlet, mediastinal, and right hilar lymphadenopathy, with the largest lymph node measuring 1.5 × 2.6 cm in the right paratracheal region and 1.3 × 2.7 cm in the right lower neck.
Uncovering the cause. The Galveston epidemiology department contacted Mrs. Roberts regarding the possibility of murine typhus because of its endemic nature in this part of the country, her exposure to cats (and therefore fleas), and her neighbor with similar symptoms. She was finally tested for Rickettsia typhi, for which she had positive IgG and IgM titers.
Treatment
Mrs. Roberts was treated with doxycycline 100 mg every 12 hours for seven days. About two weeks after she started treatment, her symptoms resolved; she no longer had fever, malaise, or floaters, and she began to regain the weight she had lost during her illness. The cotton- wool spots and the hemorrhage had also resolved (Fig. 3).
 |
|
RESOLUTION. (3) After treatment with doxycycline, the cotton-wool spots in the right eye resolved.
|
Discussion
Rickettsia typhi is an obligate intracellular organism that causes murine typhus and is typically spread through the feces of infected fleas. Rats, opossums, and even domestic cats are reservoirs for the disease. Murine typhus is especially common in coastal and port cities. In the United States, cases of murine typhus have been reported in central and south central Texas and in Los Angeles and Orange counties in California.1 The disease frequently occurs in epidemics; however, because the symptoms are nonspecific, it is difficult to diagnose and is substantially underreported.2 Clinical features of the disease combined with epidemiologic data are key to making the diagnosis, which can be confirmed with serological evidence using indirect immunofluorescence assays.
Systemic involvement. Murine typhus has a six- to 14-day incubation period before the onset of symptoms, which may include high fevers, myalgias, fatigue, and a rash. The rash, if present, is typically located centrally on the trunk. Multiple organ system involvement has been documented, with abnormal lab findings for hematologic, respiratory, hepatic, and renal systems.3
The most common manifestations are fever (96% of patients), headache (75%), and chills (66%), with a rash occurring in slightly over half of cases. Gastrointestinal symptoms may include nausea (48% of patients), vomiting (40%), and diarrhea (21%).2 Although the disease is typically mild, it can lead to hospitalization (10% of patients) and death (4%).4
Ocular findings. The Rickettsia typhi organism has a predilection for vascular endothelium, specifically retinal vessels, which explains its wide array of ocular manifestations.5 Retinal findings that have been described previously include areas of retinal whitening and hemorrhages. There are no apparent choroidal findings on clinical examination, but hypofluorescent dots have been reported on fluorescein angiography and indocyanine green angiography. Optic nerve involvement has also been noted, in the form of optic disc staining, optic edema, or optic neuritis.4 Although the previous literature has not documented changes on optical coherence tomography, this patient’s imaging demonstrates that a swelling of the RNFL may be attributable to murine typhus uveitis (see Fig. 2).
Treatment. Early initiation of antibiotics is crucial and yields better outcomes for patients with severe disease. Treatment is typically initiated empirically based on clinical findings. However, signs and symptoms of the disease can be nonspecific, and results of immunologic testing may take two to three weeks to return.6 Ocular examination can help to provide valuable information for atypical presentations of rickettsial disease while the serologies are pending.
Doxycycline is the drug of choice for rickettsial disease (100 mg twice a day for seven to 10 days). Other tetracyclines can also be effective in treating murine typhus. In children and pregnant patients, macrolides may be used in lieu of tetracyclines.6
___________________________
*Patient name is fictitious.
___________________________
1 Blanton LS et al. Am J Trop Med Hyg. 2016;95(2):457-461.
2 Dumler JS et al. JAMA. 1991;266(10):1365-1370.
3 Azad AF. Annu Rev Entomol. 1990;35:553-569.
4 Khairallah M et al. Br J Ophthalmol. 2009;93(7):938-942.
5 Hudson HL. Int Ophthalmol. 1997;21(3):121-126.
6 Abroug N et al. J Infect Dis Ther. 2014. doi:10.4172/2332-0877.1000140.
___________________________
Mr. Gupta is a medical student, Dr. Lyons is a third-year resident, and Dr. Puthenparambil is a clinical associate professor; all three are at the University of Texas Medical Branch, Galveston. Financial disclosures: None.
Morning Rounds: 2019 in Review
Tackle this year’s medical mysteries. View this article online, where you’ll see links to all the case reports that EyeNet has published so far in 2019.
The Curious Case of Cysts and Sight. After a presumed ocular migraine, the 29-year-old’s vision became hazy (January).
A Case of Pixelated Vision. The 65-year-old insisted that he had a 10%-15% reduction in vision, which he described as pixelated (February).
The Case of Red Eyes and Red Ears. The 57-year-old’s eyes were red, painful, and photophobic; his ears, painful and tender (March).
A Mysterious Eyelid Mass. The 47-year-old noticed an area of fullness in her right upper eyelid. She began to feel uneasy as the mass grew and became readily visible. Then it started feeling tender to the touch (April).
The Case of the Blind Bibliophile. The 64-year-old had experienced a month of rapid decline in vision, followed by gradual deterioration. Five months later, reading was impossible (May).
The Eyelid Lump That Wouldn’t Go Away. The patient was frustrated with his year-old lump that had not responded to topical antibiotics or steroids (June).
The Case of the Double-Edged Protector. The root cause of a surgical oversight (and the swiss cheese metaphor for medical mishaps) (July).
The Horticulturist With Blurry Vision. This horticulturist’s case underscores the importance of a thorough history (August).
The Swollen Eyelid That Kept on Swelling. Despite use of erythromycin ointment, the young boy’s eye became even more swollen and was now painful (September).
The Case of a High School Graduate With a New Blind Spot. The 18-year-old described an egg-shaped black dot just off-center in her right field of view (October).
NEXT MONTH: A Puzzling Pediatric Tumor. The eight-year-old had a painful foreign body sensation in her right eye and, for the previous few weeks, hadn’t been able to see her alarm clock with her left eye. She had a history of accommodative esotropia with 20/20 vision in both eyes.
|